Abstract
Objective
Resolution of the acute respiratory distress syndrome (ARDS) requires clearance of pulmonary edema. Biologically variable ventilation (BVV) strategies that improve gas exchange, lung mechanics, and inflammatory mediators in ARDS may be beneficial in this regard. We used quantitative computed tomography (CT), a single indicator thermodilution system (PiCCO®) to determine extravascular lung water (EVLW), and the change in edema protein concentration over time to compare edema clearance with BVV vs conventional mechanical ventilation (CMV) in a porcine ARDS model.
Methods
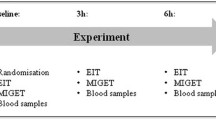
Sixteen pigs with oleic acid lung injury were randomized to four hours of ventilation with either CMV (n = 8) or BVV (n = 8) at identical low tidal volume and minute ventilation over time. Hemodynamic variables, gas exchange, lung mechanics, and PiCCO derived EVLW were determined hourly. Computed tomography images and edema fluid samples were obtained at baseline lung injury and after four hours of ventilation. Wet and dry lung weights were determined postmortem.
Results
At four hours with BVV, peak airway pressure was decreased significantly and lung compliance improved compared with CMV (P = 0.003; P < 0.001, respectively). Hemodynamic variables and gas exchange were not different between groups. Also at four hours, computed tomography revealed an increase in total gas volume (P = 0.001) and a decrease in total lung weight and global lung density (P = 0.005; P = 0.04 respectively) with BVV. These findings were associated with a significant increase in the gas volume of normally aerated lung regions (P < 0.001) and a decrease in the poorly and non-aerated lung regions (P = 0.001). No change in any CT parameter occurred with CMV. The lung weights derived from computed tomography correlated well with postmortem wet weights (R2 = 0.79; P < 0.01). The decrease in PiCCO derived EVLW from injury to four hours did not differ significantly between BVV and CMV. Extravascular lung water showed no correlation with postmortem wet weights and significantly underestimated lung water. Average alveolar fluid clearance rates were positive (1.4%·hr−1 (3%)) with BVV and negative with CMV (−2.0%·hr−1 (4%)).
Conclusions
In a comparison between BVV and CMV, computed tomography evidence suggests that BVV facilitates enhanced clearance and/or redistribution of edema fluid with improved recruitment of atelectatic and poorly aerated lung regions; no such evidence was seen with either single thermodilution measurement of EVLW or edema clearance rates. The results of computed tomography provide further evidence of the benefit of BVV over conventional ventilation in ARDS.
Résumé
Objectif
La résolution d’un syndrome de détresse respiratoire aiguë (SDRA) nécessite l’élimination de l’œdème pulmonaire. Des stratégies de ventilation variable biologique (VVB) améliorant les échanges gazeux, la mécanique ventilatoire et les médiateurs de l’inflammation dans le SDRA pourraient être bénéfiques pour résoudre ce problème. Afin de comparer la résolution de l’œdème avec une VVB par rapport à la ventilation mécanique conventionnelle (VMC) dans un modèle porcin de SDRA, nous avons eu recours à la tomodensitométrie quantitative, à un système de thermodilution à indicateur unique (PiCCO®) afin de déterminer l’eau extravasculaire dans les poumons (EVLW), et avons observé les changements dans la concentration des protéines dans l’œdème au fil du temps.
Méthode
Seize porcs présentant une lésion pulmonaire à l’acide oléique ont été randomisés à être ventilés pendant quatre heures à l’aide de soit une VMC (n = 8), soit une VVB (n = 8). Le volume courant et la ventilation minute étaient bas et les mêmes en fonction du temps. Les variables hémodynamiques, les échanges gazeux, la mécanique ventilatoire et l’EVLW dérivée du PiCCO ont été déterminés une fois l’heure. Des images de tomodensitométrie et des échantillons de liquide de l’œdème ont été obtenus au début de la lésion pulmonaire et après quatre heures de ventilation. Les poids pulmonaires mouillé et sec ont été déterminés post-mortem.
Résultats
Après quatre heures de VVB, la pression ventilatoire maximale était significativement réduite et la compliance pulmonaire améliorée par rapport à la VMC (P = 0,003; P < 0,001, respectivement). Les variables hémodynamiques et les échanges gazeux étaient semblables dans les deux groupes. Après quatre heures également, la tomodensitométrie a révélé une augmentation du volume gazeux total (P = 0,001) et une réduction du poids pulmonaire total ainsi que de la densité pulmonaire globale (P = 0,005; P = 0,04 respectivement) avec la VVB. Ces résultats étaient associés à une augmentation significative du volume gazeux dans les régions pulmonaires ventilées normalement (P < 0,001) et à une réduction du nombre de régions pulmonaires peu ou pas ventilées (P = 0,001). Aucun changement au niveau des paramètres de tomodensitométrie n’est survenu avec la VMC. Les poids des poumons dérivés de la tomodensitométrie étaient bien corrélés avec les poids mouillés post-mortem (R2 = 0,79; P < 0,01). Aucune différence significative n’a été observée au niveau de la réduction de l’EVLW dérivée du PiCCO de la lésion à quatre heures entre la VVB et la VMC. La quantité d’eau extravasculaire n’était pas corrélée aux poids mouillés post-mortem et sous-estimée significativement. La vitesse moyenne d’élimination du liquide alvéolaire était positive (1,4 %·h−1 (3 %)) avec la VVB et négative avec la VMC (-2,0 %·h−1 (4 %)).
