Abstract
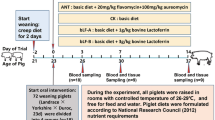
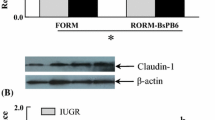
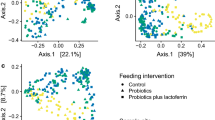
The aim of this study was to determine the effects of early-life bovine lactoferrin and host specific probiotic interventions on growth performance, mortality, and concentrations of immunoglobulin A and immunoglobulin G and transforming growth factor beta 1 (a marker of intestinal integrity) in serum of neonatal piglets. A total of eight piglet litters from parity matched sows were randomly divided into four groups and assigned to one of the four interventions: control (sterile normal saline), bovine lactoferrin (100 mg bovine lactoferrin), probiotic (1 × 109 colony forming unit (cfu) of swine origin Pediococcus acidilactici FT28 probiotic), and bovine lactoferrin + probiotic (100 mg bovine lactoferrin and 1 × 109 CFU of P. acidilactici FT28 probiotic). All the interventions were given once daily through oral route for first 7 days of life. The average daily gain (p = 0.0004) and weaning weight (p < 0.0001) were significantly improved in the probiotic group. The piglet survivability was significantly higher in bovine lactoferrin and probiotic groups than control group in Log-rank (Mantel-Cox) test. The concentrations of immunoglobulin A on day 21 in bovine lactoferrin, probiotic, and bovine lactoferrin + probiotic groups increased significantly (p < 0.05). Immunoglobulin G concentrations on day 7 and 15 in bovine lactoferrin and bovine lactoferrin + probiotic groups and on day 15 in probiotic group were significantly (p < 0.05) elevated, whereas, the concentration of transforming growth factor-β1 was significantly (p < 0.05) increased from day 7 to 21 in all the supplemented groups. In conclusion, the early-life bovine lactoferrin and P. acidilactici FT28 probiotic interventions reduced the mortality in the suckling piglets by promoting the systemic immunity and enhancing the intestinal integrity.



Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sell-Kubiak E (2021) Selection for litter size and litter birthweight in Large White pigs: maximum, mean and variability of reproduction traits. Animal 15:100352. https://doi.org/10.1016/j.animal.2021.100352
Cabrera RA, Lin X, Campbell JM, Moeser AJ, Odle J (2012) Influence of birth order, birth weight, colostrum and serum immunoglobulin G on neonatal piglet survival. J Anim Sci Biotechnol 3:1–10. https://doi.org/10.1186/2049-1891-3-42
Butler JE, Zhao Y, Sinkora M, Wertz N, Kacskovics I (2009) Immunoglobulins, antibody repertoire and B cell development. Dev Comp Immunol 33:321–333. https://doi.org/10.1016/j.dci.2008.06.015
Salmon H, Berri M, Gerdts V, Meurens F (2009) Humoral and cellular factors of maternal immunity in swine. Dev Comp Immunol 33:384–393. https://doi.org/10.1016/j.dci.2008.07.007
Hurley WL, Theil PK (2011) Perspectives on immunoglobulins in colostrum and milk. Nutrients 3:442–474. https://doi.org/10.3390/nu3040442
Navarro E, Mainau E, de Miguel R, Temple D, Salas M, Manteca X (2021) Oral meloxicam administration in sows at farrowing and its effects on piglet immunity transfer and growth. Front Vet Sci 8:72. https://doi.org/10.3389/fvets.2021.574250
Walker WA (2013) Initial intestinal colonization in the human infant and immune homeostasis. Ann Nutr Metab 63:8–15. https://doi.org/10.1159/000354907
Isaacson R, Kim HB (2012) The intestinal microbiome of the pig. Anim Health Res Rev 13:100. https://doi.org/10.1017/S1466252312000084
Pajarillo EA, Chae JP, Balolong MP, Kim HB, Kang DK (2014) Assessment of fecal bacterial diversity among healthy piglets during the weaning transition. J Gen Appl Microbiol 60:140–146. https://doi.org/10.2323/jgam.60.140
