Abstract
Purpose
Dexmedetomidine, a selective α2 adrenoreceptor agonist, has analgesic and sedative properties, minimal impact on respiratory parameters, and reportedly decreases analgesic requirements after surgery. Given its pharmacodynamic profile, dexmedetomidine might have a role for postoperative pain control in children undergoing tonsillectomy. In this study, we hypothesized that dexmedetomidine would delay and decrease opioid requirements after tonsillectomy.
Methods
In a double-blind controlled trial, participants undergoing tonsillectomy were randomized to receive one intravenous dose of fentanyl (1 μg·kg−1 or 2 μg·kg−1) or dexmedetomidine (2 μg·kg−1 or 4 μg·kg−1) immediately after endotracheal intubation. Primary outcomes included requirement for rescue morphine in the initial postoperative period.
Results
One hundred and one children were enrolled. During the postoperative period, dexmedetomidine (2 and 4 μg·kg−1 groups combined) significantly prolonged the opioid-free interval of children who underwent tonsillectomy compared with fentanyl (1 and 2 μg·kg−1 groups combined) (P < 0.001). Children treated with dexmedetomidine 2 μg·kg−1 vs dexmedetomidine 4 μg·kg−1 had similar cumulative incidence curves for time to morphine rescue, whereas there was a small difference in time to first morphine rescue administration when comparing fentanyl 1 μg·kg−1 vs fentanyl 2 μg·kg−1. Furthermore, length of stay in the postanesthesia care unit was significantly longer for children treated with dexmedetomidine vs children treated with fentanyl (P = 0.0016).
Conclusions
High-dose dexmedetomidine decreases opioid requirements, prolongs the opioid-free interval after tonsillectomy, and prolongs length of stay in the postanesthesia care unit. It is conceivable that these early opioid-sparing effects could benefit patients at risk for respiratory complications early in the postoperative course after tonsillectomy (e.g., patients with obstructive sleep apnea). (ClinicalTrials.gov number, NCT00654511).
Résumé
Objectif
La dexmédétomidine, un agoniste sélectif des récepteurs adrénergiques α2, a des propriétés analgésiques et sédatives ainsi qu’un impact minimal sur les paramètres respiratoires. De plus, elle semble réduire les besoins analgésiques après une chirurgie. Étant donné son profil pharmacodynamique, la dexmédétomidine pourrait jouer un rôle sur le contrôle de la douleur postopératoire chez les enfants subissant une amygdalectomie. Dans cette étude, nous avons émis l’hypothèse que la dexmédétomidine retarderait et réduirait les besoins en opioïdes après une amygdalectomie.
Méthode
Dans une étude contrôlée à double insu, les participants devant subir une amygdalectomie ont été randomisés à recevoir une dose intraveineuse de fentanyl (1 μg·kg−1 ou 2 μg·kg−1) ou de dexmédétomidine (2 μg·kg−1 ou 4 μg·kg−1) immédiatement après l’intubation endotrachéale. Le critère d’évaluation principal était le besoin en analgésie morphinique de secours dans la période postopératoire initiale.
Résultats
Cent-un enfants ont été recrutés. Pendant la période postopératoire, la dexmédétomidine (groupes 2 et 4 μg·kg−1 combinés) a prolongé de façon significative l’intervalle sans opioïde chez les enfants subissant une amygdalectomie par rapport au fentanyl (groupes 1 et 2 μg·kg−1 combinés) (P < 0,0001). Les enfants traités avec de la dexmédétomidine 2 μg·kg−1 vs de la dexmédétomidine 4 μg·kg−1 ont affiché des courbes d’incidence cumulative semblables au niveau du temps jusqu’à administration d’une analgésie morphinique de secours. En revanche, une légère différence a été observée dans les temps jusqu’à la première administration de morphine de secours lors de la comparaison de fentanyl 1 μg·kg−1 et de fentanyl 2 μg·kg−1. De plus, la durée de séjour en salle de réveil était significativement plus longue pour les enfants traités avec de la dexmédétomidine que pour les enfants traités avec du fentanyl (P = 0,0016).
Conclusion
La dexmédétomidine en forte dose réduit les besoins en opioïdes, prolonge l’intervalle sans opioïde après une amygdalectomie, et prolonge également la durée de séjour en salle de réveil. On peut imaginer que ces effets précoces de réduction des besoins en opioïdes pourraient être avantageux pour les patients présentant un risque de complications respiratoires en période postopératoire après une amygdalectomie (par ex. les patients souffrant d’apnée obstructive du sommeil). (Numéro de ClinicalTrials.gov, NCT00654511).