Conclusion
Dans une comparaison de la VVB et de la VMC, les données probantes obtenues par tomodensitométrie indiquent que la VVB facilite une meilleure élimination et/ou redistribution du liquide de l’œdème ainsi qu’un meilleur recrutement des régions pulmonaires atélectasiques ou peu ventilées; aucun de ces résultats n’a été observé avec la mesure de thermodilution unique de l’EVLW ou de la vitesse d’élimination de l’œdème. Les résultats de tomodensitométrie fournissent des données probantes supplémentaires soutenant les bienfaits de la VVB par rapport à la ventilation conventionnelle dans le SDRA.
Similar content being viewed by others
The acute respiratory distress syndrome (ARDS) is the end result of an intense inflammatory reaction that damages the alveolar capillary epithelial barrier causing non-hydrostatic alveolar edema, patchy atelectasis, reduced lung compliance, and profound impairment in gas exchange. Resolution requires clearance of edema fluid to restore lung mechanics and gas exchange. Ware and Matthay1correlated alveolar fluid clearance rates with survival in ARDS. In their study, patients with the greatest clearance rates were more likely to be ventilated with lower tidal volumes (VT). In oleic acid (OA) injured pigs, Colmenero-Ruiz et al.2 showed decreased extravascular lung water (EVLW) when VT was reduced from 12 to 6 mL·kg−1. In a rat model of acid-injured lungs, Frank et al. 3 showed an even greater improvement in alveolar fluid clearance and biochemical markers of epithelial and endothelial injury with further VT reduction from 12 to 3 mL·kg−1. Alternatively, Constantin et al.4 showed that recruitment maneuvers were associated with improved alveolar fluid clearance only in those patients in whom recruitment was sustained. Taken together, these results suggest that the ideal ventilation strategy to maximize fluid clearance should provide effective alveolar recruitment with the lowest VT and distending stress.
Biologically variable ventilation (BVV) is one form of variable mechanical ventilation that recapitulates the physiological variability in VT and respiratory rate that is present in healthy breathing patterns.5 In animal models of ARDS, variable ventilation strategies are superior to conventional control mode mechanical ventilation (CMV) or CMV with recruitment maneuvers with respect to lung mechanics, gas exchange, surfactant content, and inflammatory mediators with an overall decrease in distending stress.5-12 In a recent computed tomography (CT) imaging study, we confirmed BVV induced recruitment of both poorly and non-aerated lung regions.13
In this study, we hypothesized that the recruitment benefit and periodic low VT breaths seen with BVV could result in enhanced resolution of edema fluid in ARDS. We used quantitative CT imaging combined with single indicator thermodilution measurements of EVLW and serial measures of edema fluid protein concentration to determine if enhanced clearance of pulmonary edema contributes to the benefits previously demonstrated with BVV.
Methods
Experimental protocol
All animals were managed following University of Manitoba Research Ethics Board Guidelines. A total of 18 farm-bred pigs (22-30 kg) were studied. Instrumentation has been reported previously.7 Total intravenous anesthesia was provided with propofol/ketamine/pancuronium (15/3.75/0.1 mg·kg−1·hr−1) during the experimental period. The animals were ventilated with an Esprit® intensive care ventilator (Respironics Inc., Palo Alto, CA, USA) capable of delivering either CMV or BVV. The ventilator delivered a square wave inspiratory flow pattern with an inspiratory:expiratory (I:E) ratio of 1:2. Animals were ventilated initially with a VT = 10 mL·kg−1, FIO2 = 0.5, and positive end-expiratory pressure (PEEP) = 5 cm H2O. Respiratory rate was adjusted to maintain PaCO2 in the range of 35-45 mmHg. Fluid management was standardized at 10 mg·kg−1·hr−1of normal saline.
Oleic acid lung injury
Oleic acid was infused at 0.2 mg·kg−1·hr−1 until static respiratory system compliance had decreased by at least 40% and PaO2 < 100 mmHg. Dopamine was infused at 5 μg·kg−1·min−1 prior to OA administration, titrated to maintain a mean arterial pressure > 60 mmHg for the period of hemodynamic instability that occurs with OA infusion, then discontinued.
When a stable injury had been achieved, ventilation was maintained in both groups using lower VT (7.5 mL·kg−1 in this model to overcome imposed equipment dead space) and PEEP = 10 cm H2O. A baseline post-injury CT scan was acquired, and then the animal was randomized to receive either BVV or CMV. Ventilation continued at the same minute ventilation and PEEP level for four hours. Hemodynamic variables, gas exchange, lung mechanics, and EVLW were determined hourly.
