Abstract
Background
Hypotension following spinal anesthesia for Cesarean delivery is common. Fluid loading is recommended to prevent hypotension, but preload is often ineffective. In non-pregnant patients, coloading has been shown to better maintain cardiac output after spinal anesthesia. The purpose of this meta-analysis was to determine whether the timing of the fluid infusion, before (preload) or during (coload) induction of spinal anesthesia for Cesarean delivery, influences the incidence of maternal hypotension or neonatal outcome.
Methods
We retrieved randomized controlled trials that compared a fluid preload with coload in patients undergoing spinal anesthesia for elective Cesarean delivery. We graded the articles for quality of reporting (maximum score = 5) and recorded the incidence of hypotension, lowest blood pressure, the incidence of maternal nausea and vomiting, umbilical cord pH, and Apgar scores. We combined the results using random effects modelling.
Results
We retrieved eight studies comprised of 518 patients. The median quality score for the published studies was three. The incidence of hypotension in the coload group was 159/268 (59.3%) compared with 156/250 (62.4%) in the preload group (odds ratio [OR] = 0.93; 95% confidence interval [CI] 0.54–1.6). There were no significant differences between groups in any of the other outcomes.
Conclusions
It is unnecessary to delay surgery in order to deliver a preload of fluid. Regardless of the fluid loading strategy, the incidence of maternal hypotension is high. Prophylactic or therapeutic vasopressors may be required in a significant proportion of patients.
Résumé
Contexte
L’hypotension est un phénomène courant à la suite d’une rachianesthésie pour un accouchement par césarienne. Il est recommandé d’administrer une charge liquidienne pour prévenir l’hypotension, mais la pré-charge est souvent peu efficace. Chez les patients et patientes non enceintes, il a été démontré que la co-charge maintenait mieux le débit cardiaque après une rachianesthésie. L’objectif de cette méta-analyse était de déterminer si le moment de perfusion liquidienne, soit avant (pré-charge) ou pendant (co-charge) l’induction de la rachianesthésie pour un accouchement par césarienne, influençait l’incidence d’hypotension chez la mère ou le devenir du nouveau-né.
Méthode
Nous avons extrait des études randomisées contrôlées comparant une pré-charge à une co-charge liquidienne chez des patientes subissant une rachianesthésie pour un accouchement par césarienne non urgent. Nous avons attribué une note aux articles selon la qualité de la présentation (score maximal = 5) et noté l’incidence d’hypotension, la tension artérielle la plus basse, l’incidence de nausées et vomissements chez la mère, le pH du sang du cordon ombilical et les scores d’Apgar. Nous avons combiné les résultats à l’aide d’un modèle à effets aléatoires.
Résultats
Nous avons retenu huit études comprenant 518 patientes. Le score de qualité médian des études publiées était de trois. L’incidence d’hypotension dans le groupe co-charge était de 159/268 (59,3 %) par rapport à 156/250 (62,4 %) dans le groupe pré-charge (rapport de cotes [RC] = 0,93; intervalle de confiance [IC] 95 % 0,54 à 1,6). Il n’y a pas eu de différence significative entre les groupes pour tous les autres critères d’évaluation.
Conclusion
Il n’est pas nécessaire de retarder la chirurgie pour permettre l’administration d’une pré-charge liquidienne. Quelle que soit la stratégie de charge liquidienne, l’incidence d’hypotension maternelle demeure élevée. Des agents vasopresseurs en prophylaxie ou comme traitement pourraient être nécessaires chez une proportion importante de patientes.