Similar content being viewed by others
Tonsillectomies are among the pediatric surgical procedures most commonly performed in North America and Europe. In the United States alone, approximately one in every 154 children undergoes the procedure each year.1–4 The procedure can be associated with significant postoperative pain, and opioids are used commonly to treat post-tonsillectomy pain. As opioids can be associated with respiratory depression, otolaryngologists and anesthesiologists alike must reconcile adequacy of pain control with the risk of respiratory complications after tonsillectomy. This is particularly important because agents without respiratory depressant effects, such as non-steroidal anti-inflammatory drugs, acetaminophen, and local anesthetics, while used, are often inadequate to treat postoperative tonsillectomy pain.4–9 Dexmedetomidine, a selective α2 adrenoreceptor agonist with sedative and analgesic properties and without respiratory depressant effects, was shown to have similar effects on post-tonsillectomy opioid-rescue needs as did higher doses of morphine.10 More recently, researchers also showed that an intraoperative infusion of dexmedetomidine reduces the proportion of patients requiring morphine rescue during the postoperative period after tonsillectomy.11 Therefore, some studies10,11 suggest that dexmedetomidine might have a role in pain control after tonsillectomies.
While the perioperative course is uneventful for the vast majority of patients undergoing tonsillectomy,3 the search for alternative pain management after tonsillectomy is important because it can be associated with significant respiratory morbidity in a subset of patients.12–14 Patients younger than three years, with Down syndrome or with co-morbidities, such as asthma and neuromuscular diseases, as well as those with severe obstructive sleep apnea syndrome are at increased risk for complications after tonsillectomy.14,15 Researchers have shown that half of the medical interventions performed to treat respiratory morbidity in children undergoing tonsillectomy are needed within the first postoperative hour.15 Furthermore, researchers showed that children with obstructive sleep apnea appear to have increased sensitivity to opioids, and respiratory complications after adenotonsillectomies are often seen within two hours of opioid administration.15,16 In addition, a recent retrospective study showed that the need for major medical interventions to treat respiratory complications was significantly reduced when high-risk children undergoing adenotonsillectomy received fewer opioids.13 Therefore, taken together, these studies provide circumstantial evidence that an analgesic regimen that obviates, reduces, or delays the need for opioids is desirable and might reduce respiratory complications after tonsillectomies.
In this investigation, we conducted a single-centre double-blind randomized clinical trial to examine whether high doses of dexmedetomidine impact on opioid requirement and opioid-free interval after tonsillectomy. We hypothesized that dexmedetomidine administered at high doses would decrease postoperative morphine requirements and delay the need for its administration after tonsillectomy in children.
Methods
We conducted a single-centre double-blind randomized clinical trial from November 2007 to July 2008. Institutional Review Board approval, written parental consent, and patient assent (patients seven years and older) were obtained. Prior to study initiation, an investigational new drug approval for dexmedetomidine use in children was obtained from the Food and Drug Administration (IND#75,079).
Male or female children (ages two to 12 yr and American Society of Anesthesiologists [ASA] physical status classification I or II) scheduled for elective tonsillectomy, with or without adenoidectomy, were assessed for enrolment by one of the investigators. Children with personal or family history of malignant hyperthermia, significant renal or hepatic disorders, opioid allergy, and history of dysrhythmias or congenital heart disease were excluded.
Interventions
Patients enrolled were assigned randomly to receive one of four treatments to be administered intravenously (IV) after endotracheal intubation: fentanyl 1 μg·kg−1 or 2 μg·kg−1 (current standard of practice groups) or dexmedetomidine 2 μg·kg−1 or 4 μg·kg−1 (study groups). The randomization scheme was generated using a computerized uniform random number generator using a locally-written program in SAS® called the SAS randuni function, which generates a list of uniformly distributed random numbers. The randomization list was implemented with sealed opaque sequentially numbered envelopes and was accessible only to the research coordinator not involved in patient enrolment, evaluation, or data collection. Investigators, participants, and evaluators were unaware of the treatment allocation scheme. Study drugs were prepared according to a written protocol by an anesthesiologist not involved in the patient’s care, data collection, or patient enrolment and evaluation. All study drugs were diluted in 10 mL of normal saline in syringes labelled with the patient study number, and the drugs were administered by the attending anesthesiologist who was unaware of its contents.
