Abstract
Purpose
Hypotension in the sitting position may reduce cerebral perfusion and oxygenation. We prospectively determined the incidence of cerebral oximetry (rSO2) desaturation in seated patients undergoing ambulatory shoulder arthroscopy.
Methods
A cohort of 99 patients received regional anesthesia and intravenous sedation, and their blood pressure was recorded every five minutes. Hypotension was defined as the occurrence of any of the following: > 30% decline in mean arterial pressure (MAP), systolic blood pressure < 90 mmHg, or MAP <66 mmHg. Cerebral desaturation was defined as a > 20% decrease in rSO2 from baseline. The association of rSO2 desaturation with potential risk factors was examined by the generalized estimating equation to account for within patient correlation and multiple observations per patient. We fitted desaturation with three models: 1) unadjusted (i.e., hypotension as sole regressor); 2) time-trend adjusted; and 3) baseline-factors adjusted model.
Results
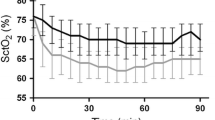
Hypotension occurred in 76% of observations (mean duration 4,261 sec), but cerebral desaturation was seen in only 0.77% of observations (mean duration 426 sec). Ninety-nine percent of patients experienced hypotension, but cerebral desaturation occurred in only 10%. By unadjusted modelling, hypotension was associated with cerebral desaturation (odds ratio = 3.21; P = 0.02). Once time-trend adjusted, cerebral desaturation was associated with time from baseline but not with hypotension (P = 0.14). When adjusted for baseline factors, the analysis demonstrated a non-significant association with hypotension (P = 0.34) but a significant association with the presence of risk factors for cerebrovascular disease (P = 0.01).
Conclusions
Despite frequent hypotension in the sitting position, rSO2 desaturation was uncommon during shoulder arthroscopy performed in the sitting position with regional anesthesia.
Résumé
Objectif
L’hypotension en position assise pourrait réduire la perfusion et l’oxygénation cérébrales. Nous avons déterminé, de façon prospective, l’incidence de désaturation cérébrale (rSO2) chez les patients assis subissant une arthroscopie de l’épaule en ambulatoire.
Méthode
Une cohorte de 99 patients a reçu une anesthésie régionale et une sédation intraveineuse, et leur pression artérielle a été enregistrée toutes les cinq minutes. L’hypotension était définie en tant que la survenue de l’un des évènements suivants: déclin de > 30 % de la tension artérielle moyenne (TAM), tension artérielle systolique < 90 mmHg, ou TAM < 66 mmHg. La désaturation cérébrale a été définie comme une réduction de 20 % de la rSO2 par rapport à la valeur de base. L’association entre la désaturation de la rSO2 et les facteurs de risque potentiels a été examinée par une équation d’estimation généralisée afin de tenir compte de la corrélation chez un même patient et des observations multiples par patient. Nous avons ajusté la désaturation en fonction de trois modèles: 1) modèle non ajusté (c.-à-d. avec l’hypotension comme variable indépendante unique); 2) modèle ajusté en fonction de la tendance temporelle; et 3) modèle ajusté selon les facteurs de base.
Résultats
L’hypotension est survenue dans 76 % des observations (durée moyenne 4 261 sec), mais la désaturation cérébrale n’a été observée que dans 0,77 % des observations (durée moyenne 426 sec). Quatre-vingt-dix-neuf pour cent des patients ont souffert d’hypotension, mais la désaturation cérébrale n’est survenue que chez 10 %. Dans le modèle non ajusté, l’hypotension a été associée à une désaturation cérébrale (rapport de cotes = 3,21; P = 0,02). Lorsque le modèle était ajusté pour tenir compte de la tendance temporelle, la désaturation cérébrale a été associée au temps depuis les mesures de base mais pas à l’hypotension (P = 0,14). Lorsqu’elle était ajustée pour tenir compte des facteurs de base, l’analyse a démontré une association non significative à l’hypotension (P = 0,34) mais une association significative à la présence de facteurs de risques de maladie vasculaire cérébrale (P = 0,01).
Conclusion
Malgré une hypotension fréquente en position assise, la désaturation de rSO2 était peu répandue pendant une arthroscopie de l’épaule réalisée en position assise avec une anesthésie régionale.