Chen X, Xu J, Ren E, Su Y, Zhu W (2018) Co-occurrence of early gut colonization in neonatal piglets with microbiota in the maternal and surrounding delivery environments. Anaerobe 49:30–40. https://doi.org/10.1016/j.anaerobe.2017.12.002
Bauche D, Marie JC (2017) Transforming growth factor β: a master regulator of the gut microbiota and immune cell interactions. Clin Transl Immunol 6:e136. https://doi.org/10.1038/cti.2017.9
Stolfi C, Troncone E, Marafini I, Monteleone G (2021) Role of TGF-beta and Smad7 in gut inflammation, fibrosis and cancer. Biomolecules 11:17. https://doi.org/10.3390/biom11010017
Mei J, Xu RJ (2005) Transient changes of transforming growth factor-β expression in the small intestine of the pig in association with weaning. Br J Nutr 93:37–45. https://doi.org/10.1079/BJN20041302
Xu R, Wan J, Lin C, Su Y (2020) Effects of early intervention with antibiotics and maternal faecal microbiota on transcriptomic profiling ileal mucosa in neonatal pigs. Antibiotics 9:35. https://doi.org/10.3390/antibiotics9010035
Bian G, Ma S, Zhu Z, Su Y, Zoetendal EG, Mackie R, Liu J, Mu C, Huang R, Smidt H, Zhu W (2016) Age, introduction of solid feed and weaning are more important determinants of gut bacterial succession in piglets than breed and nursing mother as revealed by a reciprocal cross-fostering model. Environ Microbiol 18:1566–1577. https://doi.org/10.1111/1462-2920.13272
Chae JP, Pajarillo EA, Oh JK, Kim H, Kang DK (2016) Revealing the combined effects of lactulose and probiotic enterococci on the swine faecal microbiota using 454 pyrosequencing. Microb Biotechnol 9:486–495. https://doi.org/10.1111/1751-7915.12370
Hu Q, Liu C, Zhang D, Wang R, Qin L, Xu Q, Che L, Gao F (2020) Effects of low-dose antibiotics on gut immunity and antibiotic resistomes in weaned piglets. Front Immunol 11:903. https://doi.org/10.3389/fimmu.2020.00903
Paesano R, Berlutti F, Pietropaoli M, Pantanella F, Pacifici E, Goolsbee W, Valenti P (2010) Lactoferrin efficacy versus ferrous sulfate in curing iron deficiency and iron deficiency anemia in pregnant women. Biometals 23:411–417. https://doi.org/10.1007/s10534-010-9335-z
Comstock SS, Reznikov EA, Contractor N, Donovan SM (2014) Dietary bovine lactoferrin alters mucosal and systemic immune cell responses in neonatal piglets. J Nutr 144:525–532. https://doi.org/10.3945/jn.113.190264
Elbarbary HA, Ejima A, Sato K (2019) Generation of antibacterial peptides from crude cheese whey using pepsin and rennet enzymes at various pH conditions. J Sci Food Agric 99:555–563. https://doi.org/10.1002/jsfa.9214
Donker AE, van der Staaij H, Swinkels DW (2021) The critical roles of iron during the journey from fetus to adolescent: developmental aspects of iron homeostasis. Blood Rev 50:100866. https://doi.org/10.1016/j.blre.2021.100866
Zhao X, Zhang X, Xu T, Luo J, Luo Y, An P (2022) Comparative effects between oral lactoferrin and ferrous sulfate supplementation on iron-deficiency anemia: a comprehensive review and meta-analysis of clinical trials. Nutrients 14:543. https://doi.org/10.3390/nu14030543
Majka G, Śpiewak K, Kurpiewska K, Heczko P, Stochel G, Strus M, Brindell MA (2013) A high-throughput method for the quantification of iron saturation in lactoferrin preparations. Anal Bioanal Chem 405:5191–200. https://doi.org/10.1007/s00216-013-6943-9
Oguchi S, Walker WA, Sanderson IR (1995) Iron saturation alters the effect of lactoferrin on the proliferation and differentiation of human enterocytes (Caco-2 cells). Biol Neonate 67:330–339. https://doi.org/10.1159/000244182
