Abstract
This review provides a critical overview of the literature published in the area of lactate in human sweat between 1934 and the present. The first section summarizes the relevant pieces of literature, the second evaluates the literature across a range of topics and the third presents potential applications for sweat lactate measurements. Key factors that may affect sweat lactate are discussed in detail in the second section of this review. Both acetylcholine and catecholamine hormonal signals can trigger sweating independently of one another; differences in sweat output and lactate concentrations are compared. The primary triggers for sweating, exercise and heat are also compared, with exercise-induced sweating being further examined with respect to the exercise intensity. This review examines the significant variations in sweat lactate between bodily sites as well the relationship to physiological parameters such as gender, age and physical fitness, along with the effect of climate adaptation on sweat lactate concentrations.
Similar content being viewed by others
Introduction and literature summary
Sweating is a vital part of human thermoregulation. Sweat is not just simple water but contains many dissolved components such as salts and other compounds, one of which is lactate. Many researchers have investigated sweat to see if its constituents could reflect the physiological conditions of the subject. We undertook this review to determine what indications exist for utilising sweat lactate to detect a number of physiological conditions. The subject of lactate in sweat, whilst only comprising a small part of sweat gland research, has been the focus of much research within the last century. This section aims to provide the reader with a summary of the key books and research that have shaped our understanding of lactate in human sweat over time. Many of the pieces are only dealt with briefly as they are discussed more extensively in subsequent sections.
There are several potential clinical applications for the analysis of lactate in sweat. One early hypothesis was that it could be used to monitor factors such as physical performance or restricted oxygen level since lactate is a product of anaerobic metabolism. It was proposed that determination of sweat lactate would offer a non-invasive alternative to blood lactate measurements; however, it appears that there is very poor correlation between blood and sweat lactate levels. Another proposed clinical application is as a measure of restricted blood flow such as pressure ischemia. Pressure ischemia can lead to such clinical consequences as decubitus ulcers (bedsores), and an early diagnosis of this condition before symptoms develop would be highly beneficial. There have also been some studies into using sweat lactate as a marker for cystic fibrosis (since that also leads to a reduction in available oxygen). Another potential application is in the detection of conditions that lead to excessive sweating such as Frey’s syndrome or panic disorder. However, only a few studies have been performed on these other applications.
Yas Kuno’s book The Physiology of Human Perspiration published in 1934 makes an ideal starting point for this review as it comprehensively presents the knowledge of sweat at the time [1]. Discussing lactic acid, the author hypothesizes that the sweat glands may act as secretory organs for blood lactic acid during intense work. It was also reported in the book for the first time that sweat rate falls in response to arterial occlusion; this is thought to be due to reduced glycolytic ATP production within the sweat glands.
Whitehouse was the first to observe that the first measurement often contained more lactate than subsequent measurements; a common feature found in subsequent studies of sweat lactate [2]. Also, the author found that sweat lactate concentration was significantly higher than, and unaffected by, a rising blood lactate concentration, and concluded that sweat lactate must be regarded as a normal metabolic product of the sweat gland. Regional variations in sweat composition [3] were reported, with a wide variation being reported across the five sites measured (torso, face, thigh, axilla and arm), from 16 mM on the face to over 30 mM on the thigh.
Sweat lactate output decreased in subjects as they became acclimatised to heat [4, 5], as well as demonstrating that lactate output increased in arm sweat when the arm had been occluded. The authors compared arm-bag sweat with whole body sweat composition [5] and showed that sweat and blood lactate were unrelated through strenuous exercise [6]. Finally, the authors also extensively investigated the origin and relationship of sweat lactate to skin temperature, rate and duration of sweating [6].
In 1956, Yas Kuno published his second book on the subject of human sweat [7]. On the topic of sweat lactate, it is mentioned that sweat lactate appeared not to be filtered from the blood but produced in the glands. It is also reported that sweat lactate concentration was initially high and then falls when sweating becomes profuse. Isolated human eccrine sweat glands produced lactate in vitro and furthermore would increase the rate of lactate production in the presence of physiological concentrations of glucose [8]. The author compares the amount of lactate produced per sweat gland in vitro and in vivo (thermal sweating), showing that they correspond closely and therefore strengthening the hypothesis that lactate in sweat is a by-product of sweat gland metabolism.
