Abstract
Purpose
This randomized double-blind study was designed to determine if respiratory muscle weakness – measured by maximum inspiratory pressure (MIP), maximum expiratory pressure (MEP), forced vital capacity (FVC), and forced expiratory volume in one second (FEV1) – persists even if an acceleromyographic train-of-four ratio (TOFR) of 1.0 is reached after major abdominal surgery.
Methods
Twenty patients underwent respiratory function tests before induction of anesthesia. Rocuronium was given, and the tests were repeated after extubation when the TOFR reached 1.0. The patients were then randomized to receive sugammadex 1 mg·kg-1 or placebo, and the same tests were repeated five and 20 min later. Between-group comparisons were carried out with a mixed-model analysis of variance analysis.
Results
After anesthesia and adequate epidural analgesia, MIP and MEP decreased by 60% in both groups. In the placebo group, MIP decreased from a pre-induction value (median [range]) of 61.8 [31.3-96.1] to 19.6 [8.3-58.3] cm H2O after extubation without significant variation five and 20 min after placebo. In the sugammadex group, MIP decreased from a pre-induction value of 57.8 [13.0-96.4] to 20.5 [6.4-67.3] cm H2O after extubation. No differences were recorded after sugammadex administration (P = 0.246 between groups). In the placebo group, MEP decreased from 88.8 [65.1-120.3] before induction to 37.6 [13.4-70.6] cm H2O after extubation. In the sugammadex group, MEP decreased from 85.5 [58.6-132.7] to 30.8 [10.5-60.5] cm H2O, with no improvement five and 20 min after either placebo or sugammadex administration (P = 0.648). Similarly, the FCV and FEV1 decreased 30-40% after extubation in both study groups.
Conclusion
Acceleromyographic TOFR of 1.0 excludes residual neuromuscular paralysis. However, major respiratory dysfunction is observed after abdominal surgery. This trial was registered at ClinicalTrials.gov: NCT01503840.
Résumé
Objectif
Cette étude randomisée à double insu a été conçue pour déterminer si la faiblesse des muscles respiratoires – mesurée par la pression inspiratoire maximum (PIM), la pression expiratoire maximum (PEM), la capacité vitale forcée (CVF) et le volume expiratoire maximal par seconde (VEMS) – persiste même si un rapport accéléromyographique de train-de-quatre (TOFR) de 1,0 est obtenu après chirurgie abdominale majeure.
Méthodes
Vingt patients ont subi des tests fonctionnels respiratoires avant l’induction de l’anesthésie. Du rocuronium a été administré et les tests ont été répétés après extubation lorsque le TOFR a atteint 1,0. Les patients ont alors été randomisés pour recevoir du sugammadex 1 mg·kg-1 ou le placebo, et les mêmes tests ont été répétés 5 et 20 minutes plus tard. Les comparaisons intergroupes ont été réalisées avec une analyse de modèle mixte d’analyse de la variance.
Résultats
Après une anesthésie et une analgésie péridurale adaptée, la PIM et la PEM a diminué de 60 % dans les deux groupes. Dans le groupe placebo, la PIM a baissé de la valeur avant induction (médiane [extrêmes]) de 61,8 [31,3-96,1] à 19,6 [8,3-58,3] cm H2O après l’extubation sans changement significatif cinq et 20 minutes après le placebo. Dans le groupe sugammadex, la PIM a baissé de la valeur avant induction de 57,8 [13,0-96,4] à 20,5 [6,4-67,3] cm H2O après l’extubation. Aucune différence n’a été enregistrée après l’administration de sugammadex (P = 0,246 entre les groupes). Dans le groupe placebo, la PEM a baissé de 88,8 [65,1-120,3], avant l’induction, à 37,6 [13,4-70,6] cm H2O après l’extubation. Dans le groupe sugammadex, la PEM a baissé de 85,5 [58,6-132,7] à 30,8 [10,5-60,5] cm H2O, sans aucune amélioration cinq et 20 minutes après l’administration de placebo ou de sugammadex (P = 0,648). De même, la CVF et le VEMS ont baissé de 30 % à 40 % après l’extubation dans les deux groupes d’étude.
