Abstract
Background
Anesthesia for rigid bronchoscopic procedures is a demanding procedure. Automatic titration of propofol and remifentanil to maintain the bispectral index (BIS) within the recommended range (40-60) has been reported during routine surgical procedures. The aim of the present study was to evaluate its use during rigid bronchoscopy.
Methods
Patients were enrolled in a randomized study comparing manual target-controlled infusion of propofol and remifentanil (manual TCI group) with automatic titration guided by the BIS (dual-loop group). Categorical variables were compared by the Fisher’s exact test, and continuous variables (median [interquartile range 25-75]) were compared by the Mann-Whitney test.
Results
Thirty-four patients were included in the manual TCI group and 33 were included in the dual-loop group. Baseline characteristics were well balanced between the groups. Intervention by the anesthesiologist in charge to modify propofol and/or remifentanil targets in the dual-loop group was not necessary. Percentage of time spent in the BIS interval (40-60) was similar in the manual TCI and dual-loop groups (69% [48-79] vs 70% [58-80], respectively). Durations of induction and of maintenance and propofol and remifentanil doses were also similar between groups, except for the amount of propofol needed for induction (P = 0.002). Time to tracheal extubation was also similar. No case of intraoperational awareness was detected.
Conclusion
The present study could not establish the superiority of automatic system over manual adjustment for bronchoscopy. Further studies with a different design and a larger number of patients are required to establish the place of automatic delivery of anesthetic agents. This study was registered at ClinicalTrials.gov number, NCT00571181.
Résumé
Contexte
L’anesthésie peut être difficile à réaliser lors des bronchoscopies rigides. L’ajustement automatique du propofol et du rémifentanil pour maintenir l’indice bispectral (BIS) dans la plage recommandée (40-60) a été décrit pendant des interventions chirurgicales de routine. L’objectif de cette étude était d’évaluer son utilisation pendant une bronchoscopie rigide.
Méthode
Des patients ont été recrutés pour une étude randomisée comparant une anesthésie intraveineuse à objectif de concentration manuelle associant propofol et rémifentanil (groupe AIVOC manuelle) à un ajustement automatique selon le BIS (groupe double boucle). Les variables catégoriques ont été comparées en utilisant le test exact de Fisher, et les variables continues (moyenne [écart interquartile 25-75]) ont été comparées à l’aide du test de Mann-Whitney.
Résultats
Trente-quatre patients ont été inclus dans le groupe AIVOC manuelle et 33 dans le groupe double boucle. Les caractéristiques de base étaient bien équilibrées entre les groupes. Aucune intervention de l’anesthésiologiste en charge n’a été nécessaire dans le groupe double boucle pour modifier les cibles de propofol et/ou de rémifentanil. Le pourcentage de temps passé dans l’intervalle de BIS (40-60) était semblable dans les groupes AIVOC manuelle et double boucle (69 % [48-79] vs. 70 % [58-80], respectivement). La durée de l’induction et les doses de maintien du propofol et du rémifentanil étaient également semblables dans les deux groupes, à l’exception de la quantité de propofol nécessaire à l’induction (P = 0,002). Le temps jusqu’à l’extubation trachéale était également semblable. Aucun cas de conscience peropératoire n’a été détecté.
Conclusion
Cette étude n’a pas pu établir la supériorité d’un système automatique d’administration de l’anesthésie par rapport à un ajustement manuel pour la bronchoscopie. D’autres études avec une méthodologie différente et un nombre plus important de patients sont nécessaires pour déterminer le rôle des systèmes de distribution automatique d’agents anesthésiques. Cette étude a été enregistrée au numéro ClinicalTrials.gov NCT00571181.
Similar content being viewed by others
Total intravenous anesthesia is an option among various anesthetic techniques for rigid bronchoscopic procedures,1 but Bould et al. showed how difficult it is to obtain the adequate depth of anesthesia as defined by a bispectral index (BIS) of 40-60.2 Recently, we described a controller that appears to be effective for anesthetic induction and maintenance during common surgical procedures.3 Rigid bronchoscopy is a particularly challenging procedure. It involves the management of high-risk patients with central airway obstruction and often major comorbidities, an unpredictable duration, the introduction and mobilization of a rigid bronchoscope (sometimes with several intubations), and use of jet ventilation. The hypothesis of the present study was that automatic delivery of anesthetic drugs would increase the percentage of time of adequate depth of anesthesia by 20% compared with manual delivery. Therefore, this randomized study compared manual target-controlled infusion (manual TCI group) of propofol and remifentanil with automatic titration of the same drugs guided solely by the BIS (dual-loop group) during interventional rigid bronchoscopy.