Tracer studies [9] which involved injecting either 14C-labelled lactate or glucose and measuring the amount recovered gave evidence that sweat glands produce all of the excreted lactate and do not excrete blood lactate. In 1974, it was found that the adrenergic sweat rate is between five and ten times lower than the cholinergic sweat rate, but that lactate concentration was not found to significantly vary between the methods of stimulation [10]. Glucose utilisation by sweat glands during fasting was studied and it was found that lactate concentration in sweat dropped to a steady state of 19 % below a control after 3 days of fasting, whilst circulatory glucose dropped by 30–40 % [11]. This is strong evidence for the hypothesis that sweat glands rely entirely on glucose metabolism to function and have preferential access to glucose over other organs such as the brain or muscle when glucose is in short supply.
In 1977, Kenzo Sato wrote a well-cited article on the physiology of sweat secretion [12]. On the topic of energy metabolism, four different potential routes are highlighted, all of which involve the degradation of glucose. The author concludes that the most likely route of energy metabolism is oxidative phosphorylation of plasma glucose, with gland glycogen stores contributing minutely. Lactate excretion is accounted for purely as a by-product of the glycolytic activity within the sweat gland. The relationship between sweat rates and lactate concentrations is outlined, stating that they are generally inversely proportional.
Two studies compared lactate concentrations in thermally induced sweat from children with and without cystic fibrosis (CF) and found no difference in sweat lactate between the groups [13, 14]. A small, proof of principle, study was performed to establish whether sweat lactate monitoring would be a viable method for detecting pressure damage in soft tissue and concluded that sweat lactate is technically feasible as a monitoring method for pressure ischemia, although only if the sweat is collected from the area of interest [15]. A study on the effect of peripheral arterial occlusive disease on sweat lactate from the calf found that, consistent with other studies on ischemia, sweat rate was significantly lowered and sweat lactate concentration was significantly raised in the diseased group in comparison to the control group [16]. It was hypothesized that, as tissue oxygen perfusion is lower, the sweat glands increasingly rely on anaerobic glycolysis for energy and that this results in reduced output and greater sweat lactate concentration. The use of sweat analysis to detect soft tissue breakdown following pressure ischemia was investigated by a research group from Oxford [17]. Further work was published and the findings of these studies are discussed later in greater detail [17–20].
Between 2000 and 2004, a research group from the USA, led by Matt Green, published five research articles with a common theme of investigating sweat lactate. The first and arguably most important study provided the most compelling evidence that blood lactate and sweat lactate are not related [21]. Further articles investigated whether there were differences in sweat lactate between genders [22], whether differences exist between younger and middle-aged men [23] as well as between men with high and low aerobic fitness [24], and investigated the response of the sweat glands to environmental temperature [25].
Critical evaluation of literature by subject
Variations in sweat lactate depending on stimulus
Sweating is initiated by the hypothalamus, in response to a rise in core body temperature, by sending a signal via the sympathetic nervous system. In contrast to normal sympathetic postganglionic neurons which release norepinephrine, the neurons that terminate within sweat glands release acetylcholine, which then activates muscarinic receptors [12, 26]. Atropine, a competitive muscarinic acetylcholine receptor, has been shown to completely block thermoregulatory sweating [27]. Whilst acetylcholine is the primary neurotransmitter, the sweat gland is known to be innervated by both cholinergic and adrenergic nerve terminals [28]. Sweating can be stimulated in vivo and in vitro using both α-adrenergic and β-adrenergic agonists, although sweat production volume is much lower than when stimulated by cholinergic means [10].
As shown by the atropine study discussed above, adrenergic sweating (in response to epinephrine) is not a significant component of thermal sweat. Isolated sweat gland studies have shown that sweat production can be stimulated in vitro using epinephrine; lactate concentration of the adrenergic sweat was found to be similar to cholinergic sweat [8, 29]. There is evidence that, whilst neurogenic sweat is exclusively stimulated by acetylcholine, given a high enough concentration of circulating adrenaline, there will be a sweating response [30].
A number of studies on the effect of pilocarpine sweat stimulation on sweat lactate [31–33] found that stimulation of sweat using pilocarpine before exercise did not change the sweat lactate concentration during exercise in comparison to a control group. Restimulation with pilocarpine 20 min after an initial dose also preserved both sweat quantity and lactate concentrations over 30 min, whereas both declined in the control group, suggesting that even without exercise the sweat glands are capable of maintaining high sweat lactate concentrations (>20 mM) after 30 min.