Conclusion
Un TOFR accéléromyographique de 1,0 exclut une paralysie neuromusculaire résiduelle. Cependant, un trouble fonctionnel respiratoire majeur est observé après chirurgie abdominale. Cette étude a été enregistrée sur le site www.clinicaltrials.gov : NCT01503840.
Similar content being viewed by others
Residual neuromuscular block can cause pulmonary complications following general anesthesia.1 Prolonged major surgery is associated with a high risk of postoperative morbidity and mortality. The risk can be reduced by reversing the effects of neuromuscular blocking agents (NMBAs).2 Acceleromyography-based monitoring is the most widespread method to evaluate neuromuscular blockade. Unfortunately, many anesthesiologists are unaware of this issue and do not monitor neuromuscular activity.3-5 It is generally agreed that an acceleromyographic (AMG) train-of-four ratio (TOFR) of 1.0 represents complete recovery from paralysis.6-8 Compared with mechanomyography – the gold standard for objective neuromuscular monitoring – an AMG TOFR of 1.0 has a negative predictive value of 97% (95% confidence interval 83% to 100%) for detecting residual paralysis.6 Theoretically, then, as many as 17% of patients could have residual weakness at an AMG TOFR of 1.0. To date, no study has investigated the possibility of clinically relevant postoperative residual weakness due to NMBA at an AMG TOFR of 1.0.
The aim of this study was to investigate whether an AMG TOFR of 1.0 reflects respiratory muscle recovery measured by maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP) after anesthesia for major abdominal surgery. This study consisted of two arms to assess the effect of sugammadex, a selective binding agent for rocuronium and vecuronium,9 compared with that of placebo on respiratory function at an AMG TOFR of 1.0. We evaluated respiratory muscular function by measuring MIP and MEP after the AMG TOFR had spontaneously reached 1.0. If muscle weakness was attributable to neuromuscular blockade, we expected the MIP and MEP to improve after sugammadex. If they did not improve, an AMG TOFR of 1.0 would exclude clinically relevant muscular impairment and confirm that this AMG value was reliable for indicating an absence of residual NMBA effect.
Methods
The Independent Ethics Committee of the Fondazione IRCCS Istituto Nazionale dei Tumori of Milan approved the study protocol on October 19, 2011 (protocol INT66-11). It is registered on ClinicalTrials.gov (NCT01503840). This single-center, randomized, double-blind parallel group study enrolled patients (American Society of Anesthesiologists status I-II, age 18-70 yr) who were scheduled for major abdominal surgery (planned to last > 120 min) at the Fondazione IRCCS Istituto Nazionale dei Tumori in Milan between November 2011 and July 2012. Inclusion criteria aimed to select cooperative, non-pregnant patients without known allergies, pulmonary disease, neuromuscular disorders, chronic liver, renal, or cardiac failure. The patients had to weigh > 50 kg and have a body mass index of < 30 kg·m-2. All patients signed the informed consent document.
Measurements
All patients were trained to perform the respiratory tests, repeating each maneuver three to five times on the ward the day before the operation (data not included in the analysis). At enrolment, patients were included only if their MIP and MEP values were above the lower limit of normality10 and the forced expiratory volume after the first second (FEV1) and the FEV1/FVC (forced vital capacity) ratio were, respectively, >70% and > 80% of their predicted values. The MIP and MEP measurements were performed with a mouthpiece connected to a pressure transducer (MPX2010DP® - Freescale Semiconductor Inc.; Austin, TX, USA) as recommended.10 A sampling device (Colligo® - ElektonSas; Agliano, Italy) was used for data recording (100 Hz acquisition). A portable instrument was used for spirometry measurements (SpiroPro® - SensorMedics; Yorba Linda, CA, USA).