With parents’ or caregivers’ presence in an induction room, anesthesia was induced in a standard manner with nitrous oxide/oxygen (2:1) gas mixture and sevoflurane. After loss of consciousness, IV access was established and propofol 1 mg·kg−1 iv was administered to facilitate endotracheal intubation. After endotracheal intubation, the study drug was administered IV over ten minutes and the end of infusion was considered time zero. Children were then transported to the operating room on 3% sevoflurane in oxygen. Anesthesia was maintained with desflurane and 70% nitrous oxide in oxygen and was titrated as deemed appropriate by the attending anesthesiologist. Ventilation was controlled initially, but patients were allowed to breathe spontaneously after surgical incision. Dexamethasone 0.5 mg·kg−1 iv (up to 12 mg) was administered to all patients according to current institutional practice for tonsillectomy. Tonsillectomies were performed in all patients using the traditional extra-capsular electrocautery dissection technique. Upon completion of surgery, desflurane and nitrous oxide were discontinued, and the trachea was extubated upon emergence from anesthesia (spontaneous eye opening, cough, or purposeful movement). Patients were then transferred to the postanesthesia care unit (PACU). In the PACU and during hospital admission, subjects with a pain score of ≥6 and/or an agitation score ≥2 received morphine sulfate 50 μg·kg−1 iv according to our hospital’s current standard of care. Subjects experiencing nausea or vomiting received ondansetron 0.15 mg·kg−1 iv every six hours as needed. According to our standards of practice, patients were discharged home from the PACU or admitted to the hospital for up to 23 hr after the procedure. Patients with any significant co-morbidity could be admitted to the hospital at the discretion of the attending surgeon and/or anesthesiologist who were unaware of the patients’ study groups.
Primary and secondary outcomes
The primary outcome was time to morphine-rescue requirement in the initial postoperative period. Secondary outcomes included total amount of morphine required during hospital admission (including PACU and overnight stay), proportion of patients requiring morphine rescue, time to emergence (defined as the time from discontinuation of desflurane to time of spontaneous eye opening, cough, or purposeful movement prior to extubation), incidence of agitation, length of stay in PACU, incidence of postoperative nausea and vomiting, need for anti-emetics, as well as heart rate and blood pressure intraoperatively and during recovery.
Clinical evaluations
We used the objective pain scale to quantify postoperative pain in the PACU.17 The patients’ behaviour during emergence from anesthesia and in the PACU was rated on a four-point agitation scale described by Watcha et al. (1 = calm; 2 = crying, but consolable; 3 = crying inconsolably; 4 = thrashing around).18 A score of 0 was assigned if the child was asleep. A single clinical research nurse, unaware of the patient’s treatment, conducted and recorded pain assessments every five minutes for the first fifteen minutes and every fifteen minutes thereafter. The PACU length of stay was recorded when discharge criteria (defined as Stewart Recovery Scale score of 6) was met.19
Statistical analysis
Based on the reported time to administration of opioid and the incidence of opioid rescue requirement after tonsillectomy,20 we determined the appropriate sample size to maintain a power of at least 80%. We used the survival analysis sample size and power estimator in PASS,Footnote 1 specifically the Kaplan-Meier panel developed per Lakatos,21 which is based on the log-rank test. For the primary comparison of dexmedetomidine vs fentanyl, an estimate of the proportion of patients requiring morphine can be entered for each of two groups, assuming equal post surgery follow-up. This tool allowed us to estimate the sample size required to detect about a 60% reduction in morphine use in the dexmedetomidine group in comparison with about a 40% reduction in the fentanyl group with 80% power, two tailed alpha = 0.05. A sample size of 105 was produced, which we adjusted to 100 because we considered the 40% estimate to be conservative. Using the original estimate, this would represent about a 62% reduction.
Descriptive statistics were used to present all findings other than the primary hypotheses comparing drugs, and we provided the means and standard deviations or median, 25th and 75th percentiles, for the demographics and hemodynamic measures at baseline, as appropriate. Continuous variables were summarized with mean (standard deviation) or as median (interquartile range) if their distribution was skewed. Nominal variables were summarized as number (percentage). Cumulative incidence curves for the time to morphine rescue, time to emergence, and length of stay in the PACU were calculated using the Kaplan-Meier method, and the difference between the two treatment groups was assessed with the log-rank test. For descriptive purposes, Kaplan-Meier graphs comprising the breakdown of both drugs by dosages are presented for time to emergence, time to first morphine rescue, and length of stay in the PACU. A Cox model comparing the two drugs was estimated for time to first morphine rescue, controlling for time to emergence. Hazard and adjusted hazard ratios are presented for this model. Stata® 11 software (StataCorp. 2009) was used for all analyses.