Vega-Bautista A, de la Garza M, Carrero JC, Campos-Rodríguez R, Godínez-Victoria M, Drago-Serrano ME (2019) The impact of lactoferrin on the growth of intestinal inhabitant bacteria. Int J Mol Sci 20:4707. https://doi.org/10.3390/ijms20194707
Hu W, Zhao J, Wang J, Yu T, Wang J, Li N (2012) Transgenic milk containing recombinant human lactoferrin modulates the intestinal flora in piglets. Biochem Cell Biol 90:485–496. https://doi.org/10.1139/o2012-003
Hering NA, Luettig J, Krug SM, Wiegand S, Gross G, van Tol EA, Schulzke JD, Rosenthal R (2017) Lactoferrin protects against intestinal inflammation and bacteria-induced barrier dysfunction in vitro. Ann N Y Acad Sci 1405:177–188. https://doi.org/10.1111/nyas.13405
Karczewski J, Troost FJ, Konings I, Dekker J, Kleerebezem M, Brummer RJM, Wells JM (2010) Regulation of human epithelial tight junction proteins by Lactobacillus plantarum in vivo and protective effects on the epithelial barrier. Am J Physiol Gastrointest Liver Physiol 298:G851–G859. https://doi.org/10.1152/ajpgi.00327.2009
Ahrne S, Hagslatt ML (2011) Effect of lactobacilli on paracellular permeability in the gut. Nutrients 3:104–117. https://doi.org/10.3390/nu3010104
Davis ME, Parrott T, Brown DC, De Rodas BZ, Johnson ZB, Maxwell CV, Rehberger T (2008) Effect of a Bacillus-based direct-fed microbial feed supplement on growth performance and pen cleaning characteristics of growing-finishing pigs. J Anim Sci 86:1459–1467. https://doi.org/10.2527/jas.2007-0603
Wang AN, Yi XW, Yu HF, Dong B, Qiao SY (2009) Free radical scavenging activity of Lactobacillus fermentum in vitro and its antioxidative effect on growing–finishing pigs. J Appl Microbiol 107:1140–1148. https://doi.org/10.1111/j.1365-2672.2009.04294.x
Galdeano CM, De Leblanc ADM, Vinderola G, Bonet MB, Perdigon G (2007) Proposed model: mechanisms of immunomodulation induced by probiotic bacteria. Clin Vaccine Immunol 14:485–492. https://doi.org/10.1128/CVI.00406-06
Dowarah R, Verma AK, Agarwal N, Singh P (2016) Effect of swine-based probiotic on growth performance, nutrient utilization and immune status of early weaned grower-finisher crossbred pigs. Anim Nutr Feed Technol 16:451–461. https://doi.org/10.5958/0974-181X.2016.00042.1
Dowarah R, Verma AK, Agarwal N, Singh P, Singh BR (2018) Selection and characterization of probiotic lactic acid bacteria and its impact on growth, nutrient digestibility, health and antioxidant status in weaned piglets. PLoS ONE 13:e0192978. https://doi.org/10.1371/journal.pone.0192978
Dowarah R, Verma AK, Agarwal N, Patel BHM, Singh P (2017) Effect of swine-based probiotic on performance, diarrhoea scores, intestinal microbiota and gut health of grower-finisher crossbred pigs. Livest Sci 195:74–79. https://doi.org/10.1016/j.livsci.2016.11.006
Li Y, Hou S, Chen J, Peng W, Wen W, Chen F, Huang X (2019) Oral administration of Lactobacillus delbrueckii during the suckling period improves intestinal integrity after weaning in piglets. J Func Food 63:103591. https://doi.org/10.1016/j.jff.2019.103591
Li Y, Hou S, Peng W, Lin Q, Chen F, Yang L, Li F, Huang X (2019) Oral administration of Lactobacillus delbrueckii during the suckling phase improves antioxidant activities and immune responses after the weaning event in a piglet model. Oxid Med Cell Longev 2019:6919803. https://doi.org/10.1155/2019/6919803
Thacker PA (2013) Alternatives to antibiotics as growth promoters for use in swine production: a review. J Anim Sci Biotechnol 4:35. https://doi.org/10.1186/2049-1891-4-35
Muurinen J, Richert J, Wickware CL, Richert B, Johnson TA (2021) Swine growth promotion with antibiotics or alternatives can increase antibiotic resistance gene mobility potential. Sci Rep 11:1–3. https://github.com/sjmuurine/ZnCu