Biologically variable ventilation
Biologically variable ventilation mode has been described previously.6,7 Briefly, breath-to-breath control of the Esprit ventilator is provided by a modulation file and laptop computer. The modulation file is derived from the breath-to-breath frequency variability that was obtained from a spontaneously ventilating awake subject, captured by a data acquisition system, and processed. Functions were developed to convert the ventilator rate to voltage scaled to the chosen frequency. Voltage to the rate controller is altered based on the next instantaneous rate, and output to control frequency is updated every 5 msec. The ventilator functions as a volume divider - changes in frequency result in reciprocal changes in VT - such that minute ventilation remains fixed.
Computed tomography imaging
A spiral CT was obtained at baseline OA injury and after four hours of ventilation. Following approved Standard Operating Procedures, the animals were transported to the CT scanning facility with ventilation unchanged. Lung imaging was performed from apex to diaphragm using the CT portion of a Siemens Biograph 16 PET/CT camera (Siemens Medical Solutions, Knoxville, TN, USA). This CT camera is equivalent to a Siemens Sensation 16. Images were acquired in spiral mode using a 120 kVp, 150 mAs protocol and reconstructed with a B80 s kernel with slice width of 1.0 mm and slice increment of 0.7 mm. Acquisition of the CT sections required approximately 13 sec, and they were obtained with a respiratory pause at the end of expiration (PEEP = 10 cm H2O). All CT sections were archived to optical disc for later analysis.
The lung CT images were analyzed following the method of Gattinoni et al.,14 which classifies lung regions according to the degree of aeration as measured by the Hounsfield Unit (HU) values in the image. Regions with CT numbers −1000 to −900 HU were overdistended, −900 to −500 HU were normally aerated, −500 to −100 were poorly aerated, and >−100 were non-aerated. Regions of interest were drawn in the images for the entire lung regions, excluding the hilar vessels, in every 25th slice (i.e., at 17.5 mm intervals) to create a total volume of interest (VOI). The CT number values for the voxels in the VOI were extracted, and histograms were developed for the total VOI, allowing the calculation of the percentage of lung volume that fit each of the four classifications.
The global lung volume and global lung weight were obtained from the sum total of the lung volumes and the lung weights, respectively, of all compartments. Global lung density was calculated as the global lung weight divided by the global lung volume.
Regional lung volumes were partitioned into gas and tissue components according to Vieira et al.15 Briefly, using the assumption that the CT number of tissue is equivalent to water, CTwater = 0 HU, and the CT number of air is CTair = −1000 HU, the fraction of gas in a voxel, Fgas, is given by
where CT is the CT number of the voxel in question (i.e., in the −1000 to 0 range for a voxel in the lung region) Fgas can also be denoted as
where Vgas is the volume of gas in a voxel and Vgas+tissue is the total volume of the voxel. Then
Extravascular lung water determination
We used a commercially available thermal indicator system, PiCCO, (Pulsion Medical Systems AG, Munich, Germany) with a thermistor-tipped aortic pressure catheter. The calculation of EVLW is based on the assumption that EVLW = intrathoracic thermal volume (ITTV) – intrathoracic blood volume (ITBV). Ten millilitres of ice-cold saline were injected into the central venous cannula. The PiCCO system calculates the flow (Q) and mean transit time (t) of the thermal indicator and multiplies Q x t to determine the thermal distribution volume between the site of injection and the thermistor, i.e., the ITTV. The downslope time of the thermal dilution curve is multiplied by Q to calculate the volume of the largest mixing chamber in the serial system, which includes the heart chambers and the lungs, i.e., the pulmonary thermal volume. The pulmonary thermal volume is subtracted from the ITTV to determine the extra pulmonary blood volume between the site of injection and the thermistor, i.e., the global end-diastolic volume (GEDV). Intrathoracic blood volume is calculated by the PiCCO system using an empirically established linear relationship between intrathoracic blood volume and GEDV (ITBV = 1.25 GEDV).16 Intrathoracic blood volume is then subtracted from ITTV to determine EVLW. Measurements were performed in triplicate at control, following OA lung injury, and hourly for four hours.
Alveolar fluid clearance
Following the methodology of Ware and Matthay,1 undiluted pulmonary edema fluid samples were aspirated from a distally wedged soft Portex #14 in-line suction catheter and interposed by a Y-connector in the breathing circuit at baseline and at four hours. The samples were centrifuged at 3,000 g for ten minutes, and the supernatant was stored at −80°C. The total protein concentration in edema fluid was measured by the Bradford method. The net alveolar fluid clearance rate was calculated using the formula: %alveolar fluid clearance = 100 x (1 − [initial edema protein/final edema protein])/hour.
At the completion of the experiment, all animals were euthanized and their lungs were excised. After passive exsanguination, wet weights were determined. The lungs were dried and dry lung weights were determined.
