Abstract
Purpose
Sore throat after tracheal intubation is common with an incidence of 30-70%. The Parker Flex-Tip™ endotracheal tube (ETT) is designed to reduce trauma during ETT placement. This randomized single-blinded trial was designed to assess whether using the Flex-Tip ETT would reduce the incidence of postoperative sore throat and/or vocal change.
Methods
A Flex-Tip or a Mallinckrodt Hi–Lo® cuffed ETT was used by random allocation in 200 patients with normal-appearing airways requiring elective orotracheal intubation. On the second postoperative day, a blinded assessor recorded the incidence and severity of postoperative sore throat and voice alteration. The primary outcome was the incidence of moderate or severe sore throat. Secondary outcomes included vocal change, time to intubation, number of attempts/failures, incidence of oropharyngeal bleeding, and subjective ease of intubation.
Results
Demographic data were similar between the two groups. Moderate or severe sore throat was observed in 12% of patients with the Flex-Tip ETT and 6% of patients with the Mallinckrodt Hi–Lo ETT (odds ratio [OR] 2.1; 95% confidence intervals [CI] 0.70 to 7.1; P = 0.14). The incidence of moderate or severe vocal change was 6% and 3%, respectively (OR 2.0; 95% CI 0.42 to 12.9; P = 0.50). Time to intubation, number of intubation attempts, incidence of oropharyngeal bleeding, and ease of intubation did not differ significantly between groups.
Conclusion
In this study involving experienced clinicians, no significant difference was observed in the incidence of postoperative sore throat or vocal change between the Flex-Tip ETT and the standard Mallinckrodt Hi-Lo cuffed ETT. This trial was registered at www.clinicaltrials.gov, NCT01095861.
Résumé
Objectif
Avec une incidence de 30-70 %, les maux de gorge sont courants après une intubation trachéale. La sonde trachéale Flex-Tip™ de Parker est conçue de façon à réduire le traumatisme pendant le positionnement de la sonde. Cette étude randomisée à simple insu a été conçue afin de déterminer si l’utilisation de la sonde Flex-Tip serait associée à une incidence réduite de maux de gorge et/ou de changements vocaux postopératoires.
Méthode
Deux-cents patients présentant des voies aériennes d’apparence normale et devant subir une intubation orotrachéale non urgente ont été randomisés à être intubés à l’aide d’un Flex-Tip™ ou d’une sonde à ballonnet Hi–Lo® de Mallinckrodt. L’incidence et la gravité des maux de gorges et les modifications vocales postopératoires ont été enregistrées le deuxième jour postopératoire par un évaluateur en aveugle. Le critère d’évaluation principal était l’incidence de maux de gorge modérés à graves. Les critères d’évaluation secondaires comprenaient les changements vocaux, le temps jusqu’à intubation, le nombre de tentatives et d’échecs, l’incidence de saignements oropharyngés et la facilité subjective d’intubation.
Résultats
Les données démographiques étaient semblables dans les deux groupes. Des maux de gorge modérés à graves ont été observés chez 12 % des patients avec la sonde Flex-Tip™ et 6 % avec la sonde Hi-Lo® de Mallinckrodt (rapport de cotes [RC] 2,1, intervalles de confiance [IC] 95 % 0,70 – 7,1; P = 0,14). L’incidence de changements vocaux modérés à graves était de 6 % et 3 %, respectivement (RC 2,0; IC 95 % 0,42 – 12,9; P = 0,50). Aucune différence significative quant au temps jusqu’à intubation, au nombre de tentatives d’intubation, à l’incidence de saignements oropharyngés et à la facilité d’intubation n’a été observée entre les groupes.
Conclusion
Dans cette étude à laquelle ont participé des cliniciens d’expérience, aucune différence significative n’a été observée au niveau de l’incidence de maux de gorge ou de changements vocaux postopératoires entre la sonde Flex-Tip™ et la sonde à ballonnet standard Hi-Lo® Mallinckrodt. Cette étude a été enregistrée au www.clinicaltrials.gov, NCT01095861.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Unfortunately, sore throat after tracheal intubation is not uncommon.1-4 Although this condition is often considered minor compared with other complications,2 a Cochrane review indicates that its incidence ranges from 30-70% depending on the definition used.1 A non-exhaustive list of risk factors includes endotracheal tube (ETT) size,5-7 duration of intubation,8,9 sex,5,10 cuff design,11 absence of cuff on the ETT,11 cuff pressure,12 and use of nitrous oxide.13 Both technical5,11 and pharmacologic1,14-17 interventions have shown promise for reducing the incidence of this complication.