Similar content being viewed by others
Introduction
Spinal anesthesia is commonly used for elective Cesarean delivery, but maternal hypotension remains a common complication that may result in maternal side effects, such as nausea and vomiting, or neonatal side effects relating to asphyxia. Early reports suggested that this complication could be prevented by infusing a bolus of fluid before induction of anesthesia,1 but this strategy, along with others that increase central blood volume, has met with limited success.2 Other measures, such as the use of therapeutic or prophylactic vasopressors, have not been uniformly successful.3 Traditionally, crystalloid intravenous fluids were administered before the induction of spinal anesthesia for Cesarean delivery (preload).4 In non-pregnant patients, coloading has been shown to better maintain cardiac output after spinal anesthesia.5 Recently, some authors have suggested that fluid administration should take place at the time of induction of anesthesia for Cesarean delivery.6 The purpose of this meta-analysis is to determine whether the timing of the fluid infusion, i.e., before or during induction of spinal anesthesia for Cesarean delivery, influences the incidence of maternal hypotension or adverse neonatal outcome.
Methods
Literature review
We sought randomized controlled trials (RCTs) in patients scheduled for elective Cesarean delivery that compared fluid administration before induction of spinal anesthesia (preloading) with fluid administration at the time of induction of spinal anesthesia (coloading). We included articles that employed either colloid or crystalloid fluids, but we did not include articles that compared these fluids. Articles were retrieved from MEDLINE, EMBASE, and LILACS (Jan 1980 until May 2009) using the following key words and text words with alternate spellings: elective, Cesarean section, anesthesia, spinal, preload or preloading, coload or coloading (see Table 1 for search strategy and results from MEDLINE and EMBASE). We also searched the bibliographies of relevant reviews and identified RCTs. In addition, we searched for and reviewed published abstracts from relevant anesthesia meetings that were held during 2000 to 2009 by the American Society of Anesthesiologists, the Society of Obstetric Anesthesia and Perinatology, and the European Society of Anaesthesia. Finally, we contacted investigators if the dataset was incomplete. The search was completed by all authors and the results were compared. The final list of qualifying studies was derived by consensus. There was no language restriction.
Quality of the trials
Two of the authors (AB, RMS) scored each trial independently using a five-point validated quality index.7 This index consisted of two points for appropriate reporting of randomization, two points for appropriate reporting of blinding, and one point for reporting the outcome of all recruited patients. The two authors reviewed the articles and assigned a final score by consensus when the initial scores differed. In addition, they noted studies where there was blinding to allocation.
Publication bias
A funnel plot can be used for assessing publication bias.8 This plot is a graph with effect size on the x axis and a measure of sample size (in this case the log of the standard error of the effect size) on the y axis. If small trials are inappropriately represented, the plot will appear to be asymmetrical. In addition, we inspected the Clinical Trials Registry website (http://clinicaltrials.gov/ last accessed September 14, 2009) for unpublished data using a broad search strategy (preload and spinal anesthesia).
Outcome measurements
The primary outcome was the incidence of hypotension as defined by the authors. The secondary outcomes were the lowest blood pressure recorded, the incidence of nausea and vomiting, umbilical arterial pH, total volume of fluid administered, and the dose of vasoconstrictor used.
Data management
Data were recorded independently by two of the authors (AB, RMS) to avoid transcription errors, with any discrepancies resolved by reinspection of the original articles. The data were then entered into the statistical program (by AB) and rechecked (by RMS).
Analysis
The study characteristics are presented in tabular form. Meta-analytic techniques (MetaView software, Revman 4.2 and 5.0, Cochrane Library, Oxford, England) were used where possible to combine the results of the randomized controlled trials. For dichotomous variables, the OR and 95% CI were calculated using a random effects model. A statistically significant difference occurred when the 95% CI did not include 1.0. We also calculated the risk difference and 95% CI for the primary outcome to provide clinical context. For continuous variables, the standardized mean difference and 95% CI were calculated using random effects modelling. A statistically significant difference occurred when the 95% CI did not include 0. Heterogeneity was assessed using the I 2 statistic. The I 2 statistic describes the percentage of total variation in study findings that is due to between study differences rather than due to chance.9
Subgroup analysis
A subgroup analysis was performed for the primary outcome according to the type of fluid (colloid or crystalloid) used in the study.