Statistical analysis
Data are presented as mean (standard deviation). Mixed measures analysis of variances were used to compare baseline, post OA, two- and four-hour hemodynamic variables, blood gas and mechanics measurements, as well as CT derived total weight, total gas volume, density, and regional gas volumes at baseline and hours. Least mean squares matrices were applied when group-time interactions were significant. Bonferroni’s correction was applied for multiple comparisons. Wet weights, wet to dry weight ratios, and fluid clearance rates were compared between groups by unpaired Student’s t-test analysis. Linear regression analysis was used to correlate CT weight or EVLW to wet weight. Corrected P values < 0.05 were considered significant.
Results
A total of 18 animals were studied. One animal from each group showed evidence of marked hemodynamic instability on return from CT scanning (CO < 1 L·min−1, pH < 7.1). They were removed from the study, leaving eight animals in each group for comparison. Pre-computed tomography data from the excluded animals were removed from the analysis. Computed tomography scanning was unavailable in one CMV animal. Analyzable paired edema fluid samples were obtained from five animals in each group.
Hemodynamic variables, fluid balance, blood gases, calculated shunt, and dead space did not differ between BVV and CMV with OA injury or at any subsequent time period (Tables 1 and 2).
Peak airway pressure increased in both groups, and total respiratory system compliance decreased to a similar extent with OA injury. However, despite identical minute ventilation and average VT, by two hours, peak airway pressure was significantly lower with BVV than with CMV (difference, −3.08 cm H2O; 95% confidence interval (CI), −4.9 to −1.2; P = 0.002). This difference persisted at four hours (difference = -3.0 cm H2O; 95% CI, −4.8 to −1.1; P = 0.003). Similarly total respiratory system compliance improved to a greater extent with BVV than with CMV at both two and four hours (difference at two hours, 0.16 mL·cm−1 H2O; 95% CI, 0.06 to 0.27; P < 0.004) (difference at four hours, 0.2 mL·cm−1 H2O; 95% CI, 0.09 to 0.3; P < 0.001) (Table 3).
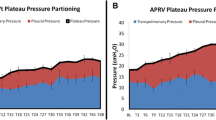
With BVV, CT derived total gas volume increased from 683 (146) mL at baseline OA injury to 780 (146) mL at four hours (difference, 96.9 mL; 95% CI, 46.0 to 146.9; P = 0.001); lung weight decreased from 510 (72) g to 482 (73) g (difference, −28.2 g; 95% CI, −46.4 to −10.1; P = 0.005); and global lung density decreased from 0.45 (0.04) g·mL−1 to 0.39 (0.05) g·mL−1 (difference, −0.06 g·mL−1, 95% CI, −0.08 to −0.4; P = 0.04). With CMV, total gas volume, lung weight, and global lung density were unchanged at four hours compared with baseline OA injury; gas volume (difference, −5.1 mL; 95% CI, −20.1 to 18.6 (P = 0.84); lung weight (difference, 0.8 g; 95% CI, −20.1 to 18.6); density (difference, 0.0 g·mL−1; 95% CI, −0.02 to 0.02) (Fig.1).
Histograms comparing computed tomography derived total gas volume (upper panel), total lung weight (middle panel), and global lung density (lower panel) at baseline (solid bars) vs four hours (hatched bars) for both ventilation modes. Biologically variable ventilation (BVV): n = 8, conventional mechanical ventilation (CMV): n = 7; *Denotes significant difference from baseline
Examining aeration by region, the increase in total gas volume with BVV could be attributed to an increase in normally aerated regional gas volume from 449 (52) mL to 550 (66) mL (difference, 103 mL; 95% CI, 61 to 146; P < 0.001) associated with a reduction in the combined poorly and non-aerated region gas volume (105 (18) mL vs 85 (24) mL, respectively; difference, −18 mL; 95% CI, −28 to −8; P = 0.002) and no significant change in hyperaerated regional gas volume. No significant differences in regional gas volumes were seen with CMV over the same time period; CMV normally aerated (difference, 2.0 mL; 95% CI, −43.7 to 47.6); CMV poorly and non-aerated (difference, 3.7 mL; 95% CI, −6.9 to 14.3) (Fig. 2).
The change in EVLW (determined by the PiCCO monitor) with OA injury and over four hours of ventilation did not differ between BVV and CMV. The alveolar fluid clearance rate (determined by the change in edema protein concentration over four hours) was positive with BVV and negative with CMV, but it was not statistically different between groups. Postmortem wet weight (corrected for dry tissue weight) and wet:dry weight ratios were not different between groups (Table 4).
Fig. 3 shows the correlation between postmortem lung weight and either CT derived lung weight or EVLW determined by PiCCO. An excellent correlation was obtained between gravimetrically determined wet weights and CT derived lung weights (WtCT = 0.96 × WtWet − 31.8; R2 = 0.79; P < 0.0001). No significant correlation between PiCCO determined EVLW and postmortem lung weight was obtained, and the discrepancy between PiCCO EVLW and lung weight increased with increasing lung weight.