The Flex-Tip™ (Parker Medical, Highlands Ranch, CO, USA) is a modified ETT made of a softer plastic with a tip designed to be less traumatic upon insertion18 (Fig. 1) than a standard ETT (Fig. 2). It has been shown to facilitate fibreoptic orotracheal intubation in anesthetized patients18 but not in awake subjects,19 and it may also reduce the incidence of trauma associated with nasal intubation.20 This potentially less traumatic ETT could be associated with a reduced incidence of sore throat in the setting of orotracheal intubation using direct laryngoscopy or videolaryngoscopy. A previous study of laryngoscopy and orotracheal intubation involving predominantly novice intubators showed faster intubation using the Flex-Tip but did not demonstrate a reduced incidence of postoperative sore throat.21
The purpose of the present study was to evaluate systematically the potential benefit of the Flex-Tip in reducing complications in clinical practice when intubation is performed by experienced anesthesiologists. This randomized controlled trial (RCT) was undertaken to compare the Flex-Tip and the traditional ETT with respect to the incidence of moderate or severe sore throat and also with respect to vocal change as a secondary outcome.
Methods
This study was carried out from January 2009 to June 2010 at the three teaching hospitals in London, Ontario, Canada. Virtually all surgical specialties were represented within the three hospitals. After obtaining local research ethics board approval, written informed consent was obtained from all patients and operators. English-speaking adult patients who were scheduled for elective surgery requiring orotracheal intubation were invited to participate. Exclusion criteria included an anticipated difficult airway, the need for rapid sequence induction, or pre-existing sore throat. Due to the ETT being evaluated, no cases involving lung isolation or panendoscopy were recruited. Staff anesthesiologists and experienced anesthesiology residents (postgraduate year three or above) were eligible to be operators. The null hypothesis was that there would be no difference in the incidence of moderate or severe postoperative sore throat between the two ETTs. Operators were permitted to use either direct laryngoscopy or videolaryngoscopy.
Operators used the Parker Flex-Tip ETT for patients in the intervention group, and they used the standard local practice – a Mallinckrodt Hi–Lo® ETT (Mallinckrodt Inc., St. Louis, MO, USA) – in the control group. The use of a stylet (Mallinckrodt Satin-Slip™ 14F) was permitted. If a stylet was requested, the operator had to specify the curvature of the stylet prior to randomization. Trimming the length of the ETT was at the discretion of the operator, again specified prior to randomization.
Patient demographics and airway assessment were recorded preoperatively, and the operator specified the ETT size, the trimmed length of the ETT (if applicable), and the requested curvature of the stylet (if used). Each patient was then allocated to a group by a computer-generated random code enclosed within a sealed opaque envelope and opened as the patient entered the operating room. The assigned and unassigned ETTs were prepared remotely by one of the study investigators who concealed the assigned ETT with a towel and then had no further involvement with clinical care or outcome assessment. The unassigned ETT, to be used in the event that the operator was unsuccessful or unhappy with the assigned ETT, was concealed in another towel. To avoid potential bias during positioning, induction, or laryngoscopy, the ETTs were concealed so that the operator would remain blinded until after laryngoscopy had been completed.
To maximise external validity, induction and maintenance of anesthesia were not standardized, but pre-oxygenation was mandated for 5 minutes or an end-tidal oxygen concentration ≥ 80%, and all patients were paralyzed with rocuronium after induction After induction, the patient’s lungs were ventilated until the operator deemed it appropriate to begin intubation, but with a minimum delay of 90 seconds after rocuronium administration.
After the operator completed laryngoscopy and declared the glottic view obtained, the ETT was given to the operator by an assistant, unblinding the operator, and the patient was intubated with the assigned ETT. Operators were permitted to use external laryngeal manipulation to improve the glottic view or to facilitate intubation. If the operator removed the blade or ETT from the patient’s mouth, this was counted as an additional attempt at intubation. If the assigned ETT proved unsuitable or unsatisfying, the operator was permitted to use the other ETT, with or without a stylet, on subsequent attempts. Lubrication of the ETT and application of local anesthetic to the ETT or in the cuff were not employed in this study.
Between 48 and 72 hr after surgery, a third investigator, blinded to group assignment, visited the patient in the hospital or telephoned the patient at home. Reading from a predefined script, this blinded investigator asked the patient if he/she had experienced a sore throat or any vocal change and, if so, to categorize each as mild, moderate, or severe. If vocal change was present, the patient was asked to provide one word that most accurately described the change. Patients with vocal change were followed up to ensure that the symptoms resolved. If vocal change persisted for seven days, the patient was referred to otolaryngology for assessment of potential airway trauma related to tracheal intubation and/or study participation.