Results
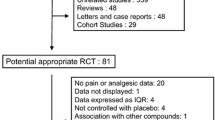
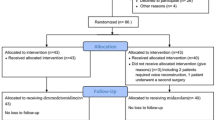
One hundred and nine consecutive patients were assessed for eligibility, eight parents declined participation, and 101 children were enrolled and assigned randomly to a study group as described in Table 1. Throughout the study, no intervention was discontinued; no patient was lost to follow-up, and all enrolled subjects were included in the analysis. Patient demographics, ASA classification, and presence of obstructive sleep apnea as documented in sleep studies are shown in Tables 1 and 2. Overall, patient randomization created the expected balance across groups and modest differences in respiratory rate were not clinically significant (Table 2).
Primary outcome
Fig. 1 shows the cumulative incidence curves for time to morphine rescue (Kaplan-Meier graphs) for the study groups. After tonsillectomy, children treated with dexmedetomidine (2 and 4 μg·kg−1 groups combined) had significantly longer opioid-free intervals compared with children treated with fentanyl (1 and 2 μg·kg−1 groups combined) (P < 0.001). Children treated with dexmedetomidine 2 μg·kg−1 vs dexmedetomidine 4 μg·kg−1 had similar cumulative incidence curves for time to morphine rescue (Fig. 1, bottom panel). In contrast, the fentanyl 1 μg·kg−1 treatment curve appears to dominate the fentanyl 2 μg·kg−1 treatment curve, (Fig. 1, bottom panel).
Cumulative incidence curves for time to morphine rescue (Kaplan-Meier graphs) administration for the dexmedetomidine (Dex) and fentanyl treatment groups. The top panel shows children treated with dexmedetomidine (2 and 4 μg·kg−1 groups combined) vs. those treated with fentanyl (1 and 2 μg·kg−1 groups combined), and the bottom panel shows each of the four study groups. The number of patients in each study group at risk of requiring morphine rescue at the times indicated is shown below the x axis.
Secondary outcomes
Table 3 shows the proportion of patients experiencing pain and requiring opioid rescue after tonsillectomy. The proportion of patients with an agitation score ≥2 during emergence from anesthesia and during PACU stay appears to be lower in the dexmedetomidine group with <20% of patients having an agitation score ≥2 in both dexmedetomidine groups and >50% of patients having an agitation score ≥2 in both fentanyl groups.
The time to emergence from anesthesia appeared longer in the dexmedetomidine 4 μg·kg−1 group than in the fentanyl groups, as demonstrated by the Kaplan-Meier curves presented in Fig. 2 (P = 0.0343, uncorrected P value). There appears to be no substantial difference between time to emergence comparing patients treated with dexmedetomidine 2 μg·kg−1 and dexmedetomidine 4 μg·kg−1, and between time to emergence comparing patients treated fentanyl 1 μg·kg−1 and fentanyl 2 μg·kg−1(Fig. 2, bottom panel). Length of stay in the PACU was significantly longer for patients treated with dexmedetomidine (both doses combined) than for patients treated with fentanyl (P = 0.0016) (Fig. 3). There appeared to be no substantial difference in length of stay in the PACU between the dexmedetomidine 2 μg·kg−1 and the dexmedetomidine 4 μg·kg−1 treatment groups (Fig. 3, bottom panel). In addition, there was no apparent difference in length of stay in the PACU between the fentanyl 1 μg·kg−1 and the fentanyl 2 μg·kg−1 treatment groups (Fig. 3, bottom panel).
Cumulative incidence curves for time to emergence from anesthesia (Kaplan-Meier graphs) for the dexmedetomidine (Dex) and fentanyl treatment groups. The top panel shows children treated with dexmedetomidine (2 and 4 μg·kg−1 groups combined) vs. children treated with fentanyl (1 and 2 μg·kg−1 groups combined), and the bottom panel shows each of the four study groups. The number of patients in each study group at risk of emerging from anesthesia at the times indicated is shown below the x axis.
