Abstract
Anorexia, a loss of appetite for food, can be caused by various physiological and pathophysiological conditions. In this review, firstly, clinical aspects of anorexia nervosa are summarized in brief. Secondly, hypothalamic neuropeptides responsible for feeding regulation in each hypothalamic nucleus are discussed. Finally, three different types of anorexigenic animal models; dehydration-induced anorexia, cisplatin-induced anorexia and cancer anorexia-cachexia, are introduced. In conclusion, hypothalamic neuropeptides may give us novel insight to understand and find effective therapeutics strategy essential for various kinds of anorexia.
Similar content being viewed by others
Introduction
Anorexia is caused by various physiological and pathophysiological conditions. Focusing on psychological eating disorders, the numbers of patients are increasing all over the world, among both men and women [1]. Eating disorders result in about 7,000 deaths a year (as of 2010) in the world, and therefore are a mental illness that results in substantial mortality [2]. Although, complexities of biological, psychological and/or environmental abnormalities are considered to be the cause of eating disorders, many things remain unknown. Investigating not only psychological aspects but also physiological aspects, including hypothalamic feeding-regulating neuropeptides, may be useful to understand its mechanism or to find effective therapeutics.
It is well established that appetite and feeding behaviors are primarily controlled by a feeding center and a satiety center in the hypothalamus, which is called the two-center theory [3–6]. Bilateral destruction of the ventromedial hypothalamus (VMH) produces a condition of voracious appetite, resulting in marked hyperphagia, which ultimately causes the animals to become remarkably obese [4]. On the other hand, bilateral destruction of the lateral hypothalamic area (LHA) produced an anorexic condition that results in animals failing to feed and ultimately wasting [6]. Although this two-center theory has been useful to understand the mechanisms of feeding behavior, it cannot be interpreted simply, because such ablation experiments may involve the destruction of many nerve fibers in the vicinity of those nuclei. For example, destruction of the LHA also damages the medial forebrain bundle, which includes abundant dopamine fibers responsible for feeding behavior and reward behavior.
Recently, the central mechanisms related to feeding behavior have been clarified on the basis of specific neuropeptides or neuronal networks rather than the two-center theory as previously described. The development of genetically modified mice using the Cre-loxP system enables us to examine the effects of specific neuronal cell populations on feeding behavior or body weight control [7]. In addition, functional neuronal mapping using optogenetics enables the identification of the neuronal circuits related to feeding control [8].
For a deeper understanding of the human eating disorders, it may be important to conduct experiments using anorexia animal models. Although anorexia, the eating disorder, in humans includes psychological problems as well as biological problems, it is difficult to imitate human eating disorders in animals. Various types of physiological and pathophysiological anorexia models have been proposed, although these models are not the same model as human anorexia because of its complexities of biological, psychological and/or environmental abnormalities. The typical models of physiological anorexia are dehydration-induced anorexia and stress-induced anorexia [9–12]. On the other hand, the typical models of pathophysiological anorexia are drug-induced anorexia, lipopolysaccharides (LPS)-induced anorexia, anti-cancer drug-induced anorexia as a side effect and cancer-induced cachexia-anorexia [13–15]. From the point of view of hypothalamic neuropeptides, distinct patterns of the orexigenic or anorexigenic neuropeptides are seen among these anorexia models. For example, dehydration-induced anorexia primarily causes up-regulation of the hypothalamic anorexigenic peptides, whereas LPS-induced anorexia causes down-regulation of orexigenic peptides in addition to the up-regulation of the anorexigenic peptides [16].
In the present review, we summarize the brief aspects of human anorexia nervosa and explain the points of hypothalamic neuropeptides responsible for feeding control. We also introduce three different types of anorexia animal model; dehydration-induced anorexia, cisplatin-induced anorexia and cancer anorexia-cachexia.
Complexity of human anorexia nervosa
In standard medical manuals such as ICD-10 or DSM-5, eating disorders are specified as mental disorders. The classification of the eating disorders and diagnostic criteria for anorexia nervosa are shown in Fig. 1.
Anorexia nervosa is characterized by food restriction, inappropriate eating habits or rituals, obsession with having a thin figure, and an irrational fear of weight gain. Often, “anorexia nervosa” and “anorexia” are used interchangeably, however, “anorexia” means simply lacking appetite and the majority of the patients with “anorexia nervosa” do not lose their appetite [17]. Anorexia nervosa is often coupled with a distorted self-image [17]. Patients often look at themselves as overweight even they are already underweight. Regardless of the feeling of continuous hunger, they restrict food due to their fear of gaining weight [18]. It is suggested the initial weight loss may in some cases be one of the triggering factors in developing anorexia nervosa, possibly because of an already inherent predisposition toward anorexia nervosa [19].
The history of anorexia nervosa begins with descriptions of religious fasting dating from the Hellenistic era and continuing into the medieval period [20]. The earliest medical descriptions of anorexic illnesses were shown by English physician Richard Morton in 1689 [20]. Many case descriptions considered to be anorexic illnesses were demonstrated until nineteenth century. The term “anorexia nervosa” [of Greek origin: an- (prefix denoting negation) and orexis (“appetite”)], was coined in 1873 by Sir William Gull, one of Queen Victoria’s personal physicians [21], and he provided some detailed case descriptions and treatments.
Anorexia nervosa has an average prevalence for the diagnosis of 0.9 % in women and 0.3 % in men in developed countries [19]. It is seen mainly in young adolescent women and is more prevalent in the upper social classes [19]. It is unclear whether or not the incidence of anorexia nervosa is on the rise because it is difficult to compare the incident rates over time. Studies demonstrate that since at least 1970 the incidence of anorexia nervosa in adult women has been fairly constant, whereas there are other studies which indicate that the incidence may have been increasing for girls aged between 14 and 20 [22].
Many biological and sociological causes, not single ones but complexities of these conditions, are considered to be responsible for the onset of anorexia nervosa. In terms of biological causes, obstetric complications [23], genetic predisposition [24], serotonergic dysregulation [25], feeding-regulating neuropeptides [26], infection [27], autoimmune system [28] and nutrition deficiencies [29] have been proposed to be the causes of anorexia nervosa. In addition to these biological causes, sociological causes can also be responsible for developing anorexia nervosa. Specific cultural factors, such as family interactions, individual psychology, and media exposure, are also among the causes of one’s likelihood of developing anorexia. People in particular professions such as models are much more likely to develop anorexia [30]. A study has suggested that patients with anorexia nervosa can be characterized by alexithymia, and that this was the case in both adult and adolescent anorexia nervosa patients [31, 32].