Vandenplas Y, Benninga M, Broekaert I, Falconer J, Gottrand F, Guarino A, Lifschitz C, Lionetti P, Orel R, Papadopoulou A (2016) Functional gastro-intestinal disorder algorithms focus on early recognition, parental reassurance and nutritional strategies. Acta Paediatr 105:244–252. https://doi.org/10.1111/apa.13270
Wang S, Yao B, Gao H, Zang J, Tao S, Zhang S, Huang S, He B, Wang J (2019) Combined supplementation of Lactobacillus fermentum and Pediococcus acidilactici promoted growth performance, alleviated inflammation, and modulated intestinal microbiota in weaned pigs. BMC Vet Res 15:1–11. https://doi.org/10.1186/s12917-019-1991-9
Pupa P, Apiwatsiri P, Sirichokchatchawan W, Pirarat N, Maison T, Koontanatechanon A, Prapasarakul N (2021) Use of Lactobacillus plantarum (strains 22F and 25F) and Pediococcus acidilactici (strain 72N) as replacements for antibiotic-growth promotants in pigs. Sci Rep 11:1–12. https://doi.org/10.1038/s41598-021-91427-5
English EA, Hopkins BA, Stroud JS, Davidson S, Smith G, Brownie C, Whitlow LW (2007) Lactoferrin supplementation to Holstein calves during the preweaning and postweaning phases. J Dairy Sci 90:5276–5281. https://doi.org/10.3168/jds.2007-0361
Geier MS, Torok VA, GuoP AGE, Boulianne M, Janardhana V, Bean AG, Hughes RJ (2011) The effects of lactoferrin on the intestinal environment of broiler chickens. Br Poult Sci 52:564–572. https://doi.org/10.1080/00071668.2011.607429
Shan T, Wang Y, Wang Y, Liu J, Xu Z (2007) Effect of dietary lactoferrin on the immune functions and serum iron level of weanling piglets. J Anim Sci 85:2140–2146. https://doi.org/10.2527/jas.2006-754
Hu P, Zhao F, Zhu W, Wang J (2019) Effects of early-life lactoferrin intervention on growth performance, small intestinal function and gut microbiota in suckling piglets. Food Funct 10:5361–5373. https://doi.org/10.1039/C9FO00676A
Wajda S, Smiecinska K, Jankowski J, Matusevicius P, Buteikis G (2010) The efficacy of lactic acid bacteria Pediococcus acidilactici, lactose and formic acid as dietary supplements for turkeys. Pol J Vet Sci 13:45. https://www.ncbi.nlm.nih.gov/pubmed/21077430
El Barbary M, Shady NA, Shaaban HA, Shaaban MA, Ahmed OY (2018) Effect of enteral bovine lactoferrin on neonatal iron status. Egypt J Haematol 43:212. https://doi.org/10.4103/ejh.ejh_30_18
Habing G, Harris K, Schuenemann GM, Piñeiro JM, Lakritz J, Clavijo XA (2017) Lactoferrin reduces mortality in preweaned calves with diarrhea. J Dairy Sci 100:3940–3948. https://doi.org/10.3168/jds.2016-11969
Joysowal M, Saikia BN, Dowarah R, Tamuly S, Kalita D, Choudhury KD (2018) Effect of probiotic Pediococcus acidilactici FT28 on growth performance, nutrient digestibility, health status, meat quality, and intestinal morphology in growing pigs. Vet World 11:1669. https://doi.org/10.14202/2Fvetworld.2018.1669-1676
Hu P, Zhao F, WangJ ZhuW (2020) Early-life lactoferrin intervention modulates the colonic microbiota, colonic microbial metabolites and intestinal function in suckling piglets. Appl Microbiol Biotechnol 104:6185–6197. https://doi.org/10.1007/s00253-020-10675-z
Washington IM, Van Hoosier G (2012) Clinical biochemistry and hematology. In The laboratory rabbit, guinea pig, hamster, and other rodents, Academic Press, Pp. 57–116. https://doi.org/10.1016/B978-0-12-380920-9.00003-1
Dong X, Zhang N, Zhou M, Tu Y, Deng K, Diao Q (2013) Effects of dietary probiotics on growth performance, faecal microbiota and serum profiles in weaned piglets. Anim Prod Sci 54:616–621. https://doi.org/10.1071/AN12372