Cumulative incidence curves for length of PACU stay (Kaplan-Meier graphs) for the dexmedetomidine (Dex) and fentanyl treatment groups. The top panel shows children treated with dexmedetomidine (2 and 4 μg·kg−1 groups combined) vs children treated with fentanyl (1 and 2 μg·kg−1 groups combined), and the bottom panel shows each of the four study groups. The number of patients in each study group at risk of being discharged from the postanesthesia care (PACU) unit at the times indicated is shown below the x axis.
Our finding of the significant delay in time to first morphine rescue and the delay in emergence from anesthesia of dexmedetomidine vs fentanyl raised the issue whether the delay in emergence from anesthesia could partly explain the delay in first morphine rescue requirement. In order to examine the role that differential delay in time to emergence may have played in the delay in administration of first morphine rescue, we estimated a Cox proportional hazard model examining first use of morphine rescue controlling for time to emergence. Even after controlling for time to emergence, there remained a statistically significant Cox hazard ratio of 0.93 (95% confidence interval, 0.88 to 0.99), suggesting a significantly lower risk of morphine rescue requirement for dexmedetomidine over fentanyl treatments.
Interestingly, in post-hoc analyses, we found that the risk for morphine rescue requirement in all treatment groups after tonsillectomies appeared to be higher in males than in females (hazard ratio for morphine rescue requirement, 1.81; 95% confidence interval, 1.15 to 2.89).
Regarding the hemodynamic variables, while dexmedetomidine tended to slow heart rate, the mean values of heart rate and systolic blood pressure were not significantly different at corresponding time points in the two groups (Table 4).
Discussion
This single-centre randomized double-blind clinical trial in children comparing dexmedetomidine with fentanyl showed that dexmedetomidine prolongs the opioid-free interval after tonsillectomy and appears to decrease overall morphine requirements as well as the risk of morphine-rescue administration. These opioid-sparing effects were coupled with prolonged time to emergence from anesthesia and increased length of stay in the PACU. In addition, dexmedetomidine, administered as a single bolus dose, appears to attenuate the hemodynamic changes (increases in heart rate and blood pressure) known to occur at stimulating times during tonsillectomy and the initial PACU stay. Our findings support the notion that a selective α2 adrenoreceptor agonist, such as dexmedetomidine, might have favourable opioid sparing effects and perhaps should be considered as an adjunct for analgesia during and after tonsillectomies.
We and others have examined the role of dexmedetomidine during tonsillectomies in children because it has anxiolytic and analgesic properties that are not associated with respiratory depression.10,11,22–24 In a study of patients undergoing tonsillectomies, 30 children were randomized to receive a single intraoperative dose of dexmedetomidine 0.5 μg·kg−1 or morphine 50 μg·kg−1. In that study, dexmedetomidine had no opioid sparing effect compared with morphine.10 More recently, in a study of 109 children undergoing tonsillectomies, dexmedetomidine 0.75 or 1 μg·kg−1 had no impact on total postoperative morphine opioid requirements compared with morphine.22 Contrary to those reports, we found that significantly higher doses of dexmedetomidine had a significant opioid-sparing effect and increased opioid-free interval after tonsillectomy compared with fentanyl. Our findings are in concert with recent reports showing that dexmedetomidine had an opioid sparing effect in children undergoing urologic procedures when it was injected at doses of 1 μg·kg−1 followed by a continuous infusion of 0.7 μg·kg−1·hr−1.25 The findings in our study of children undergoing tonsillectomy are also in concert with those reporting that dexmedetomidine administered as a bolus (2 μg·kg−1) followed by a continuous infusion of 0.7 μg·kg−1·hr−1 decreases emergence agitation and the proportion of patients requiring morphine rescue.11 Therefore, it appears that there might be a role for dexmedetomidine to treat pain after tonsillectomy.
It is intriguing, however, that dexmedetomidine has been shown to decrease opioid requirement and prolong opioid-free interval when it is given at higher doses and compared with fentanyl but not when it is compared with morphine. While the reasons for these discrepant results are unclear, one could postulate that the following factors could have contributed to discrepancies in the results: differences in dexmedetomidine doses (we used dexmedetomidine doses two to eight times higher than those used in other studies)10,22; differences in pharmacokinetics (short vs long half-life) of the opioids (morphine vs fentanyl) compared with dexmedetomidine; and the possibility that the pharmacokinetics of dexmedetomidine are different when administered in very high doses rather than in smaller doses. Nevertheless, our study and others suggest that higher doses of dexmedetomidine delay the need for opioid rescue and have an opioid-sparing effect compared with short-acting opioids.