Early intervention and treatment for anorexia nervosa seems to be more effective, though there is no conclusive treatment [33]. Usually, treatments aim to restore patients to a healthy weight, to treat the psychological problems related to anorexia nervosa, and to reduce or eliminate the behaviors or thoughts that originally led to the disordered eating [17]. It has been reported that the drug olanzapine is effective in treating certain aspects of anorexia nervosa [34]. Psychotherapies such as cognitive behavioral therapy or acceptance and commitment therapy are also used for treatment [17]. Regardless of these treatments, relapse, binging or starving after initial weight gain occurs in 40–70 % of the patients [17, 35]. It can be said that treating anorexia nervosa is never easy.
Neuropeptides in the hypothalamic nuclei to understand anorexia
Each nucleus responsible for feeding behavior and examples of the gene expression pattern of the feeding-regulating neuropeptides in the hypothalamus are described in Fig. 2.
Arcuate nucleus (ARC)
The ARC is considered to be one of the most important hypothalamic nuclei related to feeding behavior. Two main neuronal populations involved in feeding behavior exist in the ARC: the neuronal cells that produce neuropeptide Y (NPY) and agouti-related peptide (AgRP), which are orexigenic peptides, and α-melanocyte stimulating hormone (α-MSH), which is an anorexigenic peptide [36–38].
NPY-producing neurons and AgRP-producing neurons are described as NPY/AgRP neurons because they are approximately the same cell populations. NPY receptor subtype 5 is considered to be the key site of action in feeding promotion [39, 40]. The neurons that express NPY in rodents also express receptors for leptin and insulin and so are linked to plasma-derived feeding signals [41, 42]. AgRP is an antagonist for the anorexigenic peptides as it blocks the melanocortin 3 (MC3R) and 4 receptors (MC4R) for γ- and α-MSH, respectively [43, 44].
Administration of diphtheria toxin in mice expressing the diphtheria toxin receptor in NPY/AgRP neurons induces anorexia and body weight loss [45]. Feeding behavior is suppressed when the function of NPY and vesicular GABA transporter (VGAT) are simultaneously blocked [46]. This indicates that there are redundant mechanisms for feeding control. Projections from the NPY/AgRP neurons to the paraventricular nucleus (PVN) are important for the execution of feeding behavior. NPY/AgRP neurons suppress single-minded homolog 1 (sim1) and MC4R-positive cells through MC4R, GABA-A receptor and Y1 receptor, resulting in feeding behavior [47, 48].
α-MSH is processed from proopiomelanocortin (POMC), and POMC-producing neurons are known to exist in the ARC [49]. POMC neurons also produce cocaine-amphetamine-regulated transcript (CART) and are sometimes described as POMC/CART neurons [50]. In addition to these peptides, Galanin-like peptide (GALP), which is an anorexigenic peptide, is also expressed in the ARC [51]. Leptin receptors are strongly expressed in the ARC [52], and the number of phosphorylated Stat3-positive cells, a marker for activated leptin receptor signaling, is markedly increased after leptin administration [53]. Most of the POMC/CART neurons are not GABAergic, unlike NPY/AgRP neurons. Abundant expression of orexin type 2 receptors, leptin receptors, serotonin receptors and NPY receptors are observed in the POMC/CART neurons [54]. POMC/CART neurons receive excitatory projection from the VMH and feeding behavior is suppressed by this projection [55]. Estrogen receptors are abundantly expressed in the ARC and the gene expression of the POMC/CART is increased by estrogen [56].
Lateral hypothalamic area (LHA)
There are melanin-concentrating hormone (MCH)-producing neurons, orexin-producing neurons and polyglutamylated arginine-phenylalanineamide peptide (QRFP)-producing neurons in the LHA. Although, orexin has been reported as a peptide which promotes feeding, subsequent studies have reported that it is also a substantial neuropeptide in sleep–awake control [57]. Because increased food intake by orexin administration is confined during the light phase in rodents [58], it can be said that food consumption increased by orexin is an effect associated with arousal. In addition to orexin, MCH also promotes eating behavior [59]. Since the phenotype of orexin-deficient mice is obesity, and that of MCH-deficient mice is lean, the actions of orexin and MCH in terms of body weight regulation are opposite [60, 61]. The detailed mechanism of obesity in orexin-deficient mice remains unknown. One possible explanation is that, although orexin deficiency cause decreased food intake, energy expenditure may decrease much more than energy consumption. Another possible explanation is that orexin neuron deficiency causes deletion of other factors which are co-localized in orexin neurons and these factors might have important roles in the regulation of energy homeostasis. Fujiki et al. reported that the obesity in orexin-deficient mice is gender-specific and prominent in female mice [62]. They suggested that sexual dimorphism of leptin signaling likely exists, and alteration of this signaling may contribute to the gender difference in orexin-deficient obesity.
QRFP has been reported to be an orexigenic peptide in humans and rodents [63, 64]. In rats, the orexigenic effects of centrally administered QRFP are mediated by factors associated with an increased motivation to eat. The gene expression of QRFP is increased by the intake of a high fat diet but not by a low fat diet [65]. Effects of QRFP effects on food intake are considered to be mediated by the adiposity signal, leptin, and hypothalamic neuropeptides [66].
Paraventricular nucleus (PVN)
The PVN contains magnocellular neurosecretory cells (MNCs) whose axons extend into the posterior pituitary, parvocellular neurosecretory cells (PNCs) which project to the median eminence, and several populations of peptide-containing cells which project to many different brain regions, including parvocellular preautonomic neurons which project to the brainstem and spinal cord. Afferent outputs and inputs to the PVN from many important integrative centers of the hypothalamus and medulla have been identified. The PVN is important as a projection target from the NPY/AgRP neurons and POMC/CART neurons in the ARC [67, 68]. MC4R, the receptors for α-MSH, are expressed abundantly in the PVN [69, 70], and reducing MC4R in the PVN results in the development of obesity [71]. The POMC/CART neurons exhibit excitatory effects on MC4R-positive cells and the NPY/AgRP neurons exhibit inhibitory effects on MC4R via α-MSH, in addition, most of these MC4R-positive neurons are oxytocin (OXT)-producing neurons [47, 48].
Various neurohypophysial hormones related to feeding behavior are synthesized in the PVN. MNCs in the PVN produce and secrete two different types of neuropeptides: OXT and arginine vasopressin (AVP). A recent study has revealed that OXT neurons in the PVN may play a key role in suppressing appetite and that other hypothalamic neurons may trigger eating via inhibition of these OXT neurons [47]. This population of oxytocin neurons are absent in Prader–Willi syndrome, a genetic disorder which leads to uncontrollable feeding and obesity, and OXT is considered to play a key role in its pathophysiology [47].