Similar content being viewed by others
Controlled hypotension is used during surgical procedures to reduce bleeding and improve visualization,1 but it may impair perfusion of vital organs.2,3 The beach chair or sitting position is often combined with controlled hypotension for shoulder surgery, further increasing the risk of cerebral hypoperfusion.4 Four cases of ischemic central nervous system injury after shoulder surgery in the beach chair position, all performed under general anesthesia, have been attributed to hypoperfusion of the brain due to postural hypotension and/or head and neck manipulation.4 Thus, the risks and benefits of controlled hypotension in the sitting position are currently controversial.Footnote 1 The safe lower limit of hypotension is uncertain.5 In normal subjects, cerebral blood flow is thought to be maintained constant over a mean arterial pressure (MAP) range of 70-150 mmHg, but the validity of this concept has been challenged.6 A MAP of 60 mmHg has been recommended by some as the lower limit of induced hypotension7; however, others suggest not to decrease the systolic blood pressure > 20-30% from baseline (to 80-90 mmHg in normal patients) during controlled hypotension.8
The lack of certain safety limits for controlled hypotension5 suggests that a monitor that directly measures end organ perfusion or a validated surrogate measure may be useful in the sitting position. Cerebral oximetry (rSO2) with near infrared spectroscopy allows estimation of brain tissue oxygenation.9 It has been evaluated as a monitor for cerebral ischemia in multiple clinical settings, and in some instances, it can predict the risk of cognitive decline and length of hospital stay.10-12 At our institution, controlled hypotension in the sitting position is commonly performed for patients undergoing ambulatory shoulder arthroscopy. We prospectively measured blinded rSO2 in patients undergoing ambulatory shoulder arthroscopy in the sitting position to determine the incidence of rSO2 desaturation. As secondary goals, we correlated rSO2 to blood pressure and oxygen saturation by pulse oximetry (SpO2). This observational study was conducted both to document the incidence of cerebral desaturation and to investigate possible correlation between hypotension and cerebral desaturation. One of two likely outcomes was expected; either cerebral desaturation is uncommon and apparently unrelated to hypotension (perhaps due to avoidance of general anesthesia with positive pressure ventilation), or cerebral desaturation is relatively common and appears to be linked to hypotension (which could lead to testing of protocols aimed at reducing the rate of cerebral desaturation).
Methods
Selection and description of participants
After Institutional Board Approval, written informed consent was obtained from 99 patients scheduled to undergo ambulatory arthroscopic shoulder surgery from July 2009 to May 2010. This study was a subset of a larger clinical registry.13 Patients were excluded if general anesthesia or an open shoulder procedure was planned, if the patient had a pre-existing contraindication to regional anesthesia (e.g., infection at block site or pre-existing neurological injury), or if a research assistant was not available to collect data.
Technical information
Patient demographic characteristics were recorded. Standard noninvasive vital signs, including blood pressures measured on the nonoperative upper arm (GE Datex-Ohmeda S5, Beverton, OR, USA), heart rate, and SpO2, were recorded at baseline prior to the nerve block and then every five minutes. Prior to the nerve block, a cerebral oximeter sensor was applied bilaterally on the patient’s forehead according to the manufacturer’s instructions (Invos 5100C Cerebral/Somatic Oximeter, Somanetics Corp, Troy, MI, USA). The clinical team was blinded to ascertainment of rSO2, which was recorded at baseline prior to anesthesia induction and then continuously throughout the procedure. All data were downloaded directly to a laptop after completion of surgery. An ultrasound-guided interscalene or supraclavicular nerve block was performed as the primary anesthetic. Surgery was performed in the sitting beach chair position, and the vertical distance from the patient’s head (external auditory meatus) to the heart (left fourth intercostal space) was measured. Intraoperative sedation was at the discretion of the anesthesia team. The anesthesiologist and surgeon agreed on the endpoints for controlled hypotension individually on an ad hoc basis. The patients were discharged home from the postanesthesia care unit after achieving routine discharge criteria.