The primary outcome was the incidence of postoperative moderate or severe sore throat at any time within the first two postoperative days. Secondary outcomes included: incidence of any vocal change, time to intubation (TTI), ease of intubation (as scored by the operator immediately after laryngoscopy on a 100 mm visual analogue scale [VAS]), number of attempts, and the presence of blood after blind suctioning the oropharynx immediately following intubation.
The TTI was defined as the period of time from the moment the laryngoscope blade first passed the teeth to the appearance of an end-tidal CO2 ≥ 30 mmHg on the anesthesia monitor. After initiating the timer, the blinded observer viewed only the anesthesia monitor and did not observe the ETT being used. If the intubation attempt took > 150 sec or more than three attempts, it would be considered a failure, and then the airway would be managed as deemed appropriate by the attending anesthesiologist. The presence of blood was categorized as none, mild, moderate, or severe. Ventilation between intubation attempts was permitted if deemed appropriate. The TTI was not revealed to the operator until after the data collection sheet, including perceived ease of intubation, had been completed. Patients were extubated according to the attending anesthesiologist’s usual practice.
Surgical procedure duration was retrieved from the hospital’s operating room database to obtain a surrogate of intubation duration. These database entries were created by nurses who were not involved in the study process.
Statistical analysis
For the sample size calculation, the consensus of the investigators was that an absolute 20% decrease in moderate to severe postoperative sore throat would be clinically relevant, using an assumed incidence of 40% and standard type I and type II error rates (α = 0.05, β = 0.20). The calculated sample size was 91 patients per group, and a total sample size of 200 patients was selected to allow for patient dropout or missing data. Stata 11.0 for Mac OS X (StataCorp LP, College Station, TX, USA) was used for all statistical tests and for sample size calculation. The data were analyzed by a statistician blinded to group allocation.
The primary outcome of moderate or severe sore throat and other categorical variables were compared between groups using the Chi square test (if all expected cell counts were ≥ 5) or Fisher’s exact test (if any expected cell counts were < 5). Continuous variables analyzed in the study (TTI and ease of intubation VAS) were anticipated to have non-normal distributions and therefore were described with medians and interquartile ranges (IQR) and analyzed using non-parametric methods (the log-rank test and the Mann Whitney U test, respectively). After adjusting for surgery duration, logistic regression was performed to see if ETT type had any influence on the incidence of moderate or severe sore throat and/or moderate or severe vocal change. There was no correction for multiple comparisons.22 Results were considered statistically significant when P < 0.05.
Results
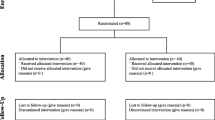
From January 2009 to June 2010, 212 patients were approached to participate in the study. Twelve patients refused; the remaining 200 patients were randomized. Data from these 200 patients were collected and analyzed. There was no crossover; tracheal intubation was performed in all patients with the assigned ETT. Sore throat and vocal change data were not collected for one patient due to death prior to follow-up; the death was unrelated to any study aspect. Baseline demographics and tracheal ETT size were similar between study groups (Table 1).
The results are shown in Table 2 and in Figs. 3 and 4. Moderate or severe sore throat was observed in 12% of Flex-Tip patients and 6% of the control patients (Odds ratio [OR] 2.1; 95% CI, 0.70 to 7.1; P = 0.14). The incidence of moderate or severe vocal change was 6% with Flex-Tip vs 3% in the control group (OR 2.0; 95% CI, 0.42 to 12.9; P = 0.50). The most common words to describe vocal change in the Flex-Tip group were “hoarse” (n = 7) and “dry” (n = 4). “Raspy” and “higher” were used twice; “breaking” was offered once. The most common words to describe vocal change in the control group were “hoarse” (n = 9), “dry” (n = 10), and “raspy” (n = 3); “crackly”, “different”, and “scratchy” were each offered once.
In three patients in the control group and one patient in the Flex-Tip group, tracheal intubation could not be performed within 150 sec. In these four cases, the anesthesiologist elected to ventilate the patients’ lungs with bag and mask prior to re-attempting tracheal intubation, and the assigned ETT was inserted successfully on a subsequent attempt. However, these events were categorized as failed intubation because the duration exceeded the predefined limit of 150 sec.
Two patients experienced vocal change that persisted more than seven days, and they were referred to otolaryngology for assessment. The first patient was in the control group; examination revealed normal anatomy, and the symptoms resolved spontaneously over the next seven days. The second patient, in the Flex-Tip group, suffered recurrent laryngeal nerve transection as a surgical complication (during carotid endarterectomy), and neither the surgeon nor the referred otolaryngologist considered the ETT to be contributory with respect to the etiology of the vocal change.