Methods
The Ethics Committee (Comité de Protection des Personnes Ile de France VIII, N° 070644, 2007) approved this randomized study on July 2, 2007. The patients gave their written informed consent prior to the surgery. The study was conducted in a single university hospital (Hôpital Foch, Suresnes France) from February to June 2008. Male and female participants aged 18-90 yr were eligible. Exclusion criteria included patients presenting psychiatric, supraspinal, or neurological disorders; those equipped with a pacemaker, due to possible interference with BIS monitoring; and pregnant women. Eligible patients were assigned by random number generation in a 1:1 ratio to either the manual TCI or the dual-loop group.
Two anesthesiologists (O.P. and J.E.L.), both experienced in the use of total intravenous anesthesia and the closed-loop system, performed the procedures. They were instructed to compete with the system. They connected an intravenous cannula, dedicated to TCI infusion, to the pumps via a three-way SmartSite® Needle-Free System (Alaris Medical Systems, San Diego, CA, USA) with a priming volume of 0.3 mL. Routine monitoring (pulse oximetry, electrocardiography, and noninvasive blood pressure) was started (monitor GE Datex-Ohmeda S/5™, Helsinki, Finland). The BIS electrode was positioned on the patient’s forehead and the M-BIS Module (version 4.0 GE Datex-Ohmeda, Helsinki, Finland) was used for recording. The impedance of the BIS electrode was checked as being lower than 5 kΩ and the BIS sampling rate was verified at 256 Hz before recording was starting.
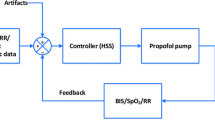
Infusion ToolBox 95® software (Department of Computer Science, Faculty of Medicine, Free University of Brussels, Brussels, Belgium) was used in both groups to deliver TCI of propofol and remifentanil4 using the pharmacokinetic models of Schnider5 and Minto,6 respectively. The investigators’ instructions for the manual group required titration of propofol and remifentanil infusions to obtain a BIS value of 40-60 (BIS40-60), and the goal for the dual-loop group was the same for the controller.3 Briefly, the controller has a cascade structure, including a dual proportional-integral-derivative algorithm and a target-controlled infusion system for the administration of propofol and remifentanil. Every five seconds, it calculates the BISerror, i.e., the difference between the measured BIS and the set point (BIS = 50). If BISerror is different from 0, the controller calculates new propofol and/or remifentanil effect-site concentrations using the pharmacokinetic models of Schnider5 and Minto6 with the demographic variables of the patient (sex, weight, and height). The error size determines which drug will be modified; a small error leads to a change of remifentanil target only, and a large error leads to a concentration change of both drugs (propofol and remifentanil). The minimal interval between two consecutive controls is set equal to the time to peak effect of each drug. Since this time interval is shorter for remifentanil than for propofol, remifentanil modifications are performed more frequently than propofol modifications. The system automatically maintains the calculated drug concentrations in the case of controller or BIS dysfunction or low signal quality index. Furthermore, during maintenance, minimum and maximum values (default values) of concentrations are set at 1.3 and 5 μg·mL−1, respectively, for propofol and at 3 and 12 ng·mL−1, respectively, for remifentanil. The anesthesiologist in charge can modify these values without limits and can also modify the propofol or remifentanil target concentrations at any time if s/he judges it necessary (inadequate antinociception or hypnosis). A detailed description of the controller can be found in the Appendix of a recently published article.3
To facilitate rigid bronchoscopy, all patients received mivacurium, which the anesthesiologist in charge titrated according to the train-of-four response and expected duration of the procedure. High-frequency jet ventilation (Monsoon ventilator, Acutronic Medical Systems AG, Switzerland) was applied through the lateral port of the rigid bronchoscope with the following settings: 100% oxygen, frequency 60-300 breaths·min−1, inspiratory/expiratory ratio 20-30%, and driving pressure three bars.