Results
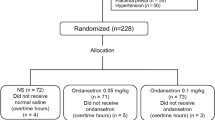
The flow diagram showing the search results is shown in Fig. 1. We retrieved six manuscripts using the search strategy described.10 – 15 One of these manuscripts compared a group that received fluid at the time of induction of anesthesia (coload) with a group that received a bolus both before and at the time of induction.15 This study was omitted from the analysis. We found three additional references in abstract form.16 – 18 Thus, we retrieved eight randomized controlled trials with a total of 518 patients. There was no evidence of publication bias seen in the funnel plot (Fig. 2). There are no studies in the clinical trials registry that are ongoing or contain unreported data.
The median quality score for the full manuscripts was 3 (range 2–5). Four of the studies were not blinded 11 – 13 , 17 and two did not completely describe the randomization process.10 , 12 Two of the studies did not describe blinding of allocation.10 , 13 The study characteristics are shown in Table 2.
Incidence of hypotension
Hypotension was defined by the authors as a 20% reduction of systolic blood pressure from baseline in five studies,10 – 13 , 16 a 20% reduction and a systolic blood pressure less than 100 mmHg in one study,18 and a reduction of 10% in two studies.14 , 17 The incidence of hypotension in the coload group was 159/268 (59.3%) compared with 156/250 (62.4%) in the preload group (OR 0.93; 95% CI 0.54, 1.6). The incidence of hypotension in each study and the pooled incidence are shown in Fig. 3. The pooled risk difference between groups was 1.0% (95% CI −10% to 8%) favouring coload but was not statistically significant. There was no significant heterogeneity among the studies (I 2 = 0.31; P = 0.18).
Similar results were found when hypotension was examined in the fluid subgroups, i.e., OR 0.9; 95% CI 0.43–1.86 in the crystalloid studies and OR 0.99; 95% CI 0.37–2.67 in the colloid studies.
The secondary outcomes are shown in Table 3. Because various drugs, drug combinations, and drug concentrations were used by investigators as vasopressors, we reported the results of this outcome as “standardized units”. This was either the number of mg of vasopressor or the number of mL, depending on the method the authors used to report this outcome. There was no significant difference between the two treatment groups in any of the outcomes.
Discussion
Early studies showed that a preload of 1 litre of crystalloid initiated about 30 min before induction of anesthesia was fully effective in preventing hypotension when compared with no fluid load.1 , 19 However, this has not been confirmed by other investigators. A recent systematic review found ten randomized controlled trials performed to determine the effectiveness of crystalloid preload.2 As defined by the authors, these studies reported a median incidence of hypotension of 46% in the crystalloid preload group. Colloid preload was somewhat better (38%).
Preloading may be unsuccessful in reducing the incidence of hypotension for a number of reasons. Early fluid loading may not effectively increase the intravascular volume at the time of maximum vasodilation. Volunteer studies have shown that a rapid infusion of lactated Ringers solution increases the intravascular volume by about 10%. This decreases rapidly when the infusion is discontinued.20 Preloading may induce atrial stretching, releasing atrial natriuretic peptide.21 Since natriuretic peptide type C is a potent vasodilator produced in the endothelium of great vessels,22 rapid fluid administration (whether before or during induction of anesthesia) may exacerbate peripheral vasodilation and facilitate fluid excretion. Finally, prehydration affects the distribution of local anesthetics in the cerebrospinal fluid (CSF) by changing the CSF circulation.23 Whether this affects the incidence of hypotension has not been determined.