We did not address the clinical relevance and impact of delaying the need for analgesia for the first eight to ten hours, in morbidity after tonsillectomy; however, one could postulate that increasing the opioid-free interval in the postoperative period, even if only for several hours, could benefit children undergoing tonsillectomy. This hypothesis is worthy of further studies given the circumstantial evidence that delaying administration of opioids might decrease morbidity. For example, researchers have shown that: half of the medical interventions performed to treat respiratory morbidity are needed within the first hour after tonsillectomy15; children with obstructive sleep apnea have increased sensitivity to opioids; respiratory complications after adenotonsillectomy are often seen within two hours of opioid administration15,16; and the need for major medical interventions to treat respiratory complications is reduced significantly when high-risk children undergoing adenotonsillectomy receive fewer opioids.13 Therefore, while one could postulate that the opioid-sparing effects of dexmedetomidine might be desirable and beneficial to a high-risk population of patients with obstructive sleep apnea presenting for tonsillectomy, testing these hypotheses warrants further study.
One must be circumspect about the interpretation of our findings. For example, a high dose (4 μg·kg−1) of dexmedetomidine rather than a lower dose (2 μg·kg−1) appears to prolong time to emergence with an associated uncorrected P value of 0.0343. Some would argue that this comparison of drug differences and dosage differences “a priori” should use an uncorrected alpha of 0.05 (Kirk, 1995; Sokal and Rohlf, 1995) for assessing significance. Others who always correct for multiplicity (Bland and Altman, 1995) would argue that a correction for multiple comparisons should be used in order to maintain a family-wise alpha of 0.05, which in turn would make the finding statistically non-significant. Nevertheless, while some might question the statistical significance of the finding, prolongation of time to emergence associated with sedation might still be clinically relevant. Nevertheless, at a minimum, our finding (i.e., high-dose dexmedetomidine prolongs time to emergence compared with lower doses) generates a hypothesis worthy of being tested in future studies.
Interestingly, in ad-hoc analysis, we found that males are at a higher risk than females to require morphine rescue. While we did not design a study to explore sex-related differences in opioid requirements, these findings are interesting given that little is known about sex-related differences in opioid requirement in children. However, in adults, some clinical studies suggest that males have higher opioid requirements than females after surgical procedures,26,27 and there are sex differences in opioid analgesia.28 In this investigation, we did not examine the relevance, mechanisms, or explanation of the finding that boys are more likely to require opioids than girls after tonsillectomies. However, this finding does suggest that the effect of sex should be explored further in studies of acute pain in children as it has been done in adults.
We also observed the effects of dexmedetomidine on hemodynamic variables. Children treated with dexmedetomidine had fewer increases in heart rate and blood pressure at times known to elicit significant hemodynamic responses (placement of the mouth gag and surgical incision) during tonsillectomies. Others have shown that dexmedetomidine can attenuate the hemodynamic response to laryngoscopy and endotracheal intubation in adults undergoing cardiac surgery, and it can ameliorate the hemodynamic and neuroendocrine stress response associated with sternotomy and cardiopulmonary bypass.29,30 While we found that children treated with dexmedetomidine had lower heart rates and blood pressure readings compared with those treated with fentanyl, these changes were clinically well-tolerated, they were resolved spontaneously, and they did not warrant pharmacologic intervention. Therefore, it is our view that dexmedetomidine might have a role in preventing heart rate and blood pressure increases elicited by surgical maneuvers know to be associated with profound hemodynamic effects.
Finally, we found that dexmedetomidine prolonged time to emergence from anesthesia and increased PACU length of stay. While this prolongation in time to emergence from anesthesia may have played a role in the delay in morphine rescue requirement, it appears that the opioid-sparing effect is present even after controlling for the increase in time to emergence from anesthesia. The finding of prolongation of PACU length of stay by approximately 15 to 20 min (25% to 50%) on average is intriguing given our findings of desirable outcomes, such as improved pain control, decreased opioid requirements, and better hemodynamic profile. Why and how might dexmedetomidine be associated with longer PACU stay? We postulate that children in the dexmedetomidine groups were significantly less agitated, which might have been interpreted as unexpected sedation after anesthesia and thereby prompted prolongation of PACU stay. As we did not design the trial to examine the reasons for prolonged PACU stay, further investigations are needed to understand the reasons for this finding. While statistically significant, the prolongation of PACU stay appears to be of modest clinical relevance, although it might become a concern when consideration of cost-benefit ratio is entertained.