Anesthesia
The patients were pre-medicated with 1 mg sublingual lorazepam. All patients underwent the respiratory tests in the operating room before induction of anesthesia. A thoracic epidural catheter was then inserted, and a bolus of 5 mL 0.375% ropivacaine was administered.
Patient monitoring included electrocardiography, pulse oximetry, and invasive blood pressure measurements. General anesthesia was induced with propofol and remifentanil. Neuromuscular function was monitored using evoked acceleromyography of the adductor pollicis muscle (TOF-Watch SX®, Organon, Ireland, now Merck & Co., USA). Pediatric stimulation electrodes were placed on the right forearm along the ulnar nerve. The acceleration transducer was placed in the Hand Adapter® (Organon), and the temperature sensor was fixed to the palmar surface of the same hand. After four to five TOF stimulations at 2 Hz every 15 sec, calibration was performed based on the CAL-2 algorithm. According to this procedure, the initial stimulation current was set at 60 mA, and the T1 (first twitch in the TOF) response was measured. This T1 response was considered to be 100%. The stimulation current was then reduced until the T1 response decreased below 90%. After this step, the current was increased by 10%, and this value (supramaximal current) was used throughout the surgery. The corresponding T1 response was reset at 100%. After this calibration procedure, single-twitch stimulation (1 Hz) was performed for 10 sec. If the T1 value was out of range (95-105%), the calibration was repeated and validated again. When the calibration was adequate, rocuronium 0.6 mg·kg-1 was injected rapidly. Anesthesia was maintained with an inhaled concentration of 3-4% desflurane in an equal mixture of oxygen and air. Additional 5-mL doses of 0.375% ropivacaine were administered epidurally as needed.
The TOF stimulations were performed every two minutes. At T1 reappearance, TOF stimulation was repeated every 15 sec. Rocuronium 0.15 mg·kg-1 was given as soon as the T2 (second twitch in the TOF) was recorded during three consecutive TOF stimulations. On the surgeon’s request, rocuronium 5 mg was administered at closure of the abdominal fascia.
Throughout the procedure, ventilator settings were adjusted to maintain an end-tidal CO2 value of 35-40 mmHg, and positive end-expiratory pressure was set at 5 cm H2O. All patients had a central catheter placed in the right internal jugular vein. The patients were warmed using a forced-air warming blanket and a fluid warmer. Intravenous ketorolac 30 mg and ondansetron 4 mg were administered 45 min before skin closure. Desflurane was stopped at the end of surgery. Spontaneous recovery from neuromuscular block was allowed until the TOFR reached 1.0. If necessary, propofol was administered as a sedative while awaiting neuromuscular recovery. The patients were extubated as soon as possible after the TOFR reached 1.0 for three consecutive TOF stimulations.
Study protocol
Ten minutes after extubation, the respiratory tests that had been performed before induction of anesthesia were repeated. The patients were then randomly assigned to receive either intravenous sugammadex 1 mg·kg-1 or 0.9% sodium chloride as placebo through a central venous catheter. A physician not involved in the respiratory tests performed randomization, preparation, and administration of the reversal agents according to a randomization list provided by the statistics unit of our institution. Respiratory tests were repeated five and 20 min after placebo/sugammadex administration. All patients performed each test twice on a stretcher with the upper body raised (30°). The best measurement of any series was chosen for the analysis.
At the beginning of each step, the patient’s vital parameters, SpO2, and data from arterial blood gas analysis while breathing room air were recorded. Collaboration, pain at rest and on movement, and swallowing ability were also investigated. No specific scale was adopted to evaluate swallowing. We simply asked the patients to indicate if it was impaired. Patient cooperation was classified as follows: poorly collaborative (investigator support needed to perform respiratory tests); collaborative (the patient executed tests alone); very collaborative (the patient actively asked to perform the tests).