In addition to one of the most important roles of AVP being regulating water retention, it also acts synergistically to stimulate adrenocorticotropic hormone (ACTH) secretion as well as corticotropin-releasing hormone (CRH) [72]. The main function of CRH is the stimulation of the pituitary synthesis of ACTH, resulting in the activation of the hypothalamo–pituitary–adrenal (HPA) axis and it is recognized as an anorexigenic neuropeptide [73].
Thyrotropin-releasing hormone (TRH) is a hormone produced in the PVN. It stimulates the release of thyroid-stimulating hormone (TSH) and prolactin (PRL) from the anterior pituitary. Excess levels of TRH inhibit dopamine, resulting in a disinhibition of prolactin and a subsequent decrease in gonadotropin-releasing hormone (GnRH) release [74]. Food, but not water intake, is greatly reduced following an i.c.v. injection of TRH in rats [75]. Other studies have also revealed that TRH is an anorexigenic neuropeptide [76, 77].
Recently, nesfatin-1, a newly identified anorexigenic neuropeptide, has been found to also exist in the PVN [78]. Nesfatin-1 participates in the regulation of hunger and fat storage. It is also distributed in the ARC or the LHA, important nuclei for feeding regulation [78]. Nesfatin-1 influences the excitability of a large proportion of different subpopulations of neurons located in the PVN, and it is reported that MNCs’ OXT neurons are activated by nesfatin-1during feeding, while i.c.v. administration of an OXT antagonist increases food intake, indicating a possible interaction between nesfatin-1 and OXT in the regulation of feeding behavior [79, 80]. Because nesfatin-1 neurons in the ARC are activated by simultaneous injection of ghrelin and desacyl ghrelin, they may be involved in the desacyl ghrelin-induced inhibition of the orexigenic effect of peripherally administered ghrelin in freely fed rats [81]. Nesfatin-1 is co-expressed with MCH in tuberal hypothalamic neurons [82], indicating a complex role not only in the regulation of food intake but also in other essential integrative brain functions involving MCH signaling, including autonomic regulation, stress, mood, cognition and sleep [83].
Ventromedial hypothalamus (VMH)
The VMH is known to be most commonly associated with satiety. Rats with VMH lesions were found to eat substantially more food and gained twice as much weight as those with PVN lesions [84]. It has been reported that there is a higher concentration of cannabinoid receptor mRNA within the VMH in comparison to other nuclei within the hypothalamus [85]. Cannabinoid ingestion has been linked to reward processes, and also with the release of dopamine in the brain [86]. Because leptin receptors and orexin receptors are abundantly distributed in the inner part of the VMH, it is considered one of the most important hypothalamic nuclei in feeding behavior [87, 88]. There are many projections between the VMH and other hypothalamic nuclei. Especially, excitatory projections from the pituitary adenylate cyclase-activating polypeptide (PACAP)-positive neurons in the VMH to the POMC/CART neurons in the ARC is thought to be one of the most important projections in suppressing feeding behavior [48].
Experimental anorexia animal models
Dehydration-induced anorexia
Because pathophysiological models of anorexia may involve multiple factors as previously described, developing a simple method to induce anorexia in animal models is necessary in order to improve our understanding of the neuronal and molecular mechanisms responsible for anorexia [16]. To resolve this problem, several groups have proposed the use of dehydration-induced anorexia in animal models [10, 89–91]. Dehydration-induced anorexia involves an important physiological adaptation that limits the intake of osmolytes from food and helps maintain the integrity of fluid compartments [92]. This model supports the existence of complex and varied neural network interactions that provide animals with the ability to adapt their feeding behaviors to deal with the many pressures imposed by the environment [93]. With this physiological aspect in mind, we examined several reports on dehydration-induced anorexia in animal models [11, 90, 91].
Watts and colleagues showed that rats develop profound anorexia from dehydration when hypertonic saline (2.5 % NaCl) instead of drinking water was given for 5 days [11, 94]. This model seems likely to be advantageous for examining the neuronal networks and feeding-regulating neuropeptides because slowly developed anorexia induced by dehydration is rapidly reversed once they regain access to drinking water.
According to their report, in dehydrated rats, the gene expression of the NPY in the ARC significantly increased in comparison with euhydrated rats [94]. In addition to this change, the gene expression of POMC and neurotensin/neuromedin N (NT/N) in the ARC and gene expression of CRH in the PVN were significantly decreased in comparison to euhydrated rats [94]. These changes were consistent and a result of the negative energy balance due to the animals developing anorexia with being dehydrated. Of interest, they also demonstrated that the gene expressions of CRH and NT/N in the LHA were significantly increased after dehydration. In addition, they reported that the gene expression of CRH in the LHA strongly correlated with the intensity of anorexia. These results suggest that the gene expressions of CRH and NT/N in the LHA increased by dehydration-induced anorexia act upon the PVN and suppress feeding in dehydrated rats [11, 90, 94].
Several studies have demonstrated that the gene expression of TRH in the PVN was significantly up-regulated in the dehydration-induced anorexia animal model [95–97]. These results indicate an inhibitory role of TRH in the PVN in feeding control as well as CRH or NT/N in the LHA.
We have previously demonstrated that the gene expression of nesfatin-1 in the PVN is also up-regulated in rats dehydrated for 2 days or drinking hypertonic saline (2 % NaCl) for 5 days instead of drinking tap water [10]. Dehydration causes hyperosmolality and hypovolemia. Chronic salt loading causes hyperosmolality without hypovolemia. The gene expression of nesfatin-1 was correlated with the degree of hyperosmolality and hypovolemia in this study. Moreover, i.c.v. injection of nesfatin-1 neutralizing antibody after 48 h water deprivation resulted in an almost complete cancelling of the anorexia induced by dehydration [10]. These results suggest that nesfatin-1 is one of the potential candidates involved in the development of anorexia induced by dehydration.
Rinaman and colleagues demonstrated that dehydration-induced anorexia was attenuated in OXT-deficient mice [98]. In addition, significantly fewer neurons within the hindbrain dorsal vagal complex were activated in OXT knockout dehydrated mice compared to wild-type dehydrated mice [98]. These results suggest that OXT neuronal projections from the hypothalamus to the hindbrain are necessary for the full expression of compensatory behavioral and physiological responses to dehydration. Taken together with the fact that OXT neurons are activated by nesfatin-1, these results are highly consistent with our study of nesfatin-1 in dehydration-induced anorexia.
Just and colleagues report that neuronal activity in the PVN and the LHA was increased in dehydrated anorexic female rats, using manganese-enhanced MRI, a noninvasive method for the investigation of the neuronal pathway [99]. It can be said that this study supports the previous reports, which indicate that activation of the PVN and LHA is induced in dehydrated animal models.