Correlation between wet weight of lungs (determined postmortem) and computed tomography (CT) derived lung weight n = 15 (solid triangles) or extravascular lung water (EVLW) n = 15 (open diamonds) determined immediately pre-mortem. Dotted line signifies identity. Computed tomography derived lung weights correlate highly with CT derived lung weights with a slope = 0.96. No correlation between EVLW and lung weight was obtained
Discussion
Our data confirm previously documented improvements with BVV in terms of lung mechanics and recruitment, although gas exchange benefits were not corroborated in the present study. Quantitative CT evidence of a significant decrease in lung weight, an increase in gas volume, and a decrease in lung density supports our hypothesis that a variable ventilation strategy improves pulmonary edema clearance in this ARDS model; our hypothesis was not corroborated by the PiCCO determined EVLW, wet weight, or the change in edema fluid protein concentrations over this short four-hour period.
Improved lung mechanics are confirmed by the significant increase in total respiratory system compliance and the decrease in average peak airway pressure with BVV, consistent with multiple previous studies. Salutary effects on recruitment are supported by CT regional aeration. If the combined change in poorly and non-aerated regional tissue weight relative to total weight is taken as an index of effective recruitment (modified from Malbouisson et al.),17 then recruitment with four hours of ventilation with BVV was 13% (5%) vs −0.3% (7%) with CMV (F = 4.1; P = 0.001 by unpaired Student’s t-test). This modest recruitment effect translated into a 24% increase in normally aerated gas volume, suggesting significant restoration of effective gas exchanging units with BVV, similar to previous reports.13 The models may not be directly comparable, however, as this recruitment benefit was not associated with a similar improvement in gas exchange reported previously. In the current study, we created a more modest OA oxygenation injury, (40% decrease in compliance and PaO2 < 100 mmHg before PEEP increase vs PaO2 < 75 mmHg with initial OA injury) to ensure hemodynamic stability during transport to and from the CT scanning facility. Post OA, the increase in PaO2 after PEEP to 10 cm H2O was higher than that attained in earlier studies (130 mmHg vs < 100 mmHg, respectively)6,7 despite similar decreases in compliance. This suggests that hypoxic pulmonary vasoconstriction was better preserved in the current model. Redistribution of blood flow away from areas of injury would account for the lack of significant difference in gas exchange obtained despite significant differences in mechanics and recruitment. However, we have demonstrated previously that changes in regional aeration correlate with changes in compliance and not with oxygenation, which suggests that ventilation perfusion balance in the porcine injury model is not necessarily coupled to mechanics.13 Evidence that this model resulted in significant edema despite the lack of oxygenation effect is provided by postmortem wet:dry weight ratios = 8 and the quantitative CT results, which showed that poorly and non-aerated regions constitute 60% of the total mass at baseline injury.
We used three methods to assess fluid clearance in this model. Of these, the only indices suggesting a fluid clearance advantage with BVV were the CT derived decreases in total lung weight and density over the four-hour ventilation period. Computed tomography derived lung weights at four hours, postmortem wet weights, and wet:dry weight ratios were not significantly different between groups, but they were all limited to a single measurement in time. The excellent correlation obtained between CT derived lung weight and postmortem lung weight provides validation for the CT determined lung weights post injury and the difference determined over four hours. This capability may provide a more sensitive index of lung water clearance over a short experimental period when modest changes in fluid clearance are present.
Malbouisson et al.18 report a close correlation between CT determination of lung weight and increasing lung water in an isolated lung preparation. This differs from the in situ lung as blood volume is excluded. Gattinoni et al.19 confirmed that the CT determined increase in lung weight was related to both intravascular and EVLW in ARDS patients. In the present study, changes in blood volumes are unlikely to account for the observed difference in CT weight between BVV and CMV as pulmonary arterial pressure, pulmonary capillary wedge pressure, and cardiac output were not different between groups at any time period. We cannot exclude possible differences in interstitial inflammatory cell infiltration that could contribute to total tissue content, but this is unlikely to account for the weight differences observed over a brief four-hour period, This suggests that the decrease in lung weight associated with BVV can most likely be attributed to EVLW. The significant decrease in global lung density further supports this conclusion. Scillia et al.20 revealed a significant correlation between CT derived density and EVLW by means of double indicator dilution in a canine OA model; this was confirmed later by Kuzkov et al.21
The single indicator thermodilution determination of EVLW has been validated clinically against the double indicator dilution method16,22 and has been substantiated in animal studies against gravimetry.23-25 As the PiCCO calculation of EVLW excludes both blood and tissue volumes, we anticipated lower PiCCO derived EVLW values compared with CT determined lung weights, but we expected EVLW to increase as CT lung weight increased with OA injury. However, no correlation between EVLW and either lung weight (Fig. 4) or CT density (R2 = 0.02; P = 0.42) was evident, and the discrepancy between the two measures increased with increasing lung weight (Fig. 4). This suggests that the PiCCO system in this porcine OA model underestimates lung water in more edematous lungs. Although studies show reasonable correlation between PiCCO EVLW and gravimetry,23-25 two of these investigators23,24 and Effros et al.26 provide evidence that thermodilution methods may underestimate EVLW when vascular obstruction from microthrombi, OA, or hypoxic pulmonary vasoconstriction limit access of the thermal indicator to the entire extravascular compartment. Additionally, we report baseline EVLW of 10-11 mL·kg−1, significantly greater than the reported normal range of 3-7 mL·kg−1,27 suggesting that EVLW may also be overestimated at baseline in this model. Previous studies have shown that constant relating GEDV to ITBV, used to calculate EVLW by the PiCCO system, may be species or size-dependent, contributing to this overestimation.23,28 Additionally, Lemson et al.29 report much higher baseline extravascular lung water index (EVLWI) values in children (mean = 12, range 8-22 mL·kg−1) compared with adults, and they showed a negative correlation between age and the EVLWI, suggesting that the EVLWI might also be an age dependent variable. We used the default PiCCO settings with an adult patient population based constant = 1.25.16 Correction of the EVLWI with constants of 1.52 or 1.72, as suggested by Rossi23 or Neumann,28 respectively, shifts the EVLWI to lower values at all time periods without changing the overall results. Systematic overestimation of EVLW at baseline and underestimation of EVLW post OA administration may render the single thermodilution method relatively insensitive in this small animal OA injury preparation, contributing to both the unexpectedly small measured increase in EVLW post OA and the discrepancy in results between CT weight/density and PiCCO derived EVLW.