The median TTI was 28.3 sec, IQR [24-37] sec with the Flex-Tip vs 26.5 sec, IQR [22-33] sec with control (P = 0.27). There was no significant difference between the groups regarding ease of intubation, number of intubation attempts, or incidence of oropharyngeal bleeding (Table 2).
Logistic regression did not demonstrate any difference between groups in the incidence of moderate or severe sore throat (adjusted OR 2.1, 95% CI 0.76–5.9, P = 0.15) and/or moderate or severe vocal change (adjusted OR 2.0, 95% CI 0.49 – 8.3, P = 0.33), after adjusting for surgery duration.
Discussion
In this study of experienced anesthesia practitioners, there was no significant difference in the incidence of postoperative sore throat or vocal change between the two groups. Flex-Tip ETT use did not reduce the incidence of either complication, and, in fact, there was a trend towards an increased incidence of complications in the Flex-Tip group. A total sample size of 708 patients would be required to detect a statistically significant difference between groups, assuming a true incidence of moderate or severe sore throat of 12% and 6% in each group. Over all, both groups experienced a sore throat incidence of approximately 40%, similar to other studies.1,3,4 The incidence of moderate or severe sore throat, the clinically relevant entity in our view, ranged from 6-12%, similar to other groups.
Because of the multifactorial nature1-13 of postoperative sore throat, a study testing an intervention to reduce postoperative sore throat must balance the competing interests of tightly-driven protocols that control known confounders (to reduce variability at the expense of external validity) and less restrictive study arms that mirror common practice (but maximize clinical applicability perhaps with increased variability). This study was designed as a pragmatic RCT that would maximize clinical applicability and employ randomization to ensure a similar distribution of both known and unknown confounders between the intervention and control groups.
The etiology of postoperative sore throat is likely multifactorial.1,4 Postoperative sore throat has been reported not only with ETTs but also with a laryngeal mask airway device3 and even with face mask.3 Thus postoperative sore throat may be related only partially to the ETT itself and/or the perceived trauma18,23 during insertion. This observation is in keeping with the demonstrated lack of correlation between multiple attempts at intubation and sore throat.5,23 The greater influence of other factors could explain the failure of a “less traumatic” tip to confer benefit in this trial.
As might be expected, there was no significant difference in the duration of intubation. Since there was no difference in perceived operator satisfaction, it is reasonable to base choice of ETT on operator preference. The end point of TTI was observation of end-tidal CO2 on the anesthesia monitor, similar to other trials investigating intubation techniques. This was intended to provide a blinded end point. If the TTI had ended at the conclusion of laryngoscopy or at cuff inflation, the observer would have become unblinded and could have biased observations.
A limitation to this trial is that most operators had more prior experience with the (control) Mallinckrodt ETT and may have been more familiar with its use. However, the ETTs are very similar during use, so much so that some operators inquired as to which ETT they had used in the study. Thus, differing experience levels are unlikely to have affected the results. While it is possible that more experience with the Flex-Tip would improve the procedure and/or reduce complications, it is considered unlikely that the improvement would be sufficient to demonstrate superiority over the standard ETT. It could be argued that a new device or technique should be clearly superior to warrant adoption and not just equivalent to the device or technique used currently, especially considering that new devices are usually more expensive than the devices they purport to replace.
Another limitation to this trial is that potential risk factors for sore throat, such as ETT size, cuff pressure, nitrous oxide use, and stylet use were not standardized as part of protocol. It is possible that these confounders or unknown confounders were not distributed evenly between the groups, thus introducing a bias. This possibility is considered unlikely since the operator was required to specify all ETT and stylet parameters prior to randomization.
Another limitation of this trial is that only 6% of the operators chose videolaryngoscopy for laryngoscopy; therefore, the results of this trial may not be applicable to this method of intubation.
Operators were aware that their actions were being timed. This could lead to faster intubation performance via the Hawthorne effect.24 However, the operators were also aware that the primary outcome of the study was the incidence of sore throat, which would be more likely to promote greater care and perhaps slower intubation. Any improvement or deterioration in performance would likely have been distributed equally between the groups – minimizing the impact of this effect.
In summary, in this RCT of 200 patients who were orotracheally intubated by experienced anesthesiologists, the Flex-Tip ETT did not reduce the incidence of moderate or severe sore throat or the secondary outcome of vocal change.
References
Tanaka Y, Nakayama T, Nishimori M, Sato Y, Furuya H. Lidocaine for preventing postoperative sore throat. Cochrane Database Syst Rev 2009; (3): CD004081.
Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg 1999; 89: 652-8.
Higgins PP, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth 2002; 88: 582-4.
McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia 1999; 54: 444-53.
Christensen AM, Willemoes-Larsen H, Lundby L, Jakobsen KB. Postoperative throat complaints after tracheal intubation. Br J Anaesth 1994; 73: 786-7.
Mandoe H, Nikolajsen L, Lintrup U, Jepsen D, Molgaard J. Sore throat after endotracheal intubation. Anesth Analg 1992; 74: 897-900.
Stout DM, Bishop MJ, Dwersteg JF, Cullen BF. Correlation of endotracheal tube size with sore throat and hoarseness following general anesthesia. Anesthesiology 1987; 67: 419-21.
Fowler MA, Spiess BD. Postoperative recovery. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC (Eds). Clinical Anesthesia. 6th ed. Lippincott Williams & Wilkins; 2009: 1438.
Yamanaka H, Hayashi Y, Watanabe Y, Uematu H, Mashimo T. Prolonged hoarseness and arytenoid cartilage dislocation after tracheal intubation. Br J Anaesth 2009; 103(3): 452-5.
Maruyama K, Sakai H, Miyazawa H, et al. Sore throat and hoarseness after total intravenous anaesthesia. Br J Anaesth 2004; 92: 541-3.
Loeser EA, Kaminsky A, Diaz A, Stanley TH, Pace NL. The influence of endotracheal tube cuff design and cuff lubrication on postoperative sore throat. Anesthesiology 1983; 58: 376-9.
Jensen PJ, Hommelgaard P, Sondergaard P, Eriksen S. Sore throat after operation: influence of tracheal intubation, intracuff pressure and type of cuff. Br J Anaesth 1982; 54: 453-7.
Stanley TH. Nitrous oxide and pressures and volumes of high- and low-pressure endotracheal-tube cuffs in intubated patients. Anesthesiology 1975; 42: 637-40.
Ebneshahidi A, Mohseni M. Strepsils(R) tablets reduce sore throat and hoarseness after tracheal intubation. Anesth Analg 2010; 111: 892-4.
Tazeh-Kand NF, Eslami B, Mohammadian K. Inhaled fluticasone propionate reduces postoperative sore throat, cough, and hoarseness. Anesth Analg 2010; 111: 895-8.
Hung NK, Wu CT, Chan SM, et al. Effect on postoperative sore throat of spraying the endotracheal tube cuff with benzydamine hydrochloride, 10% lidocaine, and 2% lidocaine. Anesth Analg 2010; 111: 882-6.
Park SY, Kim SH, Lee SJ, et al. Application of triamcinolone acetonide paste to the endotracheal tube reduces postoperative sore throat: a randomized controlled trial. Can J Anesth 2011; 58: 436-42.
Kristensen MS. The Parker Flex-Tip tube versus a standard tube for fiberoptic orotracheal intubation: a randomized double-blind study. Anesthesiology 2003; 98: 354-8.
Joo HS, Naik VN, Savoldelli GL. Parker Flex-Tip are not superior to polyvinylchloride tracheal tubes for awake fibreoptic intubations. Can J Anesth 2005; 52: 297-301.
Prior S, Heaton J, Jatana KR, Rashid RG. Parker flex-tip and standard-tip endotracheal tubes: a comparison during nasotracheal intubation. Anesth Prog 2010; 57: 18-24.
So M, Sobue K, Arima H, et al. Flexible, tapered-tip tube facilitates conventional orotracheal intubation by novice intubators. J Anesth 2006; 20: 344-7.
Perneger TV. What’s wrong with Bonferroni adjustments. BMJ 1998; 316: 1236-8.
Harding CJ, McVey FK. Interview method affects incidence of postoperative sore throat. Anaesthesia 1987; 42: 1104-7.
Holden JD. Hawthorne effects and research into professional practice. J Eval Clin Pract 2001; 7: 65-70.
Acknowledgement
We gratefully acknowledge the respiratory therapists who assisted with data collection and the surgeons whose patients were involved in this trial.
Disclosure statement
This study was funded internally and all evaluated devices were purchased by the University of Western Ontario, Department of Anesthesia.
Competing interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Turkstra, T.P., Smitheram, A.K., Alabdulhadi, O. et al. The Flex-Tip™ tracheal tube does not reduce the incidence of postoperative sore throat: a randomized controlled trial. Can J Anesth/J Can Anesth 58, 1090–1096 (2011). https://doi.org/10.1007/s12630-011-9592-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-011-9592-5