These studies raise the hypothesis that dehydration primarily causes up-regulation of the gene expression of the anorexigenic neuropeptides in the hypothalamus, and then anorexia-induced starvation, namely the negative energy balance, up-regulates the gene expression of the orexigenic neuropeptides (Fig. 3). The reason why dehydration primarily causes up-regulation of the anorexigenic neuropeptides, but not down-regulation of the orexigenic neuropeptides, remains unclear. Possible involvement of peripheral humoral factors such as circulating leptin, ghrelin, OXT and nesfatin-1 on dehydration-induced anorexia should be clarified by further study.
Cisplatin-induced anorexia
A pathophysiological anorexic animal model as well as a physiological anorexic model may also be important in examining the mechanisms of anorexia. Because it may involve multiple factors, investigating respective hypothalamic feeding-regulating neuropeptides could help us to understand molecular mechanisms or the central circuit responsible for anorexia.
Cisplatin-induced anorexia, one of the pathophysiological anorexic animal models, has been proposed by previous researchers. Cisplatin is widely used for various types of malignant tumors. It demonstrates anti-tumor effects by inhibiting the replication of DNA [100]. Although it is useful for treating diverse tumors, many disadvantageous side effects, such as loss of appetite, nausea and vomiting, afflict patients. It has been suggested that serotonin receptors are involved in the occurrence of nausea and vomiting from the use of cisplatin [101].
Yakabi and colleagues demonstrated that hypothalamic ghrelin secretion was markedly reduced 24 and 48 h after cisplatin treatment in cisplatin-treated rats compared to saline-treated rats, though their plasma ghrelin levels did not differ [102, 103]. In this study, it was found that the plasma acylated ghrelin level returned to the normal level within 24 h after a single administration of cisplatin, though the decreased food intake lasted for more than 48 h. They also demonstrated that i.c.v administration of ghrelin reversed the decreased in food intake in cisplatin-treated anorexic rats [102].
We previously described changes in the gene expression of the hypothalamic feeding-regulating neuropeptides in cisplatin-treated rats [13]. In this study, the gene expression of CRH in the PVN and the gene expression of NPY in the ARC were significantly decreased, while the gene expressions of POMC and CART in the ARC were markedly increased in cisplatin-treated rats compared to saline-treated rats. These results suggest that cisplatin primarily causes the up-regulation of the POMC and CART, anorexigenic neuropeptides, and down-regulation of NPY, an orexigenic neuropeptide, in the ARC, and that the ensuing decreased appetite, namely the negative energy balance, induced by cisplatin causes down-regulation of CRH, an anorexigenic neuropeptide, in the PVN.
There are abundant serotonergic neuronal projections from the raphe nuclei, where 5-HT is synthesized, to the hypothalamus and many 5-HT receptors have been identified in the ARC [104]. Taken together, it is speculated that peripherally administered cisplatin decreases ghrelin secretion in the hypothalamus and increases 5-HT receptors in the hypothalamus, which cause up-regulation of POMC and CART and down-regulation of NPY. It is thought that these alterations are one of the causes of anorexia induced by cisplatin.
These studies raise the hypothesis that peripheral administration of cisplatin primarily causes up-regulation in gene expression of the anorexigenic neuropeptides and down-regulation of the orexigenic neuropeptides in the hypothalamus (Fig. 4). These are convincing results because these neuropeptide changes induced by cisplatin administration cause anorexia. In other types of pathophysiological anorexia models such as lipopolysaccharide (LPS)-induced anorexia or cancer anorexia-cachexia models, primarily down-regulation of the MCH and orexin were also observed [50, 105], which is not observed in dehydration-induced anorexia. As well as dehydration-induced anorexia, the distinct underlying mechanisms between physiological and pathophysiological models in developing anorexia, including possible involvement of the peripheral humoral factors, should be revealed by further study.
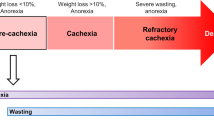
Cancer anorexia-cachexia
Anorexia-cachexia syndrome is reported in the advanced stages of cancer [106]. This syndrome is a cause of patients’ increased rate of morbidity and mortality [107]. Metabolic and behavioral abnormalities and psychological distress are observed in this syndrome, whereas it is difficult to describe a common factor which is responsible for cancer cachexia-anorexia syndrome because multiple factors may be involved in the etiology of this syndrome [108]. Although the understanding of cachexia has progressed over the last decade, the lack of consensus on a definition, diagnostic criteria and classification have impeded a meaningful advancement in both clinical trials and clinical practice. New definitions have proposed to integrate the concept of cachexia as a complex metabolic disorder, which is distinctly different to malnutrition [109].
Investigating hypothalamic feeding-regulating neuropeptides may be a good strategy in order to understand the underlying mechanism or central pathways which mediate feeding behavior, though multiple factors are involved in the cancer anorexia-cachexia. Previous studies have demonstrated that cytokines and hypothalamic neuropeptides are involved in cancer cachexia-anorexia syndrome [110–112], and that cachectic factors such as cytokines mimic the effects of leptin on the hypothalamus and induce anorexia in cachexia-anorexia syndrome [16].
Several studies focused on the orexigenic neuropeptides in the hypothalamus in the cancer anorexia-cachexia animal model. We demonstrated that the gene expressions of NPY, AgRP, MCH and ORX in the hypothalamus were significantly increased in rats implanted with 85As2 cells (human stomach cancer cell line) [15]. Nara-ashizawa et al. reported that the gene expression of NPY was significantly increased in mice bearing human tumor cells (SEKI melanoma cells); however, the gene expressions of MCH and ORX were comparable compared to control mice [105]. The up-regulation of the gene expression of NPY has also been reported in rats bearing glucagonoma (MSL-G-AN) [113], tumor-bearing (methylcholanthrene-induced sarcoma) rats [114] and MAC16 (chronic adenocarcinoma)-bearing mice [115], whereas Plata-Salaman et al. demonstrated that NPY mRNA expression was not different between pair-fed normal rats and prostate adenocarcinoma tumor cell-bearing rats [116]. Treatment with i.c.v. administration of NPY worsened anorexia in tumor-bearing rats, suggesting that cachexia did not result from a selective reduction in NPY release [117].
It is difficult to explain the cause of the up-regulation of the gene expression of NPY or other orexigenic neuropeptides in cachectic tumor-bearing animal models. One possible explanation is that, downstream of NPY mRNA, functions such as protein synthesis, transport, secretion and its receptors are distributed by humoral factors such as cytokines and tumor-derived factors [118].