Hu P, Zhao F, Wang J, Zhu W (2021) Metabolomic profiling reveals the effects of early-life lactoferrin intervention on protein synthesis, energy production and antioxidative capacity in the liver of suckling piglets. Food Funct 12:3405–3419. https://doi.org/10.1039/D0FO01747G
Al-Zubaidi HJ, Falih IB (2018) Immunological and pathological effect of lactoferrin against murine leishmaniasis. J Entomol Zool Stud 6:1108–1111. https://www.entomoljournal.com/archives/2018/vol6issue1/PartP/5-6-345-520.pdf
Sfeir RM, Dubarry M, Boyaka PN, Rautureau M, Tome D (2004) The mode of oral bovine lactoferrin administration influences mucosal and systemic immune responses in mice. J Nutr 134:403–409. https://doi.org/10.1093/jn/134.2.403
Jang YS, Seo GY, Lee JM, Seo HY, Han HJ, Kim SJ, Jin BR, Kim HJ, Park SR, Rhee KJ, Kim WS, Kim PH (2015) Lactoferrin causes IgA and IgG2b isotype switching through betaglycan binding and activation of canonical TGF-β signaling. Mucosal Immunol 8:906–917. https://doi.org/10.1038/mi.2014.121
Lee JM, Jang YS, Jin BR, Kim SJ, Kim HJ, Kwon BE, Ko HJ, Yoon SI, Lee GS, Kim WS, Seo GY, Kim PH, (2016) Retinoic acid enhances lactoferrin-induced IgA responses by increasing betaglycan expression. Cell Mol Immunol 13:862–870. https://doi.org/10.1038/cmi.2015.73
Yu LT, Ju CC, Ju J, Wu HL, Yen HT (2004) Effect of probiotics and selenium combination on the immune and blood cholesterol concentration of pigs. J Anim Feed Sci 13:625–634. https://doi.org/10.22358/jafs/67630/2004
Karamese M, Aydin H, Sengul E, Gelen V, Sevim C, Ustek D, Karakus E (2016) The immunostimulatory effect of lactic acid bacteria in a rat model. Iran J Immunol 13:220–228. http://iji.sums.ac.ir/article_33410_0.html
Aiyegoro O, Dlamini Z, Okoh A, Langa1 R (2017) Effects of probiotics on growth performance, blood parameters, and antibody stimulation in piglets. S Afr J Anim Sci 47:766-775. http://dx.doi.org/https://doi.org/10.4314/sajas.v47i6.4
Resendiz-Albor AA, Reina-Garfias H, Rojas-Hernandez S, Jarillo-Luna A, Rivera-Aguilar V, Miliar-Garcia A, Campos-Rodriguez R (2010) Regionalization of pIgR expression in the mucosa of mouse small intestine. Immunol Lett 128:59–67. https://doi.org/10.1016/j.imlet.2009.11.005
Naqid IA, Owen JP, Maddison BC, Gardner DS, Foster N, Tchórzewska MA, La Ragione RM, Gough KC (2015) Prebiotic and probiotic agents enhance antibody-based immune responses to Salmonella typhimurium infection in pigs. Anim Feed Sci Technol 201:57–65. https://doi.org/10.1016/j.anifeedsci.2014.12.005
Kim SH, Jeung W, Choi ID, Jeong JW, Lee DE, Huh CS, Kim GB, Hong SS, Shim JJ, Lee, Sim SH, JL, Ahn YT (2016) Lactic acid bacteria improve Peyer's patch cell-mediated immunoglobulin A and tight-junction expression in a destructed gut microbial environment. J Microbiol Biotechnol 26:1035–1045.https://doi.org/10.4014/jmb.1512.12002
Liu H, Wang S, Zhang D, Wang J, Zhang W, Wang Y, Ji H (2020) Effects of dietary supplementation with Pediococcus acidilactici ZPA017 on reproductive performance, fecal microbial flora and serum indices in sows during late gestation and lactation. Asian-Australas J Anim Sci 33:120. https://doi.org/10.5713/2Fajas.18.0764
Vadopalas L, Ruzauskas M, Lele V, Starkute V, Zavistanaviciute P, Zokaityte E, Bartkevics V, Pugajeva I, Reinolds I, Badaras S, Klupsaite D, Bartkiene E (2020) Combination of antimicrobial starters for feed fermentation: influence on piglet feces microbiota and health and growth performance, including mycotoxin biotransformation in vivo. Front Vet Sci 7:528990. https://doi.org/10.3389/2Ffvets.2020.528990
Al-Saiady MY (2010) Effect of probiotic bacteria on immunoglobulin G concentration and other blood components of newborn calves. J Anim Vet Adv 9:604–609. https://doi.org/10.3923/javaa.2010.604.609