The effect of induced metabolic alkalosis on sweat found that sweat pH increased significantly when NaHCO3 − was ingested prior to exercise [34]. Sweat lactate did increase but did not reach significance (p = 0.08). The authors suggested that the change in pH is caused by a change in reabsorptive duct function.
Other authors investigated the effect of hyperoxia, in the context of jet pilots, on sweat composition in males [35]. Concentration of sweat constituents were compared during heat stress for subjects breathing in normal air and 100 % oxygen and found a significant (p < 0.05) decrease in lactate concentration and a significant (p < 0.01) increase in sweat loss when the subjects were breathing 100 % oxygen.
Sweat lactate variation between modes of stimulation
Sweating is a physiological response to a number of stimuli such as the environmental conditions, physical exercise and a person’s emotional state. In this section, we will discuss whether there are any differences in sweat lactate concentrations depending on the stimulation method, focussing on the difference between thermally and exercise induced sweating since very little has been published on lactate within emotionally induced sweat. Further comparison will be drawn between exercise-induced sweat where the protocols had multiple exercise intensities.
Comparison between individual studies is made difficult by subject and protocol variations which have been shown to greatly affect the reported lactate concentrations. There are a number of articles that, whilst not directly comparing, make use of multiple stimulation methods and are therefore best suited to highlight any potential differences that may exist.
Sweat lactate variation with exercise intensity
A number of articles present data on sweat lactate concentration for exercising subjects but are not suitable for assessing variation with exercise intensity since they examine sweat lactate under a single mode of exercise [36, 37]. A number of studies were identified that employed protocols suitable for comparing sweat stimulated by endurance and exhaustive exercise with in some cases this being the explicit hypothesis of a study. In some studies, it was not stated whether the protocol was intended to result in entirely aerobic respiration or exceed the aerobic capacity of the subject; in those cases, we made the assessment ourselves based on factors such as respirometry data, blood lactate concentration and heart rates. The criteria used for categorisation was whether the exercise protocol employed by the authors of the research was likely to have caused the rise in blood lactate traditionally associated with exercise beyond the individuals’ lactate threshold. It is now known that blood lactate is not the cause of muscle fatigue per se, but remains an important indicator of oxygen-independent metabolism in muscles [38].
A total of nine studies were identified to provide a useful comparison, of which four present evidence that exercise intensity has no significant effect on sweat lactate concentration, while the other five present evidence that a significant relationship exists. For clarity, the two opposing cases will be discussed in turn, starting with those that present a significant relationship.
A three-subject study utilized a sedentary, a fit and a very fit subject (determined by their VO2max) to investigate whether a difference in sweat rate and lactate concentration exists across three modes of sweat stimulation: external heat load, constant exercise and incremental exercise [39]. In the incremental exercise test, which was classed as anaerobic, the sweat lactate concentration for all three subjects did not exhibit the classic decay observed in the constant exercise trials; the sweat lactate concentration remained constant and no significant difference (p > 0.05) was shown between the first and last measurements for the anaerobic exercise. Dilution due to sweat rate was unlikely to be the contributing factor for this difference between the constant and incremental exercise protocols, since sweat rates were comparable between the tests for the sedentary and very fit individual, and only the fit individual showed a large difference in sweat rate. The authors hypothesize that the difference in sweat lactate concentration between the constant and incremental exercise is that an increase in blood epinephrine levels during the more strenuous incremental exercise could have a vasoconstrictive effect on the sweat glands, and thereby lead to an increase on the reliance of anaerobic glycolysis. However the small sample size of this study is a concern.