Statistics
At the time of the study design, we arbitrarily decided to enroll patients until we obtained useable data for approximately 100 patients. Statistical analysis was planned with descriptive statistics to report incidences of controlled hypotension and low rSO2, and we used three previously recommended definitions of hypotension (MAP > 30% decline from baseline, systolic blood pressure < 90 mmHg, and/or MAP < 66 mmHg).2,3,5 Mean arterial pressure was calculated as MAP = diastolic blood pressure + 1/3 (systolic blood pressure − diastolic blood pressure). In the sitting position, blood pressure measurements from the arm cuff were corrected to the head level with a 1 mmHg reduction in blood pressure for each 1.25 cm of vertical distance from the head to the heart.A Cerebral desaturation was defined as rSO2 decline > 20% from baseline.14
We summarized patient characteristics at baseline using mean and standard deviation (SD) for continuous variables and using frequency and percentage for categorical variables. The incidence of clinical events was estimated by percentages per patient as well as per observation; duration of events was summarized by mean, median, and range. The association of the endpoint (i.e., rSO2 desaturation) with potential risk factors was examined by the generalized estimating equation (GEE). The GEE was used to account for within patient correlation and the different number of observations per patient. We fitted three models: 1) unadjusted model with the single exposure variable of interest (i.e., hypotension); 2) time-trend adjusted model; and 3) baseline multivariables adjusted model. The time-trend adjusted model controlled “time from baseline” as a time-varying covariate, and the baseline multivariables adjusted model controlled “time-independent covariates at baseline”, which are deemed to be clinically relevant but did not control time-trend in the model. Thus, the endpoint, primary exposure (i.e., hypotension), and time variables were time-dependent, while other factors were analyzed as time-independent (i.e., fixed at baseline) variables. Note that we did not employ a statistical technique for variable selection in order to provide comprehensive and fair views of the analysis in the presence of multivariables, and we did not adjust time-dependent covariates which could be affected by the primary exposure in the regression models.
For correlation structure within patient, first-order autoregressive model, i.e., AR(1), was employed. Since the endpoint is binary, parameter estimates are expressed in the log of odds ratio (OR), and standard errors were estimated by the empirical method.
We assumed two-sided hypotheses/tests for all statistical estimation and inference. Calculations were made using SAS® software (version 9.2; SAS Institute Inc., Cary, NC, USA) and SPSS® software (version 14.0.2; SPSS Inc., Chicago, IL, USA).
Results
One hundred twenty-three of 153 eligible patients were enrolled in the study and 99 patients reached completion (Figure). The baseline characteristics of the 99 patients whose data were analyzed are presented in Table 1. Most patients were young to middle aged, healthy, and non-obese. Only 17% had at least one risk factor for cerebrovascular disease, 12% had two risk factors, and none of the patients had three or more risk factors. Every 30 sec, rSO2 measurements were recorded and paired with the most recent blood pressure measurement.
All patients were placed in the sitting position with a mean heart to head vertical distance of 32 cm. Most patients received midazolam and a propofol infusion (Table 2). Some patients received metoprolol, both to counteract the effects of exogenous epinephrine (often included with the nerve block as well as in the arthroscopic irrigation fluid) and to prevent bradycardia mediated by the Bezold-Jarisch reflex.15 Additional hypotensive agents were used as clinically indicated; either labetalol or hydralazine was given based on the patient’s heart rate.
On a per observation basis, hypotension occurred 76% of the time with a mean duration of 4,261 sec, but cerebral desaturation occurred only 0.77% of the time with a mean duration of 426 sec. The median duration of desaturation was 30 sec (one measurement period), indicating that most episodes of desaturation were relatively brief. On a per patient basis, only one patient did not manifest hypotension. The combination of both hypotension and cerebral desaturation occurred in ten patients (Table 3a, b), and the combination of hypotension and cerebral desaturation occurred 129 times out of 18,353 observations (Table 3b).
Table 4 summarizes regression analysis between hypotension (as regressor) and cerebral desaturation (as endpoint), and Tables 4a, 4b, and 4c, present unadjusted, time-adjusted, and multivariable adjusted analyses, respectively. When we crudely modelled hypotension and cerebral desaturation, a positive association between these two events was observed (OR = 3.21; P = 0.02) (Table 4a). However, once time-trend was adjusted, the association between hypotension and cerebral desaturation was not significant (P = 0.14) (Table 4b). In this analysis, an increasing trend toward the occurrence of cerebral desaturation over time was clearly noted (P < 0.0001). When we did not adjust time-trend but adjusted baseline factors at baseline (as fixed covariates), hypotension and cerebral desaturation were still positively associated, but the association was not statistically significant (P = 0.34) (Table 4c) Notably, the presence of risk factors for cerebrovascular disease at baseline was significantly associated with cerebral desaturation (P = 0.01).