Because fluid is rapidly lost from the intravascular compartment, it may be rational to initiate a rapid infusion immediately after induction of spinal anesthesia. Hahn et al. demonstrated that colloid and crystalloid are less efficient in expanding the functional volume than previously thought. In particular, much of the blood volume may be sequestered in the legs. They also postulate that fluid does not return to the functional compartment from the interstitium in spite of central hypovolemia. Therefore, it would be desirable to rapidly infuse fluid immediately after the block has been placed to maximize the amount of fluid in the functional compartment.24 Fluid enhances cardiac output and stroke volume but only transiently. These parameters are equal whether preload or coload is given within 10 min of induction of spinal anesthesia.14
In this review, we were unable to conclude that the time of fluid loading, either before or during induction of spinal anesthesia, affected the incidence of hypotension or other side effects in patients undergoing elective Cesarean delivery. None of the eight studies we retrieved that involved a total of 518 patients showed a statistically significant difference in the incidence of hypotension between groups. Only one study showed a reduced requirement for vasopressor in the coload group. Of interest, this study used the highest infusion volume, i.e., 20 mL · kg−1 of crystalloid.12
While there are insufficient data to conclude that fluid preloading is equivalent to coload, the difference in the incidence of hypotension between the groups is consistently small. In addition, there were no statistically (or clinically) significant differences in any of the other side effects reported. These data give further support to the recent American Society of Anesthesiologists (ASA) clinical practice guideline recommendation concerning spinal anesthesia for Cesarean delivery that states, “Although fluid preloading reduces the frequency of maternal hypotension, initiation of spinal anesthesia should not be delayed to administer a fixed volume of intravenous fluid.” 25 It should be noted that all of the studies in this review were done on patients undergoing elective Cesarean delivery and may not apply to emergency situations.
This review has several limitations. The majority of the studies are small. Combining small studies may give misleading information if many of them were not published (publication bias). This is unlikely, since the most common reason for failure to publish is the inability to demonstrate a statistical difference between groups.26 None of the studies in this review demonstrated a statistical difference; nevertheless, they were published. In addition, none of the usual methods used for detecting publication bias were positive. A second limitation is the heterogeneity in the secondary outcomes. In particular, there was significant heterogeneity in the amount of vasopressor used to treat hypotension. This can be accounted for by noting the clinical differences in the vasopressor drugs and the protocols for their use. A third limitation is our decision to combine all fluid volumes into one analysis. As a result, an effect size for each bolus size could not be established. However, the studies in our meta-analysis were relatively homogenous and used fluid boluses in the range of 1000–1500 mL of crystalloid or 500–1000 mL of colloid. If significant heterogeneity had appeared, we would have performed a sensitivity analysis to consider the effect of volume of fluid.
In summary, in patients undergoing elective Cesarean delivery under spinal anesthesia, the timing of fluid loading does not have an impact on the incidence of hypotension. This is true for both colloid and crystalloid loading. Therefore, it is unnecessary to delay surgery in order to deliver a preload of fluid. Regardless of the fluid loading strategy, either prophylactic or therapeutic vasopressors may be required in a significant proportion of patients.
References
Marx GF, Cosmi EV, Wollman SB. Biochemical status and clinical condition of mother and infant at Cesarean section. Anesth Analg 1969; 48: 986–94.
Morgan PJ, Halpern SH, Tarshis J. The effects of an increase of central blood volume before spinal anesthesia for Cesarean delivery: a qualitative systematic review. Anesth Analg 2001; 92: 997–1005.
Ngan Kee WD, Khaw KS, Ng FF, Lee BB. Prophylactic phenylephrine infusion for preventing hypotension during spinal anesthesia for Cesarean delivery. Anesth Analg 2004; 98: 815–21.
Hughes SC, Levinson G, Rosen MA. Anesthesia for Cesarean section. In: Hughes SC, Levinson G, Rosen MA, editors. Shnider and Levinson’s Anesthesia for Obstetrics. 4th ed. Philadelphia: Lippincott Williams Wilkins; 2002. p. 201.
Kamenik M, Paver-Erzen V. The effects of lactated Ringer’s solution infusion on cardiac output changes after spinal anesthesia. Anesth Analg 2001; 92: 710–4.
Tsen LC. Anesthesia for Cesarean delivery. In: Chestnut DH, Polley LS, Tsen LC, Wong CA, editors. Chestnut’s Obstetric Anesthesia: Principles and Practice, 4th ed. Philadelphia: Mosby Elsiever; 2009. p. 512.
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996; 17: 1–12.
Haynes RB. Conducting systematic reviews. In: Haynes RB, Sackett DL, Guyatt GH, Tugwell P, editors. Clinical Epidemiology: How to do Clinical Practice Research. 3rd ed. Philadelphia, PA: Lippincott, Williams and Wilkins; 2006. p. 15–47.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21: 1539–58.