Other than administration of study drugs, patient management was at the discretion of the treating physician based on current standards of care. The final mivacurium dose was administered 15 min before the expected end of the procedure. Propofol and remifentanil infusions were stopped when four twitches were seen following train-of-four stimulation; the bronchoscope was then removed when spontaneous ventilation had returned. The patient was transferred to the postanesthesia care unit (PACU) with high-flow oxygen inhaled through a face mask.
In the PACU and on the day following the procedure, we visited and interviewed all patients regarding intraoperative recall to seek possible intraoperative explicit awareness with a standardized questionnaire.7
Data recording
Every five seconds, the Infusion ToolBox 95 software recorded the total dose of propofol and remifentanil infused and the BIS values. For purposes of analysis, the anesthetic was divided into three phases:
-
1.
The induction period was defined as the time from the start of propofol administration to the moment when the BIS value decreased to < 60 and remained below that value for at least 30 sec.
-
2.
The maintenance period began at the fourth minute after BIS reached a value < 60 and ended when the propofol and remifentanil infusions were stopped.
-
3.
The emergence period started when the propofol and remifentanil infusions were interrupted and ended with the removal of the bronchoscope.
Outcomes
The primary outcome was the time spent with adequate anesthesia, defined by a BIS value of 40-60, expressed as a percentage of time during the maintenance period. Additional secondary outcomes included duration of the induction period; the occurrence of burst suppression ratio (defined by a suppression ratio > 10% during more than one minute); drug consumption; time to tracheal extubation (defined as the time from discontinuation of propofol and remifentanil infusions until tracheal extubation); hemodynamic abnormalities, assessed by the requirement for ephedrine or an antihypertensive drug; and the incidence of intraoperative awareness in each group. Furthermore, the accuracy of the system was validated using the parameters proposed by Varvel et al. 8: performance error (PE) calculates the difference between actual and desired values; bias or median PE describes the measured values either above or below the target (undershoot or overshoot); inaccuracy or median absolute performance error (MDAPE) describes the size of the errors; and wobble measures the intra-individual variability in PE. We calculated another parameter, namely, the global score (GS), which characterizes the overall performance of the system. GS = (MDAPE + Wobble) / % of time BIS value is 40-60.
Excellent performance is characterized by low MDAPE and wobble values, a high percentage of BIS values from 40-60, and, consequently, a low GS value.9
Statistical analysis
In a pilot study performed during routine bronchoscopic procedures performed under manual administration of anesthetic drugs, the mean (SD) percentage of time with adequate anesthesia was 55 (12)% during the maintenance period. We calculated 26 per group as the number of participants necessary to detect a 20% (relative) improvement in the time with adequate anesthesia, assuming an alpha error of 5% and a beta error of 10%. We planned to recruit 35 patients per group to allow for patients who drop out.
Categorical variables, expressed as numbers and frequencies, were compared using Fisher’s exact test. Continuous variables, expressed as median [interquartile range 25-75], were compared by means of the Mann-Whitney test. P values < 0.05 were considered significant. All reported P values are two-sided. Data analysis was performed using SPSS® version 11.0 (SPSS Science Inc., Chicago, IL, USA).
Results
Seventy patients were included, 35 in each group. Three patients were excluded for prolonged absence of BIS signal (one patient) and incomplete data collection (two patients). The analysis thus relates to 34 patients in the manual TCI group and 33 patients in the dual-loop group.
Baseline characteristics of the population are shown in Table 1. All baseline characteristics were well balanced between groups. More than one-half of the studied population was American Society of Anesthesiologists physical status III or IV. The automated system performed the anesthetic induction and maintenance in all 33 patients of the dual-loop group without any modification of propofol and/or remifentanil targets by the anesthesiologist in charge.
Individual BIS data, BIS median values, and 10th and 90th BIS value percentiles are presented in the Figure. The target BIS value (40-60) was attained 69% [48-79] of the time during the maintenance period in the manual TCI group and 70% [58-80] of the time in the dual-loop group (P = 0.81). Times with BIS < 40, BIS > 60, and with burst suppression ratio > 10% were similar between groups. All control performance parameters were similar between groups (Table 2).