A recent study also suggested a relationship between sweat lactate concentration and exercise intensity [40]; although in contrast to the previously discussed study, this study presents an inverse relationship. The study protocol had subjects (n = 8) performing three successive 30-min exercise bouts on a treadmill at 60, 70 and 80 % of their respective maximum age-predicted heart rates (HRmax). Since all subjects were able to complete the full 30-min bouts, this would suggest that even the highest intensity was not exhaustive; nonetheless, exercise intensity varied from easy to strenuous. Sweat lactate concentrations were significantly (p < 0.05) higher at 60 % HRmax compared with at 70 and 80 % HRmax and no significant difference was observed between 70 and 80 % HRmax. The authors also calculated the lactate excretion rate to compensate for sweat dilution at the higher intensities and found that, whilst no significant difference was observed between 70 and 80 % HRmax, both were significantly (p < 0.05) greater than at 60 % HRmax. These results show that at greater exercise intensities the subjects sweated a greater amount of a more dilute sweat, resulting in a greater total amount of lactate being excreted in comparison to exercise at a lower intensity. It is also possible that exercise intensity did not contribute to this trend and that this trend would have been observed when exercising for a total of 90 min at a steady intensity.
Evidence for a strong relationship between blood and sweat lactate concentrations was presented following a single subject study in which a volunteer cycled for 10 min at various work-loads [41, 42], elicitating a range of heart rate response from 109 to 165 bpm, which suggests that at the lightest work-load the exercise was fairly light and that at the highest work-load was close to exhaustive. A significant (p < 0.01) increase in sweat lactate was observed from the lowest to the highest work-load. Regression analysis showed a relationship between blood and sweat lactate (r = 0.88). However, these results were only obtained on a single subject. Earlier work by the same group analysed sweat samples from football players, walkers and table tennis players whilst they performed their respective sports [43]. The sweat lactate results showed that walkers (aerobic) had the lowest concentration of sweat lactate, followed by football players (anaerobic) and then table tennis players (anaerobic), who had the greatest concentration. The variability in sweat collection protocols between groups makes comparison difficult.
Research by a group that had developed a novel lactate biosensor [44] involved an undisclosed number of untrained subjects performing a 3,000 m endurance run and an exhaustive stair sprint. The average sweat lactate concentration for the endurance exercise was 43.7 mM and for the exhaustive exercise was 115.8 mM. The stair sprint only lasted 5 min whilst the endurance exercise lasted roughly 15 min; it is therefore likely that the difference in sweat lactate is due to the initially high sweat lactate concentration that is commonly observed rather than the difference in intensity, as initially high concentrations are observed in most studies of sweat lactate. However, no extensive validation studies appear to have been carried out on the biosensor.
A group of three articles from the same research group on sweat lactate using identical methodologies and utilising common results will be discussed collectively. These works attempted to establish whether high or low blood lactate concentrations had an effect on sweat lactate concentrations [21], whether gender differences existed in sweat lactate [22], and finally compared younger and middle-aged males [23]. The exercise protocol used in the studies comprises a constant load and an interval cycling trial, with both starting with a 15-min warm-up followed by a 15 min rest. The constant load trial involved the subject cycling at 40 % VO2max for 30 min and the interval trial involves cycling at 80 % VO2max for two 15-min bouts with a 1 min rest in between. Blood lactate concentrations were significantly (p < 0.05) raised in the interval cycling trials in comparison with the constant load trials. Sweat lactate concentrations showed no significant difference at any time point between the two trials. Sweat rates, derived from whole body weight difference before and after exercise, were also not seen to differ significantly between constant and interval trials. All three studies show that two trials that elicited significantly different blood lactate responses showed no differences in sweat rates due to equated work volume or sweat lactate concentrations.
Sweat lactate and ammonia concentrations changed with incremental cycling exercise [45] where the subjects (n = 10) were required to cycle until exhaustion as the work-load increased every 3.5 min, thereby encompassing both endurance and exhaustive exercise. Blood lactate measurements showed that subjects exceeded the lactate threshold before terminating the exercise bout. The sweat lactate response showed the typical decay curve and then reached a plateau despite exercise intensity increasing; at the start of exercising, the average lactate concentration was 31 mM compared with 12.1 mM at the point of exhaustion. This agreed with the earlier wide-ranging study on the lactate content in sweat [6] which included a small study into the effect of increasing blood lactate concentration on sweat lactate concentration. No difference in sweat lactate levels were observed between two trials, despite the latter significantly raising blood lactate.