Cardoso MM, Santos MM, Yamaguchi ET, Hirahara JT, Amaro AR. Fluid preload in obstetric patients. how to do it? (Portuguese). Rev Bras Anestesiol 2004; 54: 13–9.
Carvalho B, Mercier FJ, Riley ET, Brummel C, Cohen SE. Hetastarch co-loading is as effective as pre-loading for the prevention of hypotension following spinal anesthesia for Cesarean delivery. Int J Obstet Anesth 2009; 18: 150–5.
Dyer RA, Farina Z, Joubert IA, et al. Crystalloid preload versus rapid crystalloid administration after induction of spinal anaesthesia (coload) for elective caesarean section. Anaesth Intensive Care 2004; 32: 351–7.
Nishikawa K, Yokoyama N, Saito S, Goto F. Comparison of effects of rapid colloid loading before and after spinal anesthesia on maternal hemodynamics and neonatal outcomes in Cesarean section. J Clin Monit Comput 2007; 21: 125–9.
Teoh WH, Sia AT. Colloid preload versus coload for spinal anesthesia for Cesarean delivery: the effects on maternal cardiac output. Anesth Analg 2009; 108: 1592–8.
Williamson W, Burks D, Pipkin J, Burkard JF, Osborne LA, Pellegrini JE. Effect of timing of fluid bolus on reduction of spinal-induced hypotension in patients undergoing elective Cesarean delivery. AANA J 2009; 77: 130–6.
Bouchnak M, Ben Cheikg N, Skhiri A, et al. Relevance of rapid crystalloid administration after spinal anaesthesia (coload) in prevention of hypotension during elective caesarean section: A685. Eur J Anaesthesiol 2006; 23: 178.
Mercier FJ, Roger-Christoph S, des Mesnard-Smaja V, et al. Crystalloid pre-loading vs post-loading for the prevention of hypotension with spinal anesthesia for Cesarean delivery. Anesthesiology; 2004; 100: A18.
Siddik-Sayyid SM, Zbeidy RA. Colloid prehydration versus colloid cohydration during spinal anesthesia for Cesarean delivery. Anesthesiology 2008; 109: A1128.
Wollman SB, Marx GF. Acute hydration for prevention of hypotension of spinal anesthesia in parturients. Anesthesiology 1968; 29: 374–80.
Hahn RG, Svensen C. Plasma dilution and the rate of infusion of Ringer’s solution. Br J Anaesth 1997; 79: 64–7.
Pouta AM, Karinen J, Vuolteenaho OJ, Laatikainen TJ. Effect of intravenous fluid preload on vasoactive peptide secretion during caesarean section under spinal anaesthesia. Anaesthesia 1996; 51: 128–32.
Suga S, Nakao K, Itoh H, et al. Endothelial production of C-type natriuretic peptide and its marked augmentation by transforming growth factor-beta. Possible existence of “vascular natriuretic peptide system”. J Clin Invest 1992; 90: 1145–9.
Shin BS, Ko JS, Gwak MS, et al. The effects of prehydration on the properties of cerebrospinal fluid and the spread of isobaric spinal anesthetic drug. Anesth Analg 2008; 106: 1002–7.
Hahn RG, Resby M. Volume kinetics of ringer’s solution and dextran 3% during induction of spinal anaesthesia for caesarean section. Can J Anaesth 1998; 45: 443–51.
American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Practice guidelines for obstetric anesthesia: an updated report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Anesthesiology 2007; 106: 843–63.
Dickersin K, Min YI, Meinert CL. Factors influencing publication of research results. Follow-up of applications submitted to two institutional review boards. JAMA 1992; 267: 374–8.
Funding
Departmental funds.
Competing interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Banerjee, A., Stocche, R.M., Angle, P. et al. Preload or coload for spinal anesthesia for elective Cesarean delivery: a meta-analysis. Can J Anesth/J Can Anesth 57, 24–31 (2010). https://doi.org/10.1007/s12630-009-9206-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-009-9206-7