Bispectral index (BIS) values recorded in the dual-loop and the manual TCI groups during the first 30 min of anesthesia. A. Data from all patients are shown; data are averaged for graphical representation with a moving average filter of one-minute duration. B. Median BIS values (thick line) are presented with 10th and 90th percentiles (fine line). C. Number of cases still anesthetized at each time. Manual TCI group = manual target-control infusion group guided by the bispectral index; dual-loop group = closed-loop control of propofol and remifentanil
Drug dosages were similar between groups, except for the dose of propofol required for induction of anesthesia (P = 0.002) (Table 3). Durations of induction (Table 3) and of maintenance (Table 4) were similar in the two groups. Modifications of target concentrations for propofol and remifentanil were more frequent in the dual-loop group (P = 0.008 for propofol and P < 0.0001 for remifentanil) (Table 4). No patient required reversal of neuromuscular blockade. The awakening time (time to tracheal extubation) was similar in both groups (Table 3). No case of intraoperative awareness was detected.
Discussion
This study shows that automatic and manual controls gave the same overall results regarding maintenance of BIS in the adequate range during rigid bronchoscopic procedures.
As outlined by Conacher1 in a review on anesthesia and tracheobronchial stenting for central airway obstruction, the anesthetic agents used during bronchoscopy have changed: propofol is now used instead of etomidate, and more recently, remifentanil has replaced alfentanil. Nevertheless, Conacher did not mention a major trend in anesthetic management, namely, delivery of hypnotic agents according to a measure of anesthetic depth.10 Among all monitors of depth of anesthesia, the BIS monitor has been studied most extensively and remains the most popular. A BIS value in the range 40-60 is considered by the manufacturer to correspond with an adequate anesthetic level,11 and using the BIS monitor during rigid bronchoscopic procedures could reduce the risk of awareness by a factor of 5.12 Then again, in an observational study of patients during routine anesthesia for rigid bronchoscopy, Bould et al.2 reported that BIS values were found to be in the range 40-60 for only 0.5% of the time. To explain their findings, these authors used various anesthetic agents (ten different methods), a clinical underestimation of the depth of anesthesia, and an involuntary modification of the anesthesiologists’ practice. There could have been a higher delivery of anesthetic than usual, as they knew that patients would be interviewed postoperatively to determine explicit recall.
In the present study, performances of the dual-loop system and manual TCI administration were similar regarding the time spent in adequate anesthesia (BIS40-60) with a similar awakening time. One point must be emphasized, i.e., the dual-loop system does not work as well during bronchoscopic procedures than it does during routine anesthetic procedures. We report in the present study that BIS was maintained in the range 40-60 during 70% [58-80] of the maintenance period in the dual-loop group; however, in our previous multicentre study of 196 surgical patients, BIS was maintained during 82 (12)% of the maintenance period.3 This observation can be explained by the unique characteristics of anesthesia for rigid bronchoscopic procedures, in particular, a short duration of maintenance (four times less than for routine surgical procedures), and electroencephalogram artefacts caused by inadequate neuromuscular blockade.13
The dual-loop system and the manual TCI administration performed similarly in the present study with respect to time spent under adequate anesthesia (BIS40-60), emergence time, and precision of the system, as estimated by the parameters proposed by Varvel et al. 8 and by the GS, a novel index proposed by our group.9 The median GS in the manual group was 37 in the present study, while it was 26 in our previous study performed in routine care.3 Automatic systems for the delivery of anesthetic drugs are still far from perfect, as they do not keep the BIS within the desired range anywhere near 100% of the time. There are many paths to improve such a system, including changes to the settings of the actual algorithm; choice of another monitor of depth of anesthesia with a shorter delay of response; introduction of another monitoring tool to monitor analgesia; or a completely different algorithm for the administration of remifentanil, as proposed by Hemmerling et al. with the Analgoscore™.14
A bias is inevitable in this type of study (“man-machine challenge”) due to the Hawthorne effect, i.e., a psychological phenomenon that produces an improvement in human performance as a result of increased attention.15 In daily use, the number of target modifications would probably have been lower than during the study, and this bias benefits the control group. As suggested by Conacher,1 we replaced succinylcholine with mivacurium. It is of great interest to emphasize that succinylcholine could interfere with the anesthetic management because initial myoclonus and later reappearance of muscle activity could be responsible for an increase in electromyographic activity as this signal overlaps the BIS algorithm’s beta ratio in the 30-47-Hz range.16 Such abrupt increases in BIS are misinterpreted as a period of awakening and treated with a bolus anesthetic dose, especially when anesthesia is automated.
