Abstract
Central arterial pulse pressure (PP), a strong predictor of cardiovascular disease, mainly consists of an incident wave generated by left ventricular ejection and a late-arriving reflected wave emanating from the lower body. We have tested the hypothesis that a reduction in leg vascular tone by heat treatment of the lower leg attenuates the central arterial PP. Pressure and wave properties of the peripheral and central arteries were measured in eight young men before and after heat treatment of the lower leg (temperature approx. 43 °C) for 30 and 60 min, respectively. Following the lower leg heat trial, leg (femoral–ankle) pulse wave velocity (PWV) was significantly decreased, but aortic (carotid–femoral) PWV and parameters of wave reflection and carotid arterial PP did not change significantly. No significant changes were observed in these parameters in the control trial. These results suggest that the reduction in leg vascular tone induced by heat treatment of the lower leg may not affect wave reflection and central arterial PP in young men.
Similar content being viewed by others
Introduction
High pulse pressure (PP) of the central arteries, such as the aorta and carotid artery, is more strongly associated with risk for cardiovascular disease than high PP of the peripheral arteries [1–4]. Thus, effective management of central arterial PP might be of pathophysiological importance. The pulsatile component of central arterial pressure consists of an incident wave elicited by left ventricular ejection and a late-arriving reflected wave arising from the peripheral vasculature of the lower body [5]. As the reflected wave seems to accrue at high resistance arterioles as well as other sites of impedance mismatch in the arterial tree (e.g., aortic bifurcation and branches of renal arteries) [5], it is very possible that peripheral vascular properties influence central arterial PP. Systemic vasodilation caused by the administration of the endothelium-independent vasodilator nitroglycerin induces a significant reduction in the central augmentation index (AI), an index of wave reflection, without alterations in heart rate (HR) and blood pressure (BP) [6]. Additionally, systemic α1-adrenergic receptor blockade evokes a significant attenuation of aortic PP elevation during dynamic leg exercise [7]. Therefore, a transient change in peripheral vascular tone may also alter central arterial PP. Although the major reflected wave emanates from peripheral vasculature in the lower body, the influence of regional change in leg vascular tone on central arterial PP remains incompletely understood.
We have studied the influence of lower leg vascular tone on central (carotid) arterial hemodynamics. To elicit vasodilation of the leg vasculature, we immersed the lower leg of eight healthy male subjects in a hot water bath as a heat treatment [8–12]; these subjects were considered to have relatively higher vasodilatory function [13, 14]. We hypothesized that in these young men, decreased leg vascular tone due to heating of the lower leg would decrease carotid arterial PP by the attenuation of wave reflection.
Methods
Subjects
We studied eight, apparently healthy young men [mean ± standard error of the mean (SEM): age 21 ± 1 years, height 171 ± 2 cm, weight 65 ± 2 kg]. All subjects had no apparent cardiovascular disease based on assessment of their respective medical history and did not take any medications. None of the participants had a history of smoking or regular physical exercise, and had adopted a normal living style. This study was approved by the Ethical Committees of the Institute of Health and Sport Sciences of the University of Tsukuba. The study conformed to the principles outlined in the Helsinki Declaration, and all subjects provided written informed consent before inclusion in the study.
Experimental protocol
The experiment consisted of a 30-min intervention (lower leg heating and control) and pre- and post-intervention hemodynamic measurements, with the post-intervention measurements performed 30 and 60 min after the intervention. The subjects abstained from alcohol, caffeine intake and vigorous exercise for at least 24 h before the experiments. In all experiments, the subjects were evaluated concurrently. First, they were asked to lay still for at least 30 min in a temperature-controlled room (approx. 23 °C) before baseline measurements were obtained. Then, during the interventions, the subjects were asked to rest still in a comfortable chair and put their lower legs and feet into a plastic bucket (diameter 42 cm, depth 40 cm) containing hot water (approx. 43 °C, approx. 40 cm of hot water; lower leg heating trial) or not containing hot water (control). To maintain the temperature of the water in the plastic basin at 43° for 30 min, hot water (at 43°) was continually added to the bucket during the 30-min trial using a hot-water supply system (BC60V3; Rinnai Corporation, Nagoya, Japan). These trials were performed on separate days with a crossover design.