In conclusion, there is still some ambiguity as to whether exercise intensity has a significant effect on sweat lactate concentration. Studies have shown sweat lactate rising [41–44], remaining level [39] and decreasing [21–23, 40, 45] in response to increased exercise intensity. Generally, it seems to be accepted that blood lactate is not cleared by the sweat glands and that raised blood lactate levels do not affect sweat lactate. Also, the rate of sweating has a marked effect, in that, as the intensity of exercise increases, this will lead to higher sweating rates with concurrent dilution of lactate. Therefore, some studies are limited in interpretation in that, if sweat rate is not monitored, then variations in sweat rate on the lactate concentration cannot be determined.
Thermally versus exercise induced sweat
The sweat lactate concentrations for three subjects exhibited a similar trend between an external heat load and a constant exercise trials—an initially high concentration (around 20 mM lactate) that decays over time. The regression trend lines were both found to be highly significant (p < 0.001) and no significant difference was observed between the slopes of the two tests; however, the small sample size must be a concern [39]. As described earlier, a small proof of principle study demonstrated average sweat lactate concentration for a heating trial of 22.1 mM, for an endurance exercise it was 43.7 mM and for an exhaustive exercise trial a concentration of 115.8 mM was observed.
Studies aimed at investigating sweat lactate, urea and ammonia in highly trained rugby players before and after a match have been reported [46]. The subjects (n = 15) had sweat and plasma samples taken before and during the match, as well as 24, 48 and 72 h after the match; with the exception of the sample during the match, the sweat samples were taken during a 60-min sauna session (81 °C and 87 % humidity). The sweat lactate concentration of the sweat samples showed no significant differences between the samples obtained during the match (exercise) and any of the other samples (thermal). When corrected for sweat rate, the authors claim that secretion rates were significantly (p < 0.05) different in the samples following the match compared with the match sample; no significant difference was seen between the pre-match and the match sample. A significant correlation was observed however between sweat rate and sweat lactate concentration (r = 0.52, p < 0.01).
Others sought to establish links between d-lactate, l-lactate, pyruvate and methylglyoxal in blood, urine and sweat before and after exercise [47]. Instead of compensating for sweat rate, they reported concentrations in relation to sodium ions as well as the actual concentrations. These authors found a significant increase in sweat lactate when comparing sweat induced by exercise or thermal stimulation. Conversely, there was a significant decrease in the concentration in relation to sodium ions. Although a rise in sweat lactate in response to exercise was reported, only one measurement was made and so development over time cannot be assessed.
The sweat lactate response for subjects cycling at either 18 or 30 °C [25] did show how temperature can affect sweat response, although this does not compare sweat obtained by either thermal or exercise. Subjects cycled on different occasions for 60 min at 18 or 30 °C wet bulb globe temperature. It was found that at 30 °C the subjects sweated significantly (p < 0.05) more than at 18 °C, 1,382 ± 335 and 611 ± 311 ml h−1 respectively. Sweat lactate concentration was significantly (p < 0.05) higher at 18 °C compared with 30 °C at all sampling times. Correcting for sweat rates showed that total lactate excretion at 30 °C was significantly (p < 0.05) higher than at 18 °C, 14.7 ± 3.4 and 9.1 ± 3.4 mmol, respectively, demonstrating that, at higher environmental temperatures, the internal heat load of the subjects will rise much more quickly and therefore lead to a greater sweat rate of more dilute sweat.
In summary, there have not been many studies which allow a useful comparison of sweat lactate concentrations from thermally- or exercise-induced sweating to be made. The best evidence is presented in the study by Fellmann et al. which shows no significant difference in sweat lactate between thermally-induced or endurance exercise-induced sweat [39].
Sweat lactate variation among body regions
Most of the research that has been described in this review has relied on sweat collection from specific parts of the body, but site selection criteria appears to be largely based on the convenience of collection. The literature specifically testing and discussing site variability of sweat lactate is very limited, although some literature compares sweat output without investigating lactate [48, 49].