In conclusion, and most importantly, we found that higher doses of dexmedetomidine, a selective α2 adrenoreceptor agonist, prolongs opioid-free intervals and decreases opioid rescue requirements after tonsillectomy. These effects are desirable and might be of benefit for a patient population at increased risk for respiratory complications associated with the use of opioids, such as those associated with obstructive sleep apnea syndrome.
Notes
A. Hintze JL. PASS USER’S Guide. Pass 2008, Power Analysis and Sample Size for Windows, 2008.
References
Vestergaard H, Wohlfahrt J, Westergaard T, Pipper C, Rasmussen N, Melbye M. Incidence of tonsillectomy in Denmark, 1980 to 2001. Pediatr Infect Dis J 2007; 26: 1117-21.
Erickson BK, Larson DR, St Sauver JL, Meverden RA, Orvidas LJ. Changes in incidence and indications of tonsillectomy and adenotonsillectomy, 1970-2005. Otolaryngol Head Neck Surg 2009; 140: 894-901.
Bhattacharyya N. Ambulatory pediatric otolaryngologic procedures in the United States: characteristics and perioperative safety. Laryngoscope 2010; 120: 821-5.
Bean-Lijewski JD, Kruitbosch SH, Hutchinson L, Browne B. Post-tonsillectomy pain management in children: can we do better? Otolaryngol Head Neck Surg 2007; 137: 545-51.
Mather SJ, Peutrell JM. Postoperative morphine requirements, nausea and vomiting following anaesthesia for tonsillectomy. Comparison of intravenous morphine and non-opioid analgesic techniques. Paediatr Anaesth 1995; 5: 185-8.
Watters CH, Patterson CC, Mathews HM, Campbell W. Diclofenac sodium for post-tonsillectomy pain in children. Anaesthesia 1988; 43: 641-3.
Korpela R, Korvenoja P, Meretoja OA. Morphine-sparing effect of acetaminophen in pediatric day-case surgery. Anesthesiology 1999; 91: 442-7.
Unal Y, Pampal K, Korkmaz S, Arslan M, Zengin A, Kurtipek O. Comparison of bupivacaine and ropivacaine on postoperative pain after tonsillectomy in paediatric patients. Int J Pediatr Otorhinolaryngol 2007; 71: 83-7.
Atef A, Fawaz AA. Peritonsillar infiltration with tramadol improves pediatric tonsillectomy pain. Eur Arch Otorhinolaryngol 2008; 265: 571-4.
Olutoye O, Kim T, Giannoni C, Stayer S. Dexmedetomidine as an analgesic for pediatric tonsillectomy and adenoidectomy. Paediatr Anaesth 2007; 17: 1007-8.
Patel A, Davidson M, Tran MC, et al. Dexmedetomidine infusion for analgesia and prevention of emergence agitation in children with obstructive sleep apnea syndrome undergoing tonsillectomy and adenoidectomy. Anesth Analg 2010; 111: 1004-10.
Nixon GM, Kermack AS, McGregor CD, et al. Sleep and breathing on the first night after adenotonsillectomy for obstructive sleep apnea. Pediatr Pulmonol 2005; 39: 332-8.
Raghavendran S, Bagry H, Detheux G, Zhang X, Brouillette RT, Brown KA. An anesthetic management protocol to decrease respiratory complications after adenotonsillectomy in children with severe sleep apnea. Anesth Analg 2010; 110: 1093-101.
Wilson K, Lakheeram I, Morielli A, Brouillette R, Brown K. Can assessment for obstructive sleep apnea help predict postadenotonsillectomy respiratory complications? Anesthesiology 2002; 96: 313-22.
Brown KA, Morin I, Hickey C, Manoukian JJ, Nixon GM, Brouillette RT. Urgent adenotonsillectomy: an analysis of risk factors associated with postoperative respiratory morbidity. Anesthesiology 2003; 99: 586-95.
Brown KA, Laferriere A, Lakheeram I, Moss IR. Recurrent hypoxemia in children is associated with increased analgesic sensitivity to opiates. Anesthesiology 2006; 105: 665-9.