Measurements
Hemodynamic variables
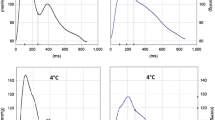
Heart rate, brachial BP and pulse wave velocity (PWV) were measured with a vascular testing device equipped with an electrocardiogram, phonocardiogram, oscillometric extremities cuffs and an (optional) applanation tonometry sensor unit (Form PWV/ABI: Model BP-203RPEII and TU-100; Colin Medical Technology, Komaki, Japan), as previously described [15, 16]. Carotid and femoral arterial pressure waveforms were simultaneously recorded by two applanation tonometry sensors incorporating an array of 15 micropiezoresistive transducers. Briefly, PWV (=arterial path length/pulse transit time) was obtained between the carotid and femoral regions (e.g. aorta) and between the femoral and ankle regions (e.g. leg). These arterial path lengths were assessed in duplicate with a random zero length measurement over the surface of the body with a nonelastic tape measure [17]. Pulse transit times were automatically computed from simultaneously recorded arterial pressure waveforms at the left carotid, left femoral (via applanation tonometory sensors) and left posterior-tibial (via air plethysmography) arteries by the 5- to 30-Hz band pass filter-based algorithm of the testing device (Fig. 1). The carotid AI was also calculated automatically as the pressure wave above its systolic shoulder, which was detected by fourth-order derivatives [15], divided by the PP [18]. Carotid arterial pressure was calibrated by equating the mean carotid and diastolic BP to the mean brachial and diastolic BP [19].
Sample of simultaneous recordings of electrocardiogram (ECG), phonocardiogram (PCG) and arterial pressure waveforms at carotid (CAP), brachial (BAP), femoral (FAP), and posterior–tibial (PAP) arteries by an automated polygraph apparatus. Each box above the carotid arterial waveform indicates the location of tonometry sensor which detected the strongest pressure (black bar) among 15 sensors
Carotid blood pressure waveform analysis
LabVIEW-based pulse waveform analysis software (TRial, Omron Health Care Co., Kyoto, Japan) was used according to the algorithm published by Westerhof et al. [20] and Qasem and Avolio [21] to decompose the carotid arterial pressure waveforms into the forward- and backward-traveling (incident wave and reflected wave, respectively) waves and their time delay [e.g. the return time of the reflected wave (TR)].
Statistical analyses
The effects of acute lower leg heating on hemodynamic variables were evaluated by repeated-measure analysis of variance (ANOVA) in a general linear model (GLM). In the case of a significant F value, Fischer’s LSD post hoc test was used to identify significant differences among mean values. All data were reported as mean ± SEM. Statistical significance was defined a priori at P < 0.05.
Results
Brachial arterial BP, HR and body temperature in the lower leg subjected to heating and in the control lower leg were not significantly different (Table 1). The aortic PWV in the heated lower leg also did not significantly from the control level (Fig. 2). Leg PWV was significantly decreased at 30 min after the lower leg heating trial (773 ± 30 vs. 741 ± 26 cm/s, respectively; P < 0.05), and this decrease was not observed after the control trials (Fig. 2). Carotid BP, incident wave amplitude and parameters of wave reflection, such as AI, TR, and reflected wave amplitude, did not change significantly in either the lower leg heating trial or control trial (Table 2). Carotid and brachial arterial PP did not change significantly throughout both trials (Fig. 3).
Discussion
Owing to the growing body of evidence demonstrating superior prognostic utility of central arterial PP compared with that of peripheral arterial PP [22–24], in the near future lowering the central arterial PP may become important in hypertension management and cardiovascular disease prevention. Therefore, we attempted to identify a determinant of the central arterial PP. A major finding of this study was that after the heat intervention the PWV in the lower leg did significantly decrease, and the reflected wave and central arterial PP did not change. This result suggests that the reduction in leg vascular tone induced by heating of the lower leg does not affect the wave reflection and, consequently, does not affect the central arterial PP in young men.
The central arterial PP differs from the peripheral arterial PP due to the variable superposition of incident and reflected pressure waves along the arterial tree [5]. As the reflected pulse wave is likely to occur in the arterioles of the lower body, which show high resistance, as well as at the aortic bifurcation and branches of the renal arteries [5], we assumed that heating of the lower leg would reduce leg vasoconstrictor tone, resulting in delayed return and dampening the magnitude of the reflected pulse waves and subsequent attenuation of the central arterial PP.