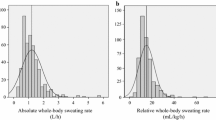
A more detailed article on the topic of sweat composition variation was not published until 2000 [50]. The authors compared the sweat composition of 10 males at 11 various sites of the body (forehead, chest, scapula, abdomen, lower back, upper arm, forearm, hand, thigh, calf and foot), as well as the whole body using a wash-down technique, and found that sweat lactate variation among individuals at any site on the body was very high. They also found that regional variations were significant whereas, in contrast, they found whole-body sweat lactate concentrations to be fairly consistent. If this is truly indicative of sweat gland function, then this could significantly affect the design of future studies and calls into question the validity of comparing studies with one another. For example, this study found that the forehead and foot sweat lactate concentrations were 6.50 ± 2.06 and 12.99 ± 2.39 mM, respectively. The reliability of the results are questioned by the authors themselves since they point out that whole-body sweat lactate concentration was found to be 5.87 ± 0.66 mM and every regional sample exceeded this. Using proportional means designed to estimate whole-body sweat composition from either four or eight regional measurements, it was shown that all composition values were overestimated. In the case of sweat lactate concentration, the formulas predicted 8.45 ± 1.83 mM (mean of 8 sites of lactate measurements) and 8.14 ± 2.00 mM (mean of 4 sites of lactate measurement); both very much higher than the 5.87 ± 0.66 mM that was measured for the whole body. The authors suggested that the wash-down technique could be the source of error. In this case, the wide variation found among regional sites would still be valid. Another potential source of discrepancy is that water will be lost via evaporation, thereby increasing apparent lactate concentration. A previous article by this research group studied the regional variations in sweat rate and the onset times of the 11 sites [51].
Earlier work measured sweat lactate concentration at five different sites (torso, face, thigh, axilla and arm) [3], demonstrating variation among the sites from 16 mM on the face to over 30 mM on the thigh, compared to the results of the previously discussed study which reported 6.50 ± 2.06 and 8.52 ± 2.95 mM for the forehead and the thigh, respectively. The magnitudes of the values are very different, but both studies show a greater concentration at the thigh compared to the facial region. No comparison was made with whole-body concentrations, but this does support the hypothesis that regional variations do exist.
Whole-body sweat was compared with that obtained using an arm bag [5], in order to validate arm-bag collection as a valid experimental technique. The study also examined the effects of acclimatisation on sweat composition. The results showed that arm-bag sweat was much more highly concentrated than whole-body sweat for all metabolites, including lactate. As the author concludes, this does not necessarily reflect physiological differences since this could be due to hindered evaporation and subsequent heating of the arm beyond the environmental temperature. In any case, this study strongly precludes the use of arm-bag sweat as a valid means of measuring sweat composition.
Research on the use of sweat analysis to investigate pressure ischemia included a trial measuring lactate concentration and total lactate amount from four sites on the body [18]. Two sites were around the hip region (ischium and sacrum), with measurements of both concentration and amount of lactate indicating these sites to be very similar but significantly lower than sweat lactate concentrations at the forearm and calf (p < 0.05). Correcting for sweat rate showed that the lactate amount secreted was actually lowest in the calf and highest in the forearm, with the difference between the two being significant (p < 0.05).
Inter-individual physiological variability
Effects of gender, age and fitness level
In general, the literature describes research that was performed using exclusively male subjects; only one article, which presented research on females alone [52], and a handful of articles utilising a mixed group of subjects were found. The majority conclusion from the literature is that gender does not affect lactate concentration. There is evidence that sweat rate is increased in males and therefore total lactate output is higher. It is known that women in general have a lower sweat rate than men, with some authors stating that this corresponds with greater sweating efficiency; i.e., women require less sweat output to effectively regulate their core temperature [53, 54].
The most comprehensive study of gender differences in sweat lactate was written by Green et al. [21] and utilized six men and six women with both groups being of a similar age, body fat and VO2max. In both steady state and interval exercise, they found no difference between genders in sweat lactate concentration or blood lactate concentration. This study found that men sweat significantly more and therefore produce a greater total lactate amount than women (p < 0.05).
A study on the effect of age and gender on sweat composition found no significant differences in sweat lactate concentration between men (n = 8) and women (n = 8) or boys (n = 18) and girls (n = 15) whilst performing using two 10-min bouts of moderate exercise in a hot environment (42 °C and 20 % relative humidity) [55]. The ages of the participants were 10.5 ± 1.8 years for girls, 9.9 ± 1.5 years for boys, 21.5 ± 0.7 years for women and 23.4 ± 2.0 years for men. Total sweat lactate was found to be higher in men than women and higher in girls than boys, although neither difference reached significance. After the first bout, there were significantly (p < 0.05) higher sweat lactate concentrations in the children compared to their adult equivalents; this difference was not significant in the second bout. Correcting for body weight and time showed that all four groups were not significantly different; however, a more suitable correction would have been for body surface area. The total amount of lactate lost through sweat from both bouts was significantly lower in the children compared to the adults (p < 0.05); this is to be expected since the adults produced far greater quantities of sweat, again demonstrating that maturity has an effect on sweat gland metabolism.