Hannallah RS, Broadman LM, Belman AB, Abramowitz MD, Epstein BS. Comparison of caudal and ilioinguinal/iliohypogastric nerve blocks for control of post-orchiopexy pain in pediatric ambulatory surgery. Anesthesiology 1987; 66: 832-4.
Watcha MF, Ramirez-Ruiz M, White PF, Jones MB, Lagueruela RG, Terkonda RP. Perioperative effects of oral ketorolac and acetaminophen in children undergoing bilateral myringotomy. Can J Anaesth 1992; 39: 649-54.
Steward DJ. A simplified scoring system for the post-operative recovery room. Can Anaesth Soc J 1975; 22: 111-3.
Mukherjee K, Esuvaranathan V, Streets C, Johnson A, Carr AS. Adenotonsillectomy in children: a comparison of morphine and fentanyl for peri-operative analgesia. Anaesthesia 2001; 56: 1193-7.
Lakatos E. Sample sizes based on the log-rank statistic in complex clinical trials. Biometrics 1988; 44: 229-41.
Olutoye OA, Glover CD, Diefenderfer JW, et al. The effect of intraoperative dexmedetomidine on postoperative analgesia and sedation in pediatric patients undergoing tonsillectomy and adenoidectomy. Anesth Analg 2010; 111: 490-5.
Koroglu A, Demirbilek S, Teksan H, Sagir O, But AK, Ersoy MO. Sedative, haemodynamic and respiratory effects of dexmedetomidine in children undergoing magnetic resonance imaging examination: preliminary results. Br J Anaesth 2005; 94: 821-4.
Venn RM, Hell J, Grounds RM. Respiratory effects of dexmedetomidine in the surgical patient requiring intensive care. Crit Care 2000; 4: 302-8.
Al-Zaben KR, Qudaisat IY, Al-Ghanem SM, et al. Intraoperative administration of dexmedetomidine reduces the analgesic requirements for children undergoing hypospadius surgery. Eur J Anaesthesiol 2010; 27: 247-52.
Weingarten TN, Sprung J, Flores A, Oviedo Baena AM, Schroeder DR, Warner DO. Opioid requirements after laparoscopic bariatric surgery. Obes Surg 2010; DOI:10.1007/s11695-010-0217-9.
Joels CS, Mostafa G, Matthews BD, et al. Factors affecting intravenous analgesic requirements after colectomy. J Am Coll Surg 2003; 197: 780-5.
Fillingim RB, Gear RW. Sex differences in opioid analgesia: clinical and experimental findings. Eur J Pain 2004; 8: 413-25.
Menda F, Koner O, Sayin M, Ture H, Imer P, Aykac B. Dexmedetomidine as an adjunct to anesthetic induction to attenuate hemodynamic response to endotracheal intubation in patients undergoing fast-track CABG. Ann Card Anaesth 2010; 13: 16-21.
Mukhtar AM, Obayah EM, Hassona AM. Preliminary experience with dexmedetomidine in pediatric anesthesia. Anesth Analg 2006; 103: 250.
Acknowledgements
The authors are indebted to the following individuals from Children’s National Medical Center, Washington, DC: Division of Otolaryngology: Nancy Bauman, MD, Maria Pena, MD, Diego Preciado, MD, Rahul Shah, MD and George Zalzal, MD for their help with this study; Division of Anesthesiology and Pain Medicine, Dianne Cochran, RN, Montagu Hankin and Kavita Nair for data collection and data management; Children’s Research Institute, Division of Biostatistics & Informatics: Karen Gold, Ph.D for critical comments and additional statistical analysis. The authors also thank Hospira (Lake Forest, IL) for graciously supplying dexmedetomidine for the clinical trial.
Funding
This study was supported, in part, by the Division of Anesthesiology and Pain Medicine, Sheikh Zayed Institute for Pediatric Surgical Innovation and by Hospira Inc., Lake Forest, IL (research support to Julia C. Finkel MD). Hospira Inc, manufacturer of dexmedetomidine, had no access to the data or its analysis and was not involved in manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pestieau, S.R., Quezado, Z.M.N., Johnson, Y.J. et al. High-dose dexmedetomidine increases the opioid-free interval and decreases opioid requirement after tonsillectomy in children. Can J Anesth/J Can Anesth 58, 540–550 (2011). https://doi.org/10.1007/s12630-011-9493-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-011-9493-7