It is well-known that warmth stimulation elicits vasodilatory substances, such as nitric oxide [10, 11], vasoactive intestinal peptide [8], prostanoids [9] and H1 histamine receptor [12]. Thus, in order to reduce vasoconstrictor tone in the leg vasculature, we applied heat stimulation to both of the lower legs of young healthy men who were likely to have relatively higher vasodilatory function. As expected, we found that heating of the lower leg decreased leg PWV, presumably due to a reduced local vasoconstrictor tone. However, aortic PWV, RWA and central (e.g. carotid artery) PP did not change significantly with heating of the lower leg. Although we were unable to clearly identify an etiology for this result, we do propose a number of theories. First, since the major reflection site is located in the abdominal region (i.e., renal and aortic bifurcation) in young adults [25], a reduction in the leg vasoconstrictor tone might not affect central arterial hemodynamics. In this context, an investigation of elderly adults may clarify whether this proposal is valid because the major wave reflection site shifts distally with advancing age [25]. Alternatively, the region subjected to heating (e.g. lower legs) might have been too small to influence central arterial hemodynamics. Further studies investigating the effects of heating an expanded full leg region, the use of different temperatures and/or the chronic application of lower leg heating on the central arterial PP are warranted.
Several methodological limitations of this study should be mentioned. First, we applied this method on carotid arterial pressure waveforms to extract carotid forward and backward pressure components, as previously reported [26]. The Westerhof’s triangulation method had been proposed for decomposing aortic forward and backward pressure waves. Although the shape of carotid arterial pressure waveform differs from that of aorta, these are both classified as central arterial pressure and provide qualitatively similar clinical information [27]. Of note, to validate this approach, we compared the ratio of backward pressure wave amplitude to forward pressure wave amplitude obtained from the carotid arterial waveform and found that this ratio was strongly correlated with the corresponding value acquired from aortic waveforms that was estimated from simultaneously recorded radial arterial pressure waveforms (r = 0.758, P < 0.01). Second, we performed measurements at 30 min post-intervention to elicit the reduction in local (leg) vasoconstrictor tone without systemic hemodynamic change (i.e. peripheral BP and HR), as seen in a previous study investigating the acute effect of aerobic exercise [28]. This protocol was likely the preferable one to test our hypothesis. To gain insight into the physiological mechanisms of central arterial hemodynamics, measurements of leg vascular tone at an earlier post-intervention phase (<30 min) are warranted.
In summary, using lower leg heating, we determined the influence of the transient reduction in leg vascular tone on the wave reflection and central arterial PP in healthy young men. Despite the decrease in leg PWV, measures of wave reflection and carotid arterial PP did not change significantly following the lower leg heating intervention. These results suggest that the lower leg heating-induced reduction in leg vascular tone does not affect the wave reflection and central arterial PP in young men.
References
Roman MJ, Devereux RB, Kizer JR, Lee ET, Galloway JM, Ali T, Umans JG, Howard BV (2007) Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the strong heart study. Hypertension 50:197–203
Roman MJ, Devereux RB, Kizer JR, Okin PM, Lee ET, Wang W, Umans JG, Calhoun D, Howard BV (2009) High central pulse pressure is independently associated with adverse cardiovascular outcome the strong heart study. J Am Coll Cardiol 54:1730–1734
Roman MJ, Okin PM, Kizer JR, Lee ET, Howard BV, Devereux RB (2010) Relations of central and brachial blood pressure to left ventricular hypertrophy and geometry: the strong heart study. J Hypertens 28:384–388
Safar ME, Blacher J, Pannier B, Guerin AP, Marchais SJ, Guyonvarc’h PM, London GM (2002) Central pulse pressure and mortality in end-stage renal disease. Hypertension 39:735–738
Nichols W, O’Rourke MF (2005) McDonald’s blood flow in arteries theoretical, experimental and clinical principles, 5th edn. Hodder Arnold, London