Discussion
In the present study, hypotension was observed almost 100 times as often as cerebral desaturation (76% vs 0.77%). Hypotension occurred in 99% of patients undergoing shoulder arthroscopy in the sitting position, but only 10% of patients experienced an episode of cerebral desaturation, defined as a 20% reduction in rSO2 from baseline. Hypotension was associated with cerebral desaturation in the univariate analysis, but the association lost statistical significance with either time-trend adjusted analysis or baseline factors adjusted analysis. The baseline factors adjusted analysis indicated that the presence of one or several risk factors for cerebrovascular disease was significantly associated with cerebral desaturation. Since measurements were repeated over time, a time-trend analysis was completed, and it indicated that cerebral desaturation was more likely to occur later in the procedure. The majority of cerebral desaturation observations occurred with hypotension, so it is difficult to conclude that there is no association (confounding factors may play a role).
Blood pressure was corrected for position, and hypotension was defined as occurrence of any of the following: a reduction of systolic blood pressure to < 90 mmHg, a reduction of MAP to < 66 mmHg, or a > 30% reduction of baseline MAP.2,3 The average lower limit of cerebral autoregulation may be as high as 70 mmHg but has considerable individual variation.6 Below the lower limit of the autoregulatory plateau, cerebral blood flow is reported to be related linearly to cerebral perfusion pressure,16 and controlled hypotension may induce cerebral hypoperfusion. However, despite frequent hypotension, the low incidence of cerebral desaturation (0.77% of time intervals) suggests that adequate cerebral perfusion was generally maintained. Studies show that a poor correlation between blood pressure and measures of cerebral perfusion (such as cerebral oximetry or transcranial Doppler) indicates maintenance of cerebral autoregulation.17
Use of regional anesthesia as the primary anesthetic may have reduced the risk of rSO2 desaturation. In a recent study,18 an 80% incidence of cerebral desaturation was found in patients who underwent surgery in the beach chair position under general anesthesia, but a much lower rate was found in patients who underwent surgery in the lateral position. Although no permanent adverse effects were noted in 61 patients, the high incidence of rSO2 desaturation with general anesthesia is potentially worrisome. Differences in anesthetic management may explain the low rate of cerebral desaturation reported in the current study. Patients in this study were breathing spontaneously while receiving intravenous sedation after a brachial plexus nerve block, whereas in the study by Murphy et al.,18 general anesthesia was applied with positive pressure ventilation. There are several important potentially relevant physiologic differences between general anesthesia and regional anesthesia. Volatile anesthetics, unlike propofol, alter cerebral autoregulation.19 However, both propofol20 and volatile anesthetics21 may be protective against injury due to cerebral ischemia. Deleterious cardiovascular effects of the sitting position can be minimized with regional anesthesia, as sedated patients can compensate for the decrease in venous return from the sitting position by increasing systemic vascular resistance. Spontaneous ventilation helps to maintain venous return. In contrast, positive pressure ventilation can cause a decrease in cardiac output and cerebral perfusion secondary to decreased venous return, right ventricular dysfunction, and alteration of left ventricular distensibility.4,22
Cerebral saturation has been studied previously and validated. In pediatric patients, it has been measured simultaneously with SpO2 during apnea,23 and it was found to be a more sensitive monitor given that reductions in rSO2 preceded reductions in SpO2. This hysteresis may contribute to a poor correlation between rSO2 and SpO2. Cerebral saturation has been examined as a functional monitor for cerebral ischemia and major organ dysfunction in cardiac, major abdominal, and carotid surgery.10-12,14,24 It generally compares favourably with other monitors of cerebral ischemia, such as transcranial Doppler, somatosensory evoked potentials, and stump pressure during carotid cross-clamp.14,25-27 Although no cutoff value has been universally agreed on,28 a 20% decrease in rSO2 has been suggested as a suitable threshold value to detect cerebral ischemia (sensitivity 80% and specificity 82%) with a primarily high negative predictive value.14 In cardiac surgery, prolonged reductions of rSO2 to < 50% or a > 20% decline from baseline were associated with greater risk of postoperative cognitive decline and increased hospital stay.11,12,24 In elderly patients undergoing abdominal surgery, a > 20-25% decline in rSO2 is associated with early postoperative cognitive decline and increased hospital stay.10 Few of our patients experienced cerebral desaturation and, correspondingly, none of our patients suffered clinically significant cerebral injury.