Left-hand panel demonstrates Jensen’s inequality as it applies to the lower convex curvilinear portion of the pressure volume curve obtained from an oleic acid injured pig. Reprinted with permission from: Brewster JA, Graham MR, Mutch WA. J. R. Soc. Interface 2005. 2: 393-396. Probability density functions for biologically variable ventilation pressures and volumes are shown by the hatched curves on the margins. Biologically variable ventilation pressures are uniformly distributed from 10 to 26 cm H2O. At a mean pressure of 18 cm H2O (Biologically variable ventilation [BVV]: solid circle, conventional mechanical ventilation [CMV]: open circle), the mean volume obtained during BVV is 205.7 mL, 12% greater than that obtained at the same average pressure during CMV (183.1 mL). Right-hand panel shows the relationship between fluid clearance and decreasing VT determined by Frank et al. in acid injured rat lungs. Reprinted with permission of the American Thoracic Society Copyright ©. Frank JA, Gutierrez JA, Jones KD, et al. Low tidal volume reduces epithelial and endothelial injury in acid injured rat lungs. AJRCCM 2002: 165; 242-9. Here we show that the relationship also fits a convex curvilinear function (superimposed dotted line, R2 = 0.97; P = 0.01) such that Jensen’s inequality may also be applied. See text for further details
The rate of change in edema fluid protein concentration over time provides an indication of epithelial barrier function as it reflects the clearance of water from the alveolar space over time. Matthay et al.30 document maximal edema clearance rates of > 14%·hr−1 with hydrostatic edema. However, the majority of patients with ARDS have reported fluid clearance rates < 3%·hr−1,1 consistent with the results observed in the present study. Although average clearance rates were positive, suggesting edema resolution with BVV, and negative, suggesting ongoing edema production with CMV, the lack of statistical difference between groups may be accounted for by the large inter-animal variability in the measurement and the limited number of comparisons. We were unable to obtain adequate volumes of edema fluid by aspiration for analysis at four hours in all animals despite wet:dry weight ratios consistent with the presence of excess lung water. However, the very low clearance rates obtained in both groups suggest that a four-hour study period is not sufficient to restore alveolar-epithelial barrier function in this OA model.
Limitations of the study include the modest injury produced, the short four-hour ventilation period, and the small number of subjects studied. These parameters were chosen as multiple previous studies have demonstrated significant BVV advantages with respect to lung mechanics, gas exchange, and inflammatory mediators within this time period with a similar number of subjects,6,7 and Ware and Matthay1 were able to demonstrate significant differences in fluid clearance rates in clinical subjects over a similar time frame. Given the more modest effects seen with a less severe injury model, however, significant differences were limited to the CT findings. Studies of longer duration with a larger number of subjects are required to be adequately powered to show significance with alternative measures of EVLW.
We propose two potential mechanisms to account for the CT results obtained: redistribution of edema fluid from recruitment of collapsed alveoli and enhanced fluid clearance from the low VT breaths included in the BVV file. In a canine OA injury model, Malo et al. 31 showed that PEEP induced recruitment may redistribute edema fluid within the compliant perivascular space such that gas exchange is restored without affecting total EVLW. Biologically variable ventilation induced recruitment may similarly redistribute edema fluid. Redistribution of edema within the lungs could contribute to significant differences in mechanics, aeration, and density in the face of unchanged EVLW or wet:dry weight ratios, as reported currently, but this cannot account for the significant differences in CT weights obtained, suggesting that enhanced clearance must also have occurred.