Study endpoints
The primary endpoint was MIP and MEP differences between the two groups after placebo/sugammadex administration. The major secondary endpoint was the differences between the two groups concerning FEV1 and FVC after placebo/sugammadex administration. Other secondary endpoints were evaluation of upper airway obstruction defined as the ratio of maximum expiratory flow and maximum inspiratory flow rate at 50% of vital capacity (MEF50/MIF50) > 111,12; ability to swallow; PaO2/FiO2 ratio; and PaCO2 values after reversal administration between the two groups. Upper airway obstruction was also evaluated by calculating another extra-thoracic obstruction index defined as the FEV1/peak expiratory flow (PEF) ratio >10 mL·L-1.min-1.12-14 A chest radiograph was taken after pulmonary function tests in the recovery room. Postoperative pulmonary complications such as atelectasis, pneumonia, respiratory failure, and pulmonary edema were investigated during hospitalization.
Statistical analysis
Based on published data,11 we expected a nearly 40% postoperative FVC decrease and a similar MIP decline after extubation. Considering the average age of our patients, we expected to measure mean MIP values of 70 and 40 cm H2O before and after anesthesia, respectively. The study by Pavlin et al. 15 on the recovery of respiratory muscles after partial neuromuscular blockade in healthy volunteers showed that a 60% MIP reduction is necessary to affect vital capacity. It allowed us to obtain a 15% coefficient of variation as a measure of variability. We estimated that sugammadex could influence MIP values but to a lesser extent in our context. Therefore, we calculated that ten patients per group would provide sufficient power (90%) at a 5% significance level (two-sided t-test) to detect a 25% relative difference in MIP group averages.
Absolute frequencies for categorical variables and medians [range] for continuous variables were used to describe the data. Logarithmic transformation was applied if the distribution of values was not normal. Between-group comparisons were carried out with a mixed-model analysis of variance-type analysis, incorporating the effects of time, treatment, and the time-treatment interaction. With this analysis, a significant result for the time-treatment interaction indicates that the temporal pattern of variation of the investigated variable is different in the two trial arms. The conventional 5% threshold of statistical significance was adopted.
The analyses were carried out using SAS® (version 9.22 – SAS Institute Inc.; Cary, NC, USA). Graphs were drawn with Prism® (version 5.0 - GraphPad Software Inc.; La Jolla, CA, USA).
Results
Of the 22 patients enrolled, two were excluded from the study before randomization (one because of excessive duration of surgery and postoperative intensive care admission; the other for refusing to perform the respiratory tests after extubation). Baseline characteristics were comparable between the two groups (Table 1).
Epidural analgesia provided adequate pain relief. Most patients were very cooperative after extubation (Table 2).
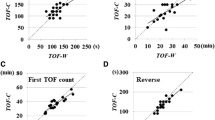
In both groups, the respiratory test values were significantly less at ten minutes after extubation than at pre-induction. They were still significantly lower even 20 min after placebo/sugammadex (Figs. 1 and 2).
Maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP) values measured in the Placebo Group (○ - PBO) and the Sugammadex Group (● - SUG) at four defined times in the study. No differences in the MIP (P = 0.246) and MEP (P = 0.648) measurements were detected over time between the two groups with the mixed-model analysis of variance-type analysis. ○ and ● stand for median; bars stand for range
Forced vital capacity (FVC) and forced expiratory volume after the first second (FEV1) values measured in the Placebo Group (○ - PBO) and the Sugammadex Group (● - SUG) at four defined times in the study. No differences in FVC (P = 0.153) and FEV1 (P = 0.073) measurements were detected over time between the two groups with the mixed-model analysis of variance-type analysis. ○ and ● stand for median; bars stand for range
No differences in the MIP and MEP measurements could be detected between the two groups after extubation or at five and 20 min after placebo/sugammadex administration (P = 0.246 and P = 0.648, respectively – Fig. 1). In the placebo group, the MIP decreased from a median [range] pre-induction value of 61.8 [31.3-96.1] to 19.6 [8.3-58.3] cm H2O after extubation without significant variation at five and 20 min after placebo (18.2 [6.1-73.2] and 25.6 [15.7-61.5] cm H2O, respectively – Fig. 1). In the sugammadex group, the MIP decreased from 57.8 [13.0-96.4] at pre-induction to 20.5 [6.4-67.3] cm H2O after extubation. No differences were observed five and 20 min after sugammadex administration (19.2 [4.0-61.1] and 21.2 [5.0-70.3] cm H2O, respectively – Fig. 1). The pattern was similar for the MEP, which decreased from 88.8 [65.1-120.3] and 85.5 [58.6-132.7] to 37.6 [13.4-70.6] and 30.8 [10.5-60.5] cm H2O after extubation in the placebo and sugammadex groups, respectively. Subsequently, the MEP did not change significantly: 31.8 [21.8-72.5] and 27.3 [3.2-78.6] cm H2O five minutes after reversal and 37 [18.6-67.4] and 28.6 [16.8-79] cm H2O 20 min after placebo and sugammadex, respectively (Fig. 1). Similarly, no differences in the FVC and FEV1 measurements were found between the groups after placebo/sugammadex administration (P = 0.153 and P = 0.073 respectively – Fig. 2). Table 3 reports percent variations of respiratory test measures from pre-induction values in both groups. The median FEV1/FVC ratios were always > 0.7 throughout the protocol steps in both groups (P = 0.086).
The MEF50/MIF50 and FEV1/PEF ratios, which indicate upper airway obstruction, did not differ between the study groups (Fig. 3). One patient (placebo group) reported impaired swallowing at each postoperative measurement despite a MEF50/MIF50 ratio of < 1 throughout the study protocol.
Maximum expiratory flow and maximum inspiratory flow rate at 50% of vital capacity ratio (MEF50/MIF50) and forced expiratory volume after the first second and peak expiratory flow ratio (FEV1/PEF) values measured in the Placebo Group (○ - PBO) and the Sugammadex Group (● - SUG) at four defined times in the study. No differences in the MEF50/MIF50 ratio (P = 0.337) and FEV1/PEF ratio (P = 0.946) were detected over time between the two groups with the mixed-model analysis of variance-type analysis. ○ and ● stand for median; bars stand for range; dotted horizontal lines represent the cutoff values for upper airway obstruction diagnosis (MEF50/MIF50 ratio > 1 and FEV1/PEF ratio > 10 mL·L-1·min-1)
The SpO2, PaO2 and PaCO2 values were within normal ranges for all patients at each protocol step: the PaO2/F i O2 ratio (F i O2 = 0.21) changed from 397 [352-435] to 405 [360-450] and to 382 [345-427] mmHg five and 20 min after placebo, respectively. It also changed from 412 [360-457] to 390 [352-427] and to 390 [345-442] mmHg five and 20 min after sugammadex, respectively.
None of the patients experienced postoperative pulmonary complications.
Discussion
This randomized controlled study evaluated the AMG TOFR value of 1.0 as an indicator of complete respiratory muscle recovery after major abdominal surgery. We hypothesized that if a clinically relevant residual concentration of rocuronium persisted at the neuromuscular junction at an AMG TOFR of 1.0, it would be considered to indicate improved strength of the respiratory muscles after administration of sugammadex. We based our analysis primarily on MIP and MEP measurements, which test respiratory muscle function.10 All tests greatly deteriorated after anesthesia/surgery, but administration of sugammadex did not bring any improvement compared with placebo (Fig. 1).