One limitation to this study is that the sports medicine population is likely at low risk for major morbidity despite use of controlled hypotension in the sitting position. However, shoulder arthroscopy is a commonly performed procedure, and our findings suggest that controlled hypotension, as practiced in this study with this patient population, is associated with a low rate of cerebral oxygen desaturation. Our findings should not be extrapolated to patients undergoing general anesthesia, shoulder procedures that may have more embolic phenomena (e.g., total shoulder replacement), or patients with a greater comorbidity burden. The blood pressures have been adjusted to account for the vertical distance from the external auditory meatus to the fourth intercostal space. Correction was not made for vertical distance from the blood pressure cuff to the heart, which may have variably increased the relevant vertical distance. For this reason, the analyses presented may underestimate the actual adjusted cerebral blood pressures.
Finally, we used three possible definitions of hypotension, all derived from the literature. A patient was considered as experiencing hypotension if any one of three conditions was fulfilled: MAP < 66 mmHg; systolic blood pressure < 90 mmHg and/or a MAP decrease > 30% from baseline. The first criterion may have been too permissive, as 28 patients had a MAP < 66 mmHg at baseline. However, had we used a 50 mmHg cutoff instead, the results shown in Tables 3 and 4 would not have changed qualitatively. The association between hypotension and cerebral desaturation would have been stronger, but the conclusions would not change.
In conclusion, hypotension was frequent but cerebral desaturation was rare among this population of patients (mostly American Society of Anesthesiologists’ physical status I and II) undergoing ambulatory shoulder arthroscopy under regional anesthesia in the sitting position.
Notes
Cullen D, Kirby R. Beach chair position may decrease cerebral perfusion. Catastrophic outcomes have occurred. The Official Journal of Anesthesia Patient Safety Foundation Newsletter 2007; 22: 25.
References
Paul J, Ling E, Lalonde C, Thabane L. Deliberate hypotension in orthopedic surgery reduces blood loss and transfusion requirements: a meta-analysis of randomized controlled trials. Can J Anesth 2007; 54: 799-810.
Degoute CS. Controlled hypotension: a guide to drug choice. Drugs 2007; 67: 1053-76.
Tobias JD. Strategies for minimizing blood loss in orthopedic surgery. Semin Hematol 2004; 41: 145-56.
Pohl A, Cullen DJ. Cerebral ischemia during shoulder surgery in the upright position: a case series. J Clin Anesth 2005; 17: 463-9.
Bijker JB, van Klei WA, Kappen TH, van Wolfswinkel L, Moons KG, Kalkman CJ. Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology 2007; 107: 213-20.
Drummond JC. The lower limit of autoregulation: time to revise our thinking? Anesthesiology 1997; 86: 1431-3.
Sollevi A. Hypotensive anesthesia and blood loss. Acta Anaesthesiol Scand 1988; 32: 39-43.
Dutton RP. Controlled hypotension for spinal surgery. Eur Spine J 2004; 13(Suppl 1): S66-71.
Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth 2009; 103(Suppl 1): i3-13.
Casati A, Fanelli G, Pietropaoli P, et al. Monitoring cerebral oxygen saturation in elderly patients undergoing general abdominal surgery: a prospective cohort study. Eur J Anaesthesiol 2007; 24: 59-65.
Slater JP, Guarino T, Stack J, et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg 2009; 87: 36-45.
Murkin JM, Adams SJ, Novick RJ, et al. Monitoring brain oxygen saturation during coronary bypass surgery: A randomized, prospective study. Anesth Analg 2007; 104: 51-8.
Liu SS, Gordon MA, Wilfred S, Shaw PM, Shetty T, YaDeau JT. A prospective clinical registry of ultrasound-guided regional anesthesia for ambulatory shoulder surgery. Anesth Analg 2010; 111: 617-23.
Samra SK, Dy EA, Welch K, Dorje P, Zelenock GB, Stanley JC. Evaluation of a cerebral oximeter as a monitor of cerebral ischemia during carotid endarterectomy. Anesthesiology 2000; 93: 964-70.