Changes of anorexigenic neuropeptides in cancer anorexia-cachexia have also been reported. We demonstrated that the gene expressions of CRH, POMC and CART are significantly decreased in rats implanted with 85As2 cells (human stomach cancer cell line) [15]. In contrast, Nara-ashizawa et al. reported that CRH mRNA in the PVN was significantly up-regulated in cachectic tumor-bearing mice [105], and Jensen et al. reported that CART mRNA in the hypothalamus was highly expressed in rats bearing glucagonoma [113]. However, Nakhate et al. indicated that a cancerous condition might down-regulate CART in the hypothalamus in rats with N-methyl-N-nitrosourea-induced mammary tumors [119].
Focusing on hypothalamic neuropeptide receptors, as opposed to the neuropeptides themselves, it has been demonstrated that MC4R expression in the PVN, which is one of the most important receptors that mediate feeding regulation, was significantly increased, resulting in decreased food intake and increased energy expenditure [120], while possible involvement of decreased ghrelin receptor signaling may be one of the causes of cancer anorexia-cachexia [121].
Because previous studies are discordant as mentioned above, it is difficult to decide the role of hypothalamic neuropeptides in appetite loss in cancer anorexia-cachexia animal models. Different models of tumor-bearing animals and different assays such as northern blot analysis, RNA protection assay and in situ hybridization histochemistry may be the reasons for the discrepancies. In addition, the studies have not examined all of the hypothalamic feeding-regulating neuropeptides at each stage of cachexia, and these cancer anorexia-cachexia animal models were not recovered by the therapeutic treatment, thus the hypothalamic neuropeptides changes cannot be readily compared.
The parathyroid hormone-related protein (PTHrP)-secreting tumor-bearing animal model, which is an ideal anorexia-cachexia animal model, has been proposed to resolve these issues. PTHrP is frequently produced and secreted in various types of cancer and is known to be a principal factor related to humoral hypercalcemia of malignancy [122, 123].
Peripheral administration of the antibody which neutralizes PTHrP exerted anti-hypercalcemic effects and improved anorexia-cachexia syndrome in PTHrP-secreting tumor-bearing animal models [124–126]. We demonstrated that, using a rat model, the gene expressions of the orexigenic neuropeptides in the hypothalamus were significantly increased, whereas those of anorexigenic neuropeptides were markedly decreased compared to non-tumor-bearing rats [127]. Bolus intravenous administration of anti-PTHrP neutralizing antibody reversed these changes in this study [127].
It is possible that hypercalcemia in plasma may inhibit appetite and feeding through the central nervous system (CNS), because severe hypercalcemia was observed in this model. However, a recent study has revealed that tumor-derived PTHrP triggers adipose tissue browning and cancer cachexia [128]. In addition, PTHrP and its receptor were widely expressed in the brain of the rat [129]. Taken together, PTHrP may act as a potent neurotransmitter or neuromodulator in the CNS.
Conclusion and perspectives
The etiology of diverse types of anorexia or appetite loss cannot be simply explained by the two-center theory in the hypothalamus as previously described. Thus, it may be useful to study from the perspective of respective feeding-regulating neuropeptides in the hypothalamus. It is hypothesized that dehydration-induced anorexia seems likely to be the result of up-regulation of the anorexigenic neuropeptides. In contrast, cisplatin-induced anorexia seems likely to be the result of the down-regulation of the orexigenic neuropeptides in addition to the up-regulation of the anorexigenic neuropeptides.
However, regardless of the up-regulation of the orexigenic neuropeptides induced by dehydration or cisplatin or cancer, these changes do not stimulate feeding. In the present review, because we have mentioned only restrictive models for anorexia, the complexity of the topic cannot be illustrated simply. Further studies should investigate not only homeostatic aspects of feeding but also hedonic aspects, to further understand the underlying mechanisms. Although human anorexia nervosa cannot be explained solely by the changes of the feeding-regulating neuropeptides in the hypothalamus, it may bring a unique strategy to the comprehension of the behavior and new therapeutics for its treatment.
References
Piccinni A, Marazziti D, Vanelli F, Franceschini C, Baroni S, Costanzo D, Cremone IM, Veltri A, Dell'Osso L (2015) Food addiction spectrum: a theoretical model from normality to eating and overeating disorders. Curr Med Chem 22(13):1631–1638
Lozano R et al (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2095–2128
Debons AF et al (1968) Gold thioglucose damage to the satiety center: inhibition in diabetes. Am J Physiol 214(3):652–658
Anand BK, Brobeck JR (1951) Localization of a feeding center in the hypothalamus of the rat. Proc Soc Exp Biol Med 77(2):323–324
Anand BK, Brobeck JR (1951) Hypothalamic control of food intake in rats and cats. Yale J Biol Med 24(2):123–140
Morgane PJ (1961) Evidence of a hunger motivational system in the lateral hypothalamus of the rat. Nature 191:672–674
Hoess RH, Ziese M, Sternberg N (1982) P1 site-specific recombination: nucleotide sequence of the recombining sites. Proc Natl Acad Sci USA 79(11):3398–3402
Wu Q, Clark MS, Palmiter RD (2012) Deciphering a neuronal circuit that mediates appetite. Nature 483(7391):594–597
Merali Z et al (2013) Stress and eating: a dual role for bombesin-like peptides. Front Neurosci 7:193
Yoshimura M et al (2014) A role of nesfatin-1/NucB2 in dehydration-induced anorexia. Am J Physiol Regul Integr Comp Physiol 307(2):R225–R236
Watts AG, Sanchez-Watts G, Kelly AB (1999) Distinct patterns of neuropeptide gene expression in the lateral hypothalamic area and arcuate nucleus are associated with dehydration-induced anorexia. J Neurosci 19(14):6111–6121
Haque Z et al (2013) Inhibition of immobilization stress-induced anorexia, behavioral deficits, and plasma corticosterone secretion by injected leptin in rats. Stress 16(3):353–362