The observed decrease in postoperative MIP and MEP was greater than expected (about 60% reduction from pre-induction). Moreover, MIP and MEP were affected to a greater extent than the FVC and FEV1 (Table 3). First, this suggests that MIP and MEP are not easy patient maneuvers during the early recovery period. Second, the deterioration might indicate commonly underestimated post-anesthesia muscle impairment revealed by the unusual effort against a blocked mouthpiece. Similar MIP and MEP changes have been described previously up to 48 hours after open cholecystectomy.16
The MIP decreased after anesthesia in both groups to a value of 20-25 cm H2O, which is adequate to ensure a vital capacity of 2 L.15 Indeed, the postoperative FVC values were between 2 and 3 L in both groups; all patients had adequate gas exchange, as suggested by the recorded values for PaO2 and PaCO2. Also, there was no additional benefit from sugammadex administration because there were no differences in the spirometric measurements between the two groups (Fig. 2).
We observed an FVC decrease comparable to the reduction reported by Eikermann et al.11 (extubation at AMG TOFR >0.9) and Kumar et al.17 We measured slightly higher absolute FVC values than Eikermann et al., which could be due to our higher target TOFR (1.0 instead of 0.9) or to the favourable impact of analgesia on postoperative pain and/or patient cooperation. Therefore, our findings agree with literature data that show reduced respiratory reserve that is always present after surgery, even in the absence of residual neuromuscular block.
Our results suggest that post-anesthesia respiratory muscle impairment is attributable to the combined effects of surgery, premedication, hypnotics, and local anesthetics. A combined general-epidural anesthesia technique was chosen to minimize these effects. Epidural analgesia leads to better postoperative lung function.18 Because ropivacaine 0.75% mildly decreases the FEV1 in patients with chronic obstructive pulmonary disease,19 we adopted a concentration of 0.375%, but a slight detrimental effect on the respiratory muscle function cannot be excluded. Some patients required stimulation by physicians to perform the tests, which could have caused a certain degree of functional impairment in these cases. Finally, we did not perform alveolar recruiting maneuvers before extubation. Consequently, we presume that all patients had some degree of functional residual capacity reduction owing to atelectasis that affected their respiratory performance.
Herbstreit et al. reported that a TOFR of 1.0 did not exclude upper airway inspiratory collapsibility in healthy volunteers.20 We did not observe a significant difference between our two groups regarding the upper airway obstruction MEF50/MIF50 index11,12 or swallowing. We observed high MEF50/MIF50 ratios at each protocol step in both groups (Fig. 3), as previously reported.11 High pre-induction values are unexplained, although upper airway obstruction due to benzodiazepine premedication is a possible explanation.21 Probably the MEF50/MIF50 ratio is not appropriate for evaluating upper airway obstruction in this context. When performing a maximum flow-volume loop after the expiratory phase, some patients fail to complete a forced inspiration or sometimes do not seal their lips well around the mouthpiece. In these cases, the MEF50/MIF50 ratio can be overestimated. As a countercheck, we adopted the FEV1/PEF ratio as a secondary index of upper airway obstruction.12-14 This ratio, based on measurements made during expiration, resulted in values indicating less upper airway obstruction (Fig. 3). These inconsistencies between indices of upper airway obstruction suggest that this diagnosis, based on spirometric measures, is difficult during the early post-extubation period.
Interestingly, the time to recovery of the AMG TOFR from 0.9 to 1.0 was extremely variable in both groups (ranging from 120 to 840 sec). This variability indicated that rocuronium inter-compartmental clearance and elimination are still slow at a TOFR ≥ 0.9 in some patients, prolonging the time to complete neuromuscular recovery. Unfortunately, no study has investigated if there is a significant difference in pulmonary function between AMG TOFR of 0.9 and AMG TOFR of 1.0 at extubation.
Study limitations
There were some limitations in this study. We did not have a complete stabilization period before AMG calibration.22 We adopted a simple calibration procedure without normalization of the TOFR at the end of surgery because we aimed to evaluate the reliability of the information resulting from AMG as used in daily practice.