Liguori GA, Kahn RL, Gordon J, Gordon MA, Urban MK. The use of metoprolol and glycopyrrolate to prevent hypotensive/bradycardic events during shoulder arthroscopy in the sitting position under interscalene block. Anesth Analg 1998; 87: 1320-5.
Olsen KS, Svendsen LB, Larsen FS, Paulson OB. Effect of labetalol on cerebral blood flow, oxygen metabolism and autoregulation in healthy humans. Br J Anaesth 1995; 75: 51-4.
Joshi BL, Brady K, Hogue CW. Real time monitoring of cerebral blood flow autoregulation with NIRS during cardiac surgery. Anesthesiology 2009; A1102 (abstract).
Murphy GS, Szokol JW, Marymont JH, et al. Cerebral oxygen desaturation events assessed by near-infrared spectroscopy during shoulder arthroscopy in the beach chair and lateral decubitus positions. Anesth Analg 2010; 111: 496-505.
Strebel S, Lam AM, Matta B, Mayberg TS, Aaslid R, Newell DW. Dynamic and static cerebral autoregulation during isoflurane, desflurane, and propofol anesthesia. Anesthesiology 1995; 83: 66-76.
Gelb AW, Bayona NA, Wilson JX, Cechetto DF. Propofol anesthesia compared to awake reduces infarct size in rats. Anesthesiology 2002; 96: 1183-90.
Warner DS, McFarlane C, Todd MM, Ludwig P, McAllister AM. Sevoflurane and halothane reduce focal ischemic brain damage in the rat. Possible influence on thermoregulation. Anesthesiology 1993; 79: 985-92.
Marshall WK, Bedford RF, Miller ED. Cardiovascular responses in the seated position-impact of four anesthetic techniques. Anesth Analg 1983; 62: 648-53.
Tobias JD. Cerebral oximetry monitoring with near infrared spectroscopy detects alterations in oxygenation before pulse oximetry. J Intensive Care Med 2008; 23: 384-8.
Hong SW, Shim JK, Choi YS, Kim DH, Chang BC, Kwak YL. Prediction of cognitive dysfunction and patients’ outcome following valvular heart surgery and the role of cerebral oximetry. Eur J Cardiothorac Surg 2008; 33: 560-5.
Moritz SM, Kasprzak PH, Arlt M, Taeger K, Metz CF. Accuracy of cerebral monitoring in detecting cerebral ischemia during carotid endarterectomy: a comparison of transcranial Doppler sonography, near-infrared spectroscopy, stump pressure, and somatosensory evoked potentials. Anesthesiology 2007; 107: 563-9.
Duffy C, Manninen P, Chan A, Kearns C. Comparison of cerebral oximeter and evoked potential monitoring in carotid endarterectomy. Can J Anaesth 1997; 44: 1077-81.
Duncan LA, Ruckley CV, Wildsmith JA. Cerebral oximetry: a useful monitor during carotid artery surgery. Anaesthesia 1995; 50: 1041-5.
Pennekamp CW, Bots ML, Kappelle LJ, Moll FL, de Borst GJ. The value of near-infrared spectroscopy measured cerebral oximetry during carotid endarterectomy in perioperative stroke prevention. A review. Eur J Vasc Endovasc Surg 2009; 38: 539-45.
Acknowledgements
We sincerely thank the Somanetics Corporation for providing the cerebral oximetry monitors and probes used for the study. We also thank Joseph Nguyen MPH for statistical advice.
Conflict of interest
None of the authors have potential competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Work should be attributed to: Department of Anesthesiology, Hospital for Special Surgery, Weill Medical College of Cornell University, 535 E 70th Street, New York, NY 10021.
Somanetics Corp. contributed monitors but was not involved in study design, conduct, or manuscript preparation.
Study funded by the Hospital for Special Surgery, Anesthesiology Department—Research and Education Fund.
This article is accompanied by an editorial. Please see Can J Anesth 2011; 58(11).
Rights and permissions
About this article
Cite this article
YaDeau, J.T., Liu, S.S., Bang, H. et al. Cerebral oximetry desaturation during shoulder surgery performed in a sitting position under regional anesthesia. Can J Anesth/J Can Anesth 58, 986–992 (2011). https://doi.org/10.1007/s12630-011-9574-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-011-9574-7