Yoshimura M et al (2013) The gene expression of the hypothalamic feeding-regulating peptides in cisplatin-induced anorexic rats. Peptides 46:13–19
Lugarini F et al (2002) A role for cyclooxygenase-2 in lipopolysaccharide-induced anorexia in rats. Am J Physiol Regul Integr Comp Physiol 283(4):R862–R868
Terawaki K et al (2014) New cancer cachexia rat model generated by implantation of a peritoneal dissemination-derived human stomach cancer cell line. Am J Physiol Endocrinol Metab 306(4):E373–E387
Ueta Y et al (2007) Hypothalamic neuropeptides and appetite response in anorexia-cachexia animal. Endocr J 54(6):831–838
Cooper MJ (2005) Cognitive theory in anorexia nervosa and bulimia nervosa: progress, development and future directions. Clin Psychol Rev 25(4):511–531
Attia E (2010) Anorexia nervosa: current status and future directions. Annu Rev Med 61:425–435
Treasure J, Claudino AM, Zucker N (2010) Eating disorders. Lancet 375(9714):583–593
Pearce JM (2004) Richard Morton: origins of anorexia nervosa. Eur Neurol 52(4):191–192
Gull WW (1997) Anorexia nervosa (apepsia hysterica, anorexia hysterica). 1868. Obes Res 5(5):498–502
Smink FR, van Hoeken D, Hoek HW (2012) Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 14(4):406–414
Favaro A, Tenconi E, Santonastaso P (2006) Perinatal factors and the risk of developing anorexia nervosa and bulimia nervosa. Arch Gen Psychiatry 63(1):82–88
Wade TD et al (2000) Anorexia nervosa and major depression: shared genetic and environmental risk factors. Am J Psychiatry 157(3):469–471
Kaye WH et al (2005) Serotonin alterations in anorexia and bulimia nervosa: new insights from imaging studies. Physiol Behav 85(1):73–81
Frederich R et al (2002) Leptin in anorexia nervosa and bulimia nervosa: importance of assay technique and method of interpretation. J Lab Clin Med 139(2):72–79
Swedo SE et al (1998) Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. Am J Psychiatry 155(2):264–271
Fetissov SO et al (2005) Autoantibodies against neuropeptides are associated with psychological traits in eating disorders. Proc Natl Acad Sci USA 102(41):14865–14870
Shay NF, Mangian HF (2000) Neurobiology of zinc-influenced eating behavior. J Nutr 130(5S Suppl):1493S–1499S
Garner DM, Garfinkel PE (1980) Socio-cultural factors in the development of anorexia nervosa. Psychol Med 10(4):647–656
Zonnevijlle-Bender MJ et al (2002) Do adolescent anorexia nervosa patients have deficits in emotional functioning? Eur Child Adolesc Psychiatry 11(1):38–42
Harrison A et al (2009) Emotion recognition and regulation in anorexia nervosa. Clin Psychol Psychother 16(4):348–356
Lock JD, Fitzpatrick KK (2009) Anorexia nervosa. BMJ Clin Evid
Brambilla F et al (2007) Olanzapine therapy in anorexia nervosa: psychobiological effects. Int Clin Psychopharmacol 22(4):197–204
Halmi KA (1996) The psychobiology of eating behavior in anorexia nervosa. Psychiatry Res 62(1):23–29
Chronwall BM, Chase TN, O’Donohue TL (1984) Coexistence of neuropeptide Y and somatostatin in rat and human cortical and rat hypothalamic neurons. Neurosci Lett 52(3):213–217
Broberger C et al (1998) The neuropeptide Y/agouti gene-related protein (AGRP) brain circuitry in normal, anorectic, and monosodium glutamate-treated mice. Proc Natl Acad Sci USA 95(25):15043–15048
Medina F et al (1998) The inter-relationship between gonadal steroids and POMC peptides, beta-endorphin and alpha-MSH, in the control of sexual behavior in the female rat. Peptides 19(8):1309–1316
Xin XG, Huang XF (1998) Down-regulated NPY receptor subtype-5 mRNA expression in genetically obese mouse brain. NeuroReport 9(4):737–741
Criscione L et al (1998) Food intake in free-feeding and energy-deprived lean rats is mediated by the neuropeptide Y5 receptor. J Clin Invest 102(12):2136–2145
Schwartz MW et al (1996) Identification of targets of leptin action in rat hypothalamus. J Clin Invest 98(5):1101–1106
Morgan DG et al (1998) Inhibition of glucose stimulated insulin secretion by neuropeptide Y is mediated via the Y1 receptor and inhibition of adenylyl cyclase in RIN 5AH rat insulinoma cells. Diabetologia 41(12):1482–1491
Nijenhuis WA, Oosterom J, Adan RA (2001) AgRP(83–132) acts as an inverse agonist on the human-melanocortin-4 receptor. Mol Endocrinol 15(1):164–171
Irani BG et al (2011) Implication of the melanocortin-3 receptor in the regulation of food intake. Eur J Pharmacol 660(1):80–87
Gropp E et al (2005) Agouti-related peptide-expressing neurons are mandatory for feeding. Nat Neurosci 8(10):1289–1291
Krashes MJ et al (2013) Rapid versus delayed stimulation of feeding by the endogenously released AgRP neuron mediators GABA, NPY, and AgRP. Cell Metab 18(4):588–595
Atasoy D et al (2012) Deconstruction of a neural circuit for hunger. Nature 488(7410):172–177
Krashes MJ et al (2014) An excitatory paraventricular nucleus to AgRP neuron circuit that drives hunger. Nature 507(7491):238–242
Kiss JZ et al (1985) Topographical distribution of pro-opiomelanocortin-derived peptides (ACTH/beta-END/alpha-MSH) in the rat median eminence. Brain Res 329(1–2):169–176
Sergeyev V, Broberger C, Hokfelt T (2001) Effect of LPS administration on the expression of POMC, NPY, galanin, CART and MCH mRNAs in the rat hypothalamus. Brain Res Mol Brain Res 90(2):93–100
Jureus A et al (2000) Galanin-like peptide (GALP) is a target for regulation by leptin in the hypothalamus of the rat. Endocrinology 141(7):2703–2706
Mercer JG et al (1996) Coexpression of leptin receptor and preproneuropeptide Y mRNA in arcuate nucleus of mouse hypothalamus. J Neuroendocrinol 8(10):733–735
Hakansson ML, Meister B (1998) Transcription factor STAT3 in leptin target neurons of the rat hypothalamus. Neuroendocrinology 68(6):420–427
Funato H et al (2009) Enhanced orexin receptor-2 signaling prevents diet-induced obesity and improves leptin sensitivity. Cell Metab 9(1):64–76
Sternson SM, Shepherd GM, Friedman JM (2005) Topographic mapping of VMH→arcuate nucleus microcircuits and their reorganization by fasting. Nat Neurosci 8(10):1356–1363
Gao Q et al (2007) Anorectic estrogen mimics leptin’s effect on the rewiring of melanocortin cells and Stat3 signaling in obese animals. Nat Med 13(1):89–94
Sakurai T et al. (1998) Orexins and orexin receptors: a family of hypothalamic neuropeptides and G protein-coupled receptors that regulate feeding behavior. Cell 92(5): p 1 page following 696