In conclusion, BIS can be maintained in the desired range during rigid bronchoscopic procedures with equal success using either an automatic delivery system of propofol and remifentanil or manual TCI. A further study with a different design is required to determine the appropriate place for automatic delivery of anesthetic agents during demanding procedures such as rigid bronchoscopy. Furthermore, other studies with a larger number of patients are required to determine the value and safety of such a system.
References
Conacher ID. Anaesthesia and tracheobronchial stenting for central airway obstruction in adults. Br J Anaesth 2003; 90: 367-74.
Bould MD, Mahtani DG, Davies R, Roughton M, Hunter DN, Kelleher A. Bispectral index values during elective rigid bronchoscopy: a prospective observational pilot study. Anaesthesia 2007; 62: 438-45.
Liu N, Chazot T, Hamada S, et al. Closed-loop coadministration of propofol and remifentanil guided by bispectral index: a randomized multicenter study. Anesth Analg 2011; 112: 546-57.
Cantraine FR, Coussaert EJ. The first object oriented monitor for intravenous anesthesia. J Clin Monit Comput 2000; 16: 3-10.
Schnider TW, Minto CF, Shafer SL, et al. The influence of age on propofol pharmacodynamics. Anesthesiology 1999; 90: 1502-16.
Minto CF, Schnider TW, Egan TD, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology 1997; 86: 10-23.
Leclerc C, Gerard JL, Bricard H. Mémorisation peropératoire. Evaluation de l’incidence chez 326 patients au décours d’une anesthésie générale. Ann Fr Anesth Reanim 2001; 20: 592-9.
Varvel JR, Donoho DL, Shafer SL. Measuring the predictive performance of computer-controlled infusion pumps. J Pharmacokinet Biopharm 1992; 20: 63-94.
Liu N, Chazot T, Genty A, et al. Titration of propofol for anesthetic induction and maintenance guided by the bispectral index: closed-loop versus manual control: a prospective, randomized, multicenter study. Anesthesiology 2006; 104: 686-95.
Moerman N, Bonke B, Oosting J. Awareness and recall during general anesthesia. Facts and feelings. Anesthesiology 1993; 79: 454-64.
Kelley SD. Monitoring Consciousness During Anesthesia & Sedation. A clinician’s Guide to the Bispectral Index®. Aspect Medical Systems, Inc.; 2003.
Myles PS, Leslie K, McNeil J, Forbes A, Chan MT. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet 2004; 363: 1757-63.
Dahaba AA. Different conditions that could result in the bispectral index indicating an incorrect hypnotic state. Anesth Analg 2005; 101: 765-73.
Hemmerling TM, Arbeid E, Wehbe M, Cyr S, Taddei R, Zaouter C. Evaluation of a novel closed-loop total intravenous anaesthesia drug delivery system: a randomized controlled trial. Br J Anaesth 2013; 110: 1031-9.
Franke RH, Kaul JD. The Hawthorne experiments: First statistical interpretation. Am Sociol Rev 1978; 43: 623-43.
Rampil IJ. A primer for EEG signal processing in anesthesia. Anesthesiology 1998; 89: 980-1002.
Acknowledgements
The authors thank Vaincre la Mucoviscidose (Paris, France) for its part in supporting their work and Alaris Medical (Hampshire, UK) for loan of the Asena® GH infusion pumps.
Conflict of interest
Hôpital Foch, N. Liu, T. Chazot, and B. Trillat are patent holders in France for the gain constants and the control algorithm (No. BFF08P669, Institut National de la Propriété Industrielle, France).
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Ngai Liu and Marc Fischler made substantial contributions to the conception and design of the study. Ngai Liu, Thierry Chazot, and Bernard Trillat made substantial contributions to the analysis of data. Ngai Liu and Thierry Chazot made substantial contributions to the interpretation of data. Ngai Liu, Olivier Pruszkowski, Jérôme Erwan Leroy, Thierry Chazot, Bernard Trillat, Arlette Colchen, and François Gonin revised the article. Olivier Pruszkowski, Jérôme Erwan Leroy, Arlette Colchen, and François Gonin made substantial contributions to the acquisition of data. Marc Fischler drafted the article.
Rights and permissions
About this article
Cite this article
Liu, N., Pruszkowski, O., Leroy, J.E. et al. Automatic administration of propofol and remifentanil guided by the bispectral index during rigid bronchoscopic procedures: a randomized trial. Can J Anesth/J Can Anesth 60, 881–887 (2013). https://doi.org/10.1007/s12630-013-9986-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-013-9986-7