Frank et al. 3 showed that VT reduction to levels even below that recommended by the ARDSNet trial was associated with the greatest improvement in fluid clearance. Biologically variable ventilation is unique in that both lower (presumably advantageous) and higher (presumably disadvantageous) VT breaths are included in the modulation file. With VT centred at 7.5 mL·kg−1, breaths < 7.5 mL·kg−1 account for 50%, while those < 4 mL·kg−1 account for < 3% of the total modulation file used in the study.
The following may account for a fluid clearance benefit of even a small proportion of very low VT breaths when a variable ventilation strategy is used. To account for the recruitment benefit seen with BVV, we previously proposed the mathematical principle of Jensen’s inequality as it applies to any convex curvilinear relationship.32 When low VT strategies are applied, ventilation occurs on the lower convex curvilinear portion of the sigmoidal ARDS pressure–volume curve. Under these conditions, Jensen’s inequality states that the application of a variable end-inspiratory pressure at the same average input pressure - as occurs with BVV- will result in greater lung volume (i.e., recruitment) over time compared with the same average pressure delivered monotonously. Due to the curvilinear nature of the relationship, the volume gain at higher pressure exceeds the volume loss at lower pressures. In Fig. 4, the data obtained from Frank et al.3 relating fluid clearance to decreasing VT can also be shown to fit a convex curvilinear relationship such that Jensen’s inequality may also be applied. Using the same low VT protocol, it follows that a variable ventilation strategy may confer benefit with respect to recruitment from the larger breaths and fluid clearance from the smaller breaths invoking the same principle (Jensen’s inequality) applied to two separate curvilinear functions: i) disproportionate lung recruitment with improved compliance and gas exchange resulting from the intermittent higher tidal volumes as applied to the convex curvilinear pressure-volume curve and ii) disproportionately greater fluid clearance resulting from the intermittent lower tidal volumes applied to the convex curvilinear fluid clearance-tidal volume curve.
In conclusion, in this porcine ARDS model, CT imaging suggests that salutary redistribution and improved clearance of pulmonary edema contribute to the beneficial effects of BVV within the limited four-hour period of study. Neither single indicator thermodilution nor the change in alveolar fluid protein concentrations differed significantly over this same time frame. Studies of longer duration with a larger number of subjects would be required to have adequate statistical power to show significance with alternative measures of EVLW and to determine if these trends are sustained.
References
Ware LB, Matthay MA. Alveolar fluid clearance is impaired in the majority of patients with acute lung injury and the acute respiratory distress syndrome. Am J Respir Crit Care Med 2001; 163: 1376-83.
Colmenero-Ruiz M, Fernandez-Mondejar E, Fernandez-Sacristan MA, Rivera-Fernandez R, Vazquez-Mata G. PEEP and low tidal volume ventilation reduce lung water in porcine pulmonary edema. Am J Respir Crit Care Med 1997; 155: 964-70.
Frank JA, Gutierrez JA, Jones KD, Allen L, Dobbs L, Matthay MA. Low tidal volume reduces epithelial and endothelial injury in acid-injured rat lungs. Am J Respir Crit Care Med 2002; 165: 242-9.
Constantin JM, Cayot-Constantin S, Roszyk L, et al. Response to recruitment maneuver influences net alveolar fluid clearance in acute respiratory distress syndrome. Anesthesiology 2007; 106: 944-51.
Lefevre GR, Kowalski SE, Girling LG, Thiessen DB, Mutch WA. Improved arterial oxygenation after oleic acid lung injury in the pig using a computer-controlled mechanical ventilator. Am J Respir Crit Care Med 1996; 154: 1567-72.
Funk DJ, Graham MR, Girling LG, et al. A comparison of biologically variable ventilation to recruitment manoeuvres in a porcine model of acute lung injury. Respir Res 2004; 5: 22.
Boker A, Graham MR, Walley KR, et al. Improved arterial oxygenation with biologically variable or fractal ventilation using low tidal volumes in a porcine model of acute respiratory distress syndrome. Am J Respir Crit Care Med 2002; 165: 456-62.
Arold SP, Mora R, Lutchen KR, Ingenito EP, Suki B. Variable tidal volume ventilation improves lung mechanics and gas exchange in a rodent model of acute lung injury. Am J Respir Crit Care Med 2002; 165: 366-71.
Arold SP, Suki B, Alencar AM, Lutchen KR, Ingenito EP. Variable ventilation induces endogenous surfactant release in normal guinea pigs. Am J Physiol Lung Cell Mol Physiol 2003; 285: L370-5.
Bellardine CL, Hoffman AM, Tsai L, et al. Comparison of variable and conventional ventilation in a sheep saline lavage lung injury model. Crit Care Med 2006; 34: 439-45.
Spieth PM, Carvalho AR, Pelosi P, et al. Variable tidal volumes improve lung protective ventilation strategies in experimental lung injury. Am J Respir Crit Care Med 2009; 179: 684-93.
Thammanomai A, Hueser LE, Majumdar A, Bartolak-Suki E, Suki B. Design of a new variable-ventilation method optimized for lung recruitment in mice. J Appl Physiol 2008; 104: 1329-40.