Kiwaki K et al (2004) Orexin A (hypocretin 1) injected into hypothalamic paraventricular nucleus and spontaneous physical activity in rats. Am J Physiol Endocrinol Metab 286(4):E551–E559
Williamson-Hughes PS, Grove KL, Smith MS (2005) Melanin concentrating hormone (MCH): a novel neural pathway for regulation of GnRH neurons. Brain Res 1041(2):117–124
Shimada M et al (1998) Mice lacking melanin-concentrating hormone are hypophagic and lean. Nature 396(6712):670–674
Hara J, Yanagisawa M, Sakurai T (2005) Difference in obesity phenotype between orexin-knockout mice and orexin neuron-deficient mice with same genetic background and environmental conditions. Neurosci Lett 380(3):239–242
Fujiki N et al (2006) Sex difference in body weight gain and leptin signaling in hypocretin/orexin deficient mouse models. Peptides 27(9):2326–2331
Kampe J et al (2006) Effect of central administration of QRFP(26) peptide on energy balance and characterization of a second QRFP receptor in rat. Brain Res 1119(1):133–149
Ramanjaneya M et al (2013) QRFP induces aldosterone production via PKC and T-type calcium channel-mediated pathways in human adrenocortical cells: evidence for a novel role of GPR103. Am J Physiol Endocrinol Metab 305(9):E1049–E1058
Primeaux SD (2011) QRFP in female rats: effects on high fat food intake and hypothalamic gene expression across the estrous cycle. Peptides 32(6):1270–1275
Primeaux SD, Barnes MJ, Braymer HD (2013) Hypothalamic QRFP: regulation of food intake and fat selection. Horm Metab Res 45(13):967–974
Bell ME et al (2000) Disruption of arcuate/paraventricular nucleus connections changes body energy balance and response to acute stress. J Neurosci 20(17):6707–6713
Solomon A, De Fanti BA, Martinez JA (2005) Peripheral ghrelin participates in glucostatic feeding mechanisms and in the anorexigenic signalling mediated by CART and CRF neurons. Nutr Neurosci 8(5–6):287–295
Siljee JE et al (2013) Melanocortin 4 receptor distribution in the human hypothalamus. Eur J Endocrinol 168(3):361–369
Vella KR et al (2011) NPY and MC4R signaling regulate thyroid hormone levels during fasting through both central and peripheral pathways. Cell Metab 14(6):780–790
Balthasar N et al (2005) Divergence of melanocortin pathways in the control of food intake and energy expenditure. Cell 123(3):493–505
Juszczak M et al (2014) The influence od melatonin receptors antagonists, luzindole and 4-phenyl-2-propionamidotetralin (4-P-PDOT), on melatonin-dependent vasopressin and adrenocorticotropic hormone (ACTH) release from the rat hypothalamo-hypophysial system. In vitro and in vivo studies. J Physiol Pharmacol 65(6):777–784
Morton GJ et al (2006) Central nervous system control of food intake and body weight. Nature 443(7109):289–295
Hagen TC, Guansing AR, Sill AJ (1976) Preliminary evidence for a human prolactin releasing factor. Neuroendocrinology 21(3):255–261
Lin MT, Chu PC, Leu SY (1983) Effects of TSH, TRH, LH and LHRH on thermoregulation and food and water intake in the rat. Neuroendocrinology 37(3):206–211
Steward CA et al (2003) Central administration of thyrotropin releasing hormone (TRH) and related peptides inhibits feeding behavior in the Siberian hamster. Neuroreport 14(5):687–691
Kow LM, Pfaff DW (1987) Neuropeptides TRH and cyclo(His-Pro) share neuromodulatory, but not stimulatory, action on hypothalamic neurons in vitro: implication for the regulation of feeding. Exp Brain Res 67(1):93–99
Oh IS et al (2006) Identification of nesfatin-1 as a satiety molecule in the hypothalamus. Nature 443(7112):709–712
Stengel A, Tache Y (2011) Minireview: nesfatin-1—an emerging new player in the brain-gut, endocrine, and metabolic axis. Endocrinology 152(11):4033–4038
Maejima Y et al (2009) Nesfatin-1-regulated oxytocinergic signaling in the paraventricular nucleus causes anorexia through a leptin-independent melanocortin pathway. Cell Metab 10(5):355–365
Inhoff T et al (2008) Desacyl ghrelin inhibits the orexigenic effect of peripherally injected ghrelin in rats. Peptides 29(12):2159–2168
Fort P et al (2008) The satiety molecule nesfatin-1 is co-expressed with melanin concentrating hormone in tuberal hypothalamic neurons of the rat. Neuroscience 155(1):174–181
Shimizu H et al (2009) A new anorexigenic protein, nesfatin-1. Peptides 30(5):995–998
King BM (2006) The rise, fall, and resurrection of the ventromedial hypothalamus in the regulation of feeding behavior and body weight. Physiol Behav 87(2):221–244
Kim KW et al (2008) Steroidogenic factor 1 regulates expression of the cannabinoid receptor 1 in the ventromedial hypothalamic nucleus. Mol Endocrinol 22(8):1950–1961
Bodnar RJ (2013) Endogenous opiates and behavior: 2012. Peptides 50:55–95
Dhillon H et al (2006) Leptin directly activates SF1 neurons in the VMH, and this action by leptin is required for normal body-weight homeostasis. Neuron 49(2):191–203
Lu XY et al (2000) Differential distribution and regulation of OX1 and OX2 orexin/hypocretin receptor messenger RNA in the brain upon fasting. Horm Behav 37(4):335–344
Watts AG (1999) Dehydration-associated anorexia: development and rapid reversal. Physiol Behav 65(4–5):871–878
Watts AG (2001) Neuropeptides and the integration of motor responses to dehydration. Annu Rev Neurosci 24:357–384
Schoorlemmer GH, Evered MD (2002) Reduced feeding during water deprivation depends on hydration of the gut. Am J Physiol Regul Integr Comp Physiol 283(5):R1061–R1069
Boyle CN et al (2012) Dehydration-anorexia derives from a reduction in meal size, but not meal number. Physiol Behav 105(2):305–314
Watts AG, Boyle CN (2010) The functional architecture of dehydration-anorexia. Physiol Behav 100(5):472–477
Watts AG, Kelly AB, Sanchez-Watts G (1995) Neuropeptides and thirst: the temporal response of corticotropin-releasing hormone and neurotensin/neuromedin N gene expression in rat limbic forebrain neurons to drinking hypertonic saline. Behav Neurosci 109(6):1146–1157
Garcia-Luna C et al (2010) Prepro-orexin and feeding-related peptide receptor expression in dehydration-induced anorexia. Regul Pept 159(1–3):54–60
Alvarez-Salas E et al (2012) Food-restricted and dehydrated-induced anorexic rats present differential TRH expression in anterior and caudal PVN. Role of type 2 deiodinase and pyroglutamyl aminopeptidase II. Endocrinology 153(8):4067–4076