A sugammadex dose of 1 mg·kg-1 is not standard. However, at a TOFR of 1.0, this dose is likely appropriate because sugammadex doses of 0.22 and 1 mg·kg-1 have been reported to reverse TOFRs of 0.5 and a threshold TOF count of four within five minutes, respectively.23,24
It is recommended that respiratory tests be performed at least three times.25 Our patients were asked to do them only twice at each protocol step because they had to support the effort of each test (MIP, MEP, and spirometry) three times during the first 30 min after extubation. Respiratory tests were performed 12-25 min after the AMG TOFR reached 1.0. Hence, we tested the patients at a supposed TOFR > 1.0.
Finally, this study was based on a small number of patients. However, we observed a smaller coefficient of variation of postoperative FVC values (33.8% and 38.8% in the placebo and sugammadex groups, respectively) compared with recent data (45.8%) in a sample of 111 patients without residual neuromuscular weakness.17 Thus, despite our small sample size, we consider our data reliable.
In conclusion, this pilot study suggests that an AMG TOFR of 1.0 excludes residual neuromuscular blockade after major abdominal surgery. At an AMG TOFR of 1.0, additional sugammadex at a dosage of 1 mg·kg-1 does not seem to improve respiratory function. A larger study could investigate whether there is a small degree of residual blockade at an AMG TOFR of 1.0. However, even if there is some residual blockade, it is probably irrelevant clinically. After neuromuscular recovery, many factors cause postoperative respiratory impairment. In fact, during the first hour after extubation this impairment is characterized by a nearly 60% reduction in MIP and MEP and 30-40% reduction in FVC and FEV1.
References
Murphy GS, Szokol JW, Marymont JH, Greenberg SB, Avram MJ, Vender JS. Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesth Analg 2008; 107: 130-7.
Arbous MS, Meursing AE, van Kleef JW, et al. Impact of anesthesia management characteristics on severe morbidity and mortality. Anesthesiology 2005; 102: 257-68.
Grayling M, Sweeney BP. Recovery from neuromuscular blockade: a survey of practice. Anaesthesia 2007; 62: 806-9.
Fuchs-Buder T, Fink H, Hofmockel R, Geldner G, Ulm K, Blobner M. Application of neuromuscular monitoring in Germany (German). Anaesthesist 2008; 57: 908-14.
Della Rocca G, Iannuccelli F, Pompei L, Pietropaoli P, Reale C, Di Marco P. Neuromuscular block in Italy: a survey of current management. Minerva Anestesiol 2012; 78: 767-73.
Capron F, Alla F, Hottier C, Meistelman C, Fuchs-Buder T. Can acceleromyography detect low levels of residual paralysis? A probability approach to detect a mechanomyographic train-of-four ratio of 0.9. Anesthesiology 2004; 100: 1119-24.
Claudius C, Skovgaard LT, Viby-Morgensen J. Is the performance of acceleromyography improved with preload and normalization? A comparison with mechanomyography. Anesthesiology 2009; 110: 1261-70.
Plaud B, Debaene B, Donati F, Marty J. Residual paralysis after emergence from anesthesia. Anesthesiology 2010; 112: 1013-22.
Rex C, Bergner UA, Puhringer FK. Sugammadex: a selective relaxant-binding agent providing rapid reversal. Curr Opin Anaesthesiol 2010; 23: 461-5.
Evans JA, Whitelaw WA. The assessment of maximal respiratory mouth pressures in adults. Respir Care 2009; 54: 1348-59.
Eikermann M, Blobner M, Groeben H, et al. Postoperative upper airway obstruction after recovery of the train of four ratio of the adductor pollicis muscle from neuromuscular blockade. Anesth Analg 2006; 102: 937-42.
Rotman HH, Liss HP, Weg JG. Diagnosis of upper airway obstruction by pulmonary function testing. Chest 1975; 68: 796-9.
Empey DW. Assessment of upper airways obstruction. Br Med J 1972; 3: 503-5.
Mellisant CF, Van Noord JA, Van de Woestijne KP, Demedts M. Comparison of dynamic lung function indices during forced and quit breathing in upper airway obstruction, asthma, and emphysema. Chest 1990; 98: 77-83.