Graham RM, Goertzen AL, Girling LG, et al. Quantitative computed tomography in porcine lung injury with variable vs. conventional ventilation: recruitment and surfactant replacement. Crit Care Med 2011; doi: 10.1097/CCM.0b013e3182186d09
Gattinoni L, Caironi P, Pelosi P, Goodman LR. What has computed tomography taught us about the acute respiratory distress syndrome? Am J Respir Crit Care Med 2001; 164: 1701-11.
Vieira SR, Puybasset L, Lu Q, et al. A scanographic assessment of pulmonary morphology in acute lung injury. Significance of the lower inflection point detected on the lung pressure-volume curve. Am J Respir Crit Care Med 1999; 159: 1612-23.
Sakka SG, Ruhl CC, Pfeiffer UJ, et al. Assessment of cardiac preload and extravascular lung water by single transpulmonary thermodilution. Intensive Care Med 2000; 26: 180-7.
Malbouisson LM, Muller JC, Constantin JM, et al. Computed tomography assessment of positive end-expiratory pressure-induced alveolar recruitment in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 2001; 163: 1444-50.
Malbouisson LM, Preteux F, Puybasset L, Grenier P, Coriat P, Rouby JJ. Validation of a software designed for computed tomographic (CT) measurement of lung water. Intensive Care Med 2001; 27: 602-8.
Gattinoni L, Pesenti A, Bombino M, et al. Relationships between lung computed tomographic density, gas exchange, and PEEP in acute respiratory failure. Anesthesiology 1988; 69: 824-32.
Scillia P, Bankier AA, Gevenois PA. Computed tomography assessment of lung structure and function in pulmonary edema. Crit Rev Comput Tomogr 2004; 45: 293-307.
Kuzkov VV, Suborov EV, Kirov MY, et al. Radiographic lung density assessed by computed tomography is associated with extravascular lung water content. Acta Anaesthesiol Scand 2010; 54: 1018-26.
Michard F, Schachtrupp A, Toens C. Factors influencing the estimation of extravascular lung water by transpulmonary thermodilution in critically ill patients. Crit Care Med 2005; 33: 1243-7.
Rossi P, Wanecek M, Rudehill A, Konrad D, Weitzberg E, Oldner A. Comparison of a single indicator and gravimetric technique for estimation of extravascular lung water in endotoxemic pigs. Crit Care Med 2006; 34: 1437-43.
Kirov MY, Kuzkov VV, Kuklin VN, Waerhaug K, Bjertnaes LJ. Extravascular lung water assessed by transpulmonary single thermodilution and postmortem gravimetry in sheep. Crit Care 2004; 8: R451-8.
Katzenelson R, Perel A, Berkenstadt H, et al. Accuracy of transpulmonary thermodilution versus gravimetric measurement of extravascular lung water. Crit Care Med 2004; 32: 1550-4.
Effros RM, Pornsuriyasak P, Porszasz J, Casaburi R. Indicator dilution measurements of extravascular lung water: basic assumptions and observations. Am J Physiol Lung Cell Mol Physiol 2008; 294: L1023-31.
Lewis FR, Elings VB, Hill SL, Christensen JM. The measurement of extravascular lung water by thermal-green dye indicator dilution. Ann N Y Acad Sci 1982; 384: 394-410.
Neumann P. Extravascular lung water and intrathoracic blood volume: double versus single indicator dilution technique. Intensive Care Med 1999; 25: 216-9.
Lemson J, Backx AP, van Oort AM, Bouw TP, van der Hoeven JG. Extravascular lung water measurement using transpulmonary thermodilution in children. Pediatr Crit Care Med 2009; 10: 227-33.
Matthay MA, Folkesson HG, Clerici C. Lung epithelial fluid transport and the resolution of pulmonary edema. Physiol Rev 2002; 82: 569-600.
Malo J, Ali J, Wood LD. How does positive end-expiratory pressure reduce intrapulmonary shunt in canine pulmonary edema? J Appl Physiol 1984; 57: 1002-10.
Brewster JF, Graham MR, Mutch WA. Convexity, Jensen’s inequality and benefits of noisy mechanical ventilation. J R Soc: Interface 2005; 2: 393-6.
Acknowledgements
The authors gratefully acknowledge Pulsion Medical Systems, Munich Germany for use of the PiCCO System, Brenden Dufault MSc for statistical analysis and Nora Nolette for performing the protein assays.
Funding
2008 CAS/GE Healthcare Canada Research Award in Perioperative Imaging
Competing interests
The University of Manitoba and Dr. WAC Mutch potentially stand to gain from commercialization of the BVV software.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Graham, M.R., Gulati, H., Kha, L. et al. Resolution of pulmonary edema with variable mechanical ventilation in a porcine model of acute lung injury. Can J Anesth/J Can Anesth 58, 740–750 (2011). https://doi.org/10.1007/s12630-011-9517-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-011-9517-3