Wilkinson IB, MacCallum H, Cockcroft JR, Webb DJ (2002) Inhibition of basal nitric oxide synthesis increases aortic augmentation index and pulse wave velocity in vivo. Br J Clin Pharmacol 53:189–192
Sugawara J, Brothers RM, Raven PB, Okazaki K, Ogoh S (2013) Effect of systemic α1-adrenergic receptor blockade on central blood pressure response during exercise. J Physiol Sci 63:389–393
Bennett LA, Johnson JM, Stephens DP, Saad AR, Kellogg DL Jr (2003) Evidence for a role for vasoactive intestinal peptide in active vasodilatation in the cutaneous vasculature of humans. J Physiol 552:223–232
McCord GR, Cracowski JL, Minson CT (2006) Prostanoids contribute to cutaneous active vasodilation in humans. Am J Physiol Regul Integr Comp Physiol 291:R596–R602
Minson CT, Berry LT, Joyner MJ (2001) Nitric oxide and neurally mediated regulation of skin blood flow during local heating. J Appl Physiol 91:1619–1626
Taylor WF, Bishop VS (1993) A role for nitric oxide in active thermoregulatory vasodilation. Am J Physiol 264:H1355–H1359
Wong BJ, Williams SJ, Minson CT (2006) Minimal role for H1 and H2 histamine receptors in cutaneous thermal hyperemia to local heating in humans. J Appl Physiol 100:535–540
DeSouza CA, Shapiro LF, Clevenger CM, Dinenno FA, Monahan KD, Tanaka H, Seals DR (2000) Regular aerobic exercise prevents and restores age-related declines in endothelium-dependent vasodilation in healthy men. Circulation 102:1351–1357
Taddei S, Virdis A, Ghiadoni L, Salvetti G, Bernini G, Magagna A, Salvetti A (2001) Age-related reduction of NO availability and oxidative stress in humans. Hypertension 38:274–279
Sugawara J, Hayashi K, Yokoi T, Cortez-Cooper MY, DeVan AE, Anton MA, Tanaka H (2005) Brachial-ankle pulse wave velocity: an index of central arterial stiffness? J Hum Hypertens 19:401–406
Hayashi K, Sugawara J, Komine H, Maeda S, Yokoi T (2005) Effects of aerobic exercise training on the stiffness of central and peripheral arteries in middle-aged sedentary men. Jpn J Physiol 55:235–239
Tanaka H, DeSouza CA, Seals DR (1998) Absence of age-related increase in central arterial stiffness in physically active women. Arterioscler Thromb Vasc Biol 18:127–132
Kelly R, Daley J, Avolio A, O’Rourke M (1989) Arterial dilation and reduced wave reflection. Benefit of dilevalol in hypertension. Hypertension 14:14–21
Armentano R, Megnien JL, Simon A, Bellenfant F, Barra J, Levenson J (1995) Effects of hypertension on viscoelasticity of carotid and femoral arteries in humans. Hypertension 26:48–54
Westerhof BE, Guelen I, Westerhof N, Karemaker JM, Avolio A (2006) Quantification of wave reflection in the human aorta from pressure alone: a proof of principle. Hypertension 48:595–601
Qasem A, Avolio A (2008) Determination of aortic pulse wave velocity from waveform decomposition of the central aortic pressure pulse. Hypertension 51:188–195
Sharman JE, Laurent S (2013) Central blood pressure in the management of hypertension: soon reaching the goal? J Hum Hypertens 27:405–411
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F (2013) 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 31:1281–1357
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E (2014) 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311:507–520
Sugawara J, Hayashi K, Tanaka H (2010) Distal shift of arterial pressure wave reflection sites with aging. Hypertension 56:920–925
Lefferts WK, Augustine JA, Heffernan KS (2014) Effect of acute resistance exercise on carotid artery stiffness and cerebral blood flow pulsatility. Front Physiol 5:101
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C (2010) Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J 31:1865–1871
Kingwell BA, Berry KL, Cameron JD, Jennings GL, Dart AM (1997) Arterial compliance increases after moderate-intensity cycling. Am J Physiol 273:H2186–H2191
Acknowledgments
We thank Mr. Satoshi Oikawa for his technical assistance. The pulse waveform analysis software used for the present study was provided by Omron Health Care Corporation.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kosaki, K., Sugawara, J., Akazawa, N. et al. No influence of lower leg heating on central arterial pulse pressure in young men. J Physiol Sci 65, 311–316 (2015). https://doi.org/10.1007/s12576-015-0368-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-015-0368-5