Karamzadeh-Dehaghani A, Towhidi A, Zhandi M, Mojgani N, Fouladi-Nashta A (2021) Combined effect of probiotics and specific immunoglobulin Y directed against Escherichia coli on growth performance, diarrhea incidence, and immune system in calves. Animal 15:100124. https://doi.org/10.1016/j.animal.2020.100124
Troncone E, Marafini I, Stolfi C, Monteleone G (2018) Transforming growth factor-β1/Smad7 in intestinal immunity, inflammation, and cancer. Front Immunol 9:1407. https://doi.org/10.3389/fimmu.2018.01407
Gough NR, Xiang X, Mishra L (2021) TGF-β signaling in liver, pancreas, and gastrointestinal diseases and cancer. Gastroenterol 161:434-452.e15. https://doi.org/10.1053/j.gastro.2021.04.064
Hwang SA, Actor JK (2009) Lactoferrin modulation of BCG-infected dendritic cell functions. Int Immunol 21:1185–1197. https://doi.org/10.1093/intimm/dxp084
Lönnerdal B, Du X, Jiang R (2021) Biological activities of commercial bovine lactoferrin sources. Biochem Cell Biol 99:35–46. https://doi.org/10.1139/bcb-2020-0182
Monteleone G, Mann J, Monteleone I, Vavassori P, Bremner R, Fantini M, Del Vecchio BG, Tersigni R, Alessandroni L, Mann D, Pallone F, MacDonald TT (2004) A failure of transforming growth factor-beta1 negative regulation maintains sustained NF-kappaB activation in gut inflammation. J Biol Chem 279:3925–3932. https://doi.org/10.1074/jbc.m303654200
Sakai F, Hosoya T, Ono-Ohmachi A, Ukibe K, Ogawa A, Moriya T, Kadooka Y, Shiozaki T, Nakagawa H, Nakayama Y, Miyazaki T (2014) Lactobacillus gasseri SBT2055 induces TGF-β expression in dendritic cells and activates TLR2 signal to produce IgA in the small intestine. PLoS ONE 9:e105370. https://doi.org/10.1371/journal.pone.0105370
Huang IF, Lin IC, Liu PF, Cheng MF, Liu YC, Hsieh YD, Chen JJ, Chen CL, Chang HW, Shu CW (2015) Lactobacillus acidophilus attenuates Salmonella-induced intestinal inflammation via TGF-β signaling. BMC Microbiol 15:203. https://doi.org/10.1186/2Fs12866-015-0546-x
Barigela A, Bhukya B (2021) Probiotic Pediococcus acidilactici strain from tomato pickle displays anti-cancer activity and alleviates gut inflammation in-vitro. 3Biotech 11:1–11. https://doi.org/10.1007/s13205-020-02570-1
Foye OT, Huang IF, Chiou CC, Walker WA, Shi HN (2012) Early administration of probiotic Lactobacillus acidophilus and/or prebiotic inulin attenuates pathogen-mediated intestinal inflammation and Smad 7 cell signaling. FEMS Immunol Med Microbiol 65(3):467–80. https://doi.org/10.1111/2Fj.1574-695X.2012.00978.x
Acknowledgements
This work was supported by All India Network Programme on Neonatal Mortality project of ICAR. First author (VKS) thanks ICAR-IVRI for granting research fellowship for his research program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted. All procedures used during the research were approved by the Institute Animal Ethics Committee, and the research protocol was approved by the Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA), Ministry of Fisheries, Animal Husbandry and Dairying, Government of India (approval number V-11–11 (13)/19/2021-CPCSEA-DADF).
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Varun Kumar Sarkar and Ujjwal Kumar De are both first authors.
Rights and permissions
About this article
Cite this article
Sarkar, V.K., De, U.K., Kala, A. et al. Early-Life Intervention of Lactoferrin and Probiotic in Suckling Piglets: Effects on Immunoglobulins, Intestinal Integrity, and Neonatal Mortality. Probiotics & Antimicro. Prot. 15, 149–159 (2023). https://doi.org/10.1007/s12602-022-09964-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-022-09964-y