Pavlin EG, Holle RH, Schoene RB. Recovery of airway protection compared with ventilation in humans after paralysis with curare. Anesthesiology 1989; 70: 381-5.
Rovina N, Bouros D, Tzanakis N, et al. Effects of laparoscopic cholecystectomy on global respiratory muscle strength. Am J Respir Crit Care Med 1996; 153: 458-61.
Kumar GV, Nair AP, Murthy HS, Jalaja KR, Ramachandra K, Paremeshwara G. Residual neuromuscular blockade affects postoperative pulmonary function. Anesthesiology 2012; 117: 1234-44.
Groeben H. Epidural anesthesia and pulmonary function. J Anesth 2006; 20: 290-9.
Groeben H, Schafer B, Pavlakovic G, Silvanus MT, Peters J. Lung function under thoracic segmental epidural anesthesia with ropivacaine or bupivacaine in patients with severe obstructive pulmonary disease undergoing breast surgery. Anesthesiology 2002; 96: 536-41.
Herbstreit F, Peters J, Eikermann M. Impaired upper airway integrity by residual neuromuscular blockade. Increased airway collapsibility and blunted genioglossus muscle activity in response to negative pharyngeal pressure. Anesthesiology 2009; 110: 1253-60.
Litman RS, Hayes JL, Basco MG, Schwartz AR, Bailey PL, Ward D. Use of dynamic negative pressure (DNAP) to assess sedative-induced upper airway obstruction. Anesthesiology 2002; 96: 342-5.
Fuchs-Buder T, Claudius C. Skovgaard LT, Eriksson LI, Mirakhur RK, Viby-Mogensen J; 8 th International Neuromuscular Meeting. Good clinical research practice in pharmacodynamic studies of neuromuscular blocking agents II: the Stockolm revision. Acta Anaesthesiol Scand 2007; 51: 789-808.
Schaller SJ, Fink H, Ulm K, Blobner M. Sugammadex and neostigmine dose-finding study for reversal of shallow residual neuromuscular block. Anesthesiology 2010; 113: 1054-60.
Pongracz A, Szatmari S, Nemes R, Fulesdi B, Tassonyi E. Reversal of neuromuscular blockade with sugammadex at the reappearence of four twitches to train-of-four stimulation. Anesthesiology 2013; 119: 36-42.
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319-38.
Acknowledgements
The authors thank Dr. Alessandra Busia of the Respiratory Medicine Unit and anesthesiologist colleagues of the Anesthesia Unit of the Fondazione IRCCS Istituto Nazionale dei Tumori who supported and collaborated on this study. The authors thank Paolo Cadringher of the Department of Pathophysiology and Transplantation of the University of Milan (Italy) for his technical support. The authors also thank Silvia Pedrotti, Ph.D. for linguistic revision of this manuscript.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was designed and conducted by the Department of Anesthesia, Intensive Care and Palliative Care, Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, Italy. This research was financed by institutional and departmental sources. Dr. F. Piccioni has received payments from MSD Italia Srl for consultancy works and for participating in educational events. Other authors have no conflicts of interest. The study is classified as ClinicalTrials.gov number: NCT01503840.
Author contributions
Federico Piccioni, Martin Langer and Luigi Mariani participated in the study design. Federico Piccioni, Lucia Bogno, Giulia T.A. Tramontano, Ilaria Rivetti, Marco Carbonara, and Mario Ammatuna contributed to the data collection. Luigi Mariani performed the statistical analysis. All authors analyzed and discussed the data. Federico Piccioni and Martin Langer drafted the manuscript. All authors have read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Piccioni, F., Mariani, L., Bogno, L. et al. An acceleromyographic train-of-four ratio of 1.0 reliably excludes respiratory muscle weakness after major abdominal surgery: a randomized double-blind study. Can J Anesth/J Can Anesth 61, 641–649 (2014). https://doi.org/10.1007/s12630-014-0160-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0160-7