Jaimes-Hoy L, Joseph-Bravo P, de Gortari P (2008) Differential response of TRHergic neurons of the hypothalamic paraventricular nucleus (PVN) in female animals submitted to food-restriction or dehydration-induced anorexia and cold exposure. Horm Behav 53(2):366–377
Rinaman L et al (2005) Dehydration anorexia is attenuated in oxytocin-deficient mice. Am J Physiol Regul Integr Comp Physiol 288(6):R1791–R1799
Just N, Gruetter R (2011) Detection of neuronal activity and metabolism in a model of dehydration-induced anorexia in rats at 14.1 T using manganese-enhanced MRI and 1H MRS. NMR Biomed 24(10):1326–1336
Kocsis F, Klein W, Altmann H (1973) A screening system to determine inhibition of specific enzymes of the semiconservative DNA-synthesis and DNA-repair replication (author’s transl). Z Naturforsch C 28(3):131–135
du Percie Sert N et al (2011) Cisplatin-induced emesis: systematic review and meta-analysis of the ferret model and the effects of 5-HT(3) receptor antagonists. Cancer Chemother Pharmacol 67(3):667–686
Yakabi K et al (2010) Reduced ghrelin secretion in the hypothalamus of rats due to cisplatin-induced anorexia. Endocrinology 151(8):3773–3782
Yakabi K et al (2010) Rikkunshito and 5-HT2C receptor antagonist improve cisplatin-induced anorexia via hypothalamic ghrelin interaction. Regul Pept 161(1–3):97–105
Voigt JP, Fink H (2015) Serotonin controlling feeding and satiety. Behav Brain Res 277:14–31
Nara-ashizawa N et al (2001) Hypothalamic appetite-regulating neuropeptide mRNA levels in cachectic nude mice bearing human tumor cells. Metabolism 50(10):1213–1219
Fujitsuka N, Uezono Y (2014) Rikkunshito, a ghrelin potentiator, ameliorates anorexia-cachexia syndrome. Front Pharmacol 5:271
Evans WJ et al (2008) Cachexia: a new definition. Clin Nutr 27(6):793–799
Mondello P et al (2015) Cancer cachexia syndrome: pathogenesis, diagnosis, and new therapeutic options. Nutr Cancer 67(1):12–26
Fearon K, Arends J, Baracos V (2013) Understanding the mechanisms and treatment options in cancer cachexia. Nat Rev Clin Oncol 10(2):90–99
Ramos EJ et al (2004) Cancer anorexia-cachexia syndrome: cytokines and neuropeptides. Curr Opin Clin Nutr Metab Care 7(4):427–434
Laviano A et al (2005) Therapy insight: cancer anorexia-cachexia syndrome—when all you can eat is yourself. Nat Clin Pract Oncol 2(3):158–165
Muscaritoli M et al (2006) Prevention and treatment of cancer cachexia: new insights into an old problem. Eur J Cancer 42(1):31–41
Jensen PB et al (1998) Transplantable rat glucagonomas cause acute onset of severe anorexia and adipsia despite highly elevated NPY mRNA levels in the hypothalamic arcuate nucleus. J Clin Invest 101(2):503–510
Chance WT et al (1998) NPY messenger RNA is increased in medial hypothalamus of anorectic tumor-bearing rats. Regul Pept 75–76:347–353
Bing C et al (2001) Cachexia in MAC16 adenocarcinoma: suppression of hunger despite normal regulation of leptin, insulin and hypothalamic neuropeptide Y. J Neurochem 79(5):1004–1012
Plata-Salaman CR, Ilyin SE, Gayle D (1998) Brain cytokine mRNAs in anorectic rats bearing prostate adenocarcinoma tumor cells. Am J Physiol 275(2 Pt 2):R566–R573
Chance WT et al (1996) Assessment of feeding response of tumor-bearing rats to hypothalamic injection and infusion of neuropeptide Y. Peptides 17(5):797–801
McCarthy HD et al (1993) Alterations in hypothalamic NPY and CRF in anorexic tumor-bearing rats. Am J Physiol 264(4 Pt 1):E638–E643
Nakhate KT et al (2010) Hypothalamic cocaine- and amphetamine-regulated transcript peptide is reduced and fails to modulate feeding behavior in rats with chemically-induced mammary carcinogenesis. Pharmacol Biochem Behav 97(2):340–349
Suzuki M et al (2012) Changes in the melanocortin receptors in the hypothalamus of a rat model of cancer cachexia. Synapse 66(8):747–751
Fujitsuka N et al (2011) Potentiation of ghrelin signaling attenuates cancer anorexia-cachexia and prolongs survival. Transl Psychiatry 1:e23
Grill V, Rankin W, Martin TJ (1998) Parathyroid hormone-related protein (PTHrP) and hypercalcaemia. Eur J Cancer 34(2):222–229
Suva LJ et al (1987) A parathyroid hormone-related protein implicated in malignant hypercalcemia: cloning and expression. Science 237(4817):893–896
Kukreja SC et al (1988) Antibodies to parathyroid hormone-related protein lower serum calcium in athymic mouse models of malignancy-associated hypercalcemia due to human tumors. J Clin Invest 82(5):1798–1802
Iguchi H et al (2001) Involvement of parathyroid hormone-related protein in experimental cachexia induced by a human lung cancer-derived cell line established from a bone metastasis specimen. Int J Cancer 94(1):24–27
Onuma E et al (2005) Parathyroid hormone-related protein (PTHrP) as a causative factor of cancer-associated wasting: possible involvement of PTHrP in the repression of locomotor activity in rats bearing human tumor xenografts. Int J Cancer 116(3):471–478
Hashimoto H et al (2007) Parathyroid hormone-related protein induces cachectic syndromes without directly modulating the expression of hypothalamic feeding-regulating peptides. Clin Cancer Res 13(1):292–298
Kir S et al (2014) Tumour-derived PTH-related protein triggers adipose tissue browning and cancer cachexia. Nature 513(7516):100–104
Weaver DR et al (1995) Localization of parathyroid hormone-related peptide (PTHrP) and PTH/PTHrP receptor mRNAs in rat brain. Brain Res Mol Brain Res 28(2):296–310
Acknowledgments
We thank A. Dickie (University of Glasgow) for language editing of the manuscript. This article was supported by a Grant-in-Aid for Scientific Research (B) (no. 25293055) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; a Research Project for Improving Quality in Healthcare and Collecting Scientific Evidence on Integrative Medicine from the Ministry of Health Labour and Welfare, Japan; and by The Naito Foundation, Japan.
Conflict of interest
All authors declare that there are no conflicts of interest, financial or otherwise.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Yoshimura, M., Uezono, Y. & Ueta, Y. Anorexia in human and experimental animal models: physiological aspects related to neuropeptides. J Physiol Sci 65, 385–395 (2015). https://doi.org/10.1007/s12576-015-0386-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-015-0386-3