Another study presented separate results for male and female participants [56], but no statistical treatment was applied when comparing the gender differences. Results were published as the median and range for the various age groups within the genders. Without the raw data or appropriate statistical treatments, it is impossible to say whether these results show a significant difference between genders. The age brackets were spaced 10 years apart at 6–15, 16–25, 26–35, 36–45 and 46–55 years old; unfortunately, the 6- to 15-year-old bracket would encompass children of varying physical maturity including some which are likely to be almost fully developed; this distinctly limits this study’s application to the hypothesis that physical maturity affects sweat lactate. Also, the cut-off points are somewhat arbitrary, since if there is a spread of ages across each group then it will become harder to demonstrate significant differences between adjoining groups; when there is a clear separation between groups, then comparisons between them are more meaningful. The sweat lactate concentration results show that the lowest age bracket had a significantly lower sweat lactate concentration than the 16- to 25-year-old bracket (p < 0.02 for males, p < 0.05 for females). For males, there was also a significant rise in sweat lactate concentration in the 26- to 35-year-old bracket compared to those either side (p < 0.02). The authors explain that they found sweat lactate concentration to be highly dependent on sweat gland activity, suggesting that children’s low sweat lactate concentration is due to their low sweat gland activity. They fail to relate sweat lactate concentration with sweat rate which could be expected to balance these differences, i.e. a child may sweat less and therefore produce less lactate, but still have a similar sweat lactate concentration to an adult. Again, this appears to demonstrate that eccrine gland metabolism varies with age.
A small study (2 male and 2 female subjects), focused on measurement of lactate in sweat in response to heat and moderate exercise [57], showed no differences between the genders in sweat lactate concentration. Females sweat less volume and have more sweat glands per surface area than males, therefore the lack of difference in lactate concentration could indicate differences in eccrine gland metabolism.
It is well known that apocrine sweat production is dependent on pubertal development; it is also known that children in general sweat less than adults. To test whether there are differences in sweat gland metabolism in children depending on their physical maturity, 36 boys were graded into either prepubertal (n = 16), midpubertal (n = 15) or late pubertal (n = 5) groups and their sweat in response to moderate exercise in heat (42 °C and 18 % relative humidity) was tested [58]. Their results show a significant rise in sweat rate as physical maturity increases as well as showing that sweat lactate concentration was initially higher in the least mature group in comparison to the most mature. Correcting for lactate excretion rate per gland showed a significant difference between the groups with the lactate excretion rate per gland increasing with physical maturity (p = 0.08), thereby demonstrating that eccrine gland metabolism is related to age.
A comparison of sweat lactate [23] involved six younger men (25.8 ± 1.5 years) and six middle-aged men (51.5 ± 3.8 years) with similar VO2max, height, weight, body fat percentage and surface area. They completed both a constant load and an interval exercise with both blood and sweat being analysed. Results showed no significant differences between the groups in sweat rate, total lactate excretion or sweat lactate concentration for either exercise, with the authors concluding that there are minimal differences in sweat gland metabolism between these age groups.
The effect of physical fitness on sweat gland metabolism is of particular interest since it indicates whether sweat glands can be trained to work more efficiently and could potentially provide a metric to quantify fitness. Also, heat acclimatisation could have an effect, leading to increased sweating and decreased lactate concentrations. Fitness is difficult to quantify in itself since there are many different forms of fitness such as endurance (aerobic), sprinting ability (anaerobic) and strength (anaerobic). Fitness can be summarised as adaptation to the physical challenges in which one participates. A commonly used metric for quantifying aerobic fitness is VO2max, a measure of the peak oxygen consumption of an individual; as fitness increases, so too does VO2max. This measure is biased towards endurance, i.e. aerobic, fitness, as it reflects the body’s ability to effectively deliver and use oxygen.
It is well established that with increased physical fitness there is an increase in sweating protection. It follows that sweat composition may also vary with physical fitness. The literature appears to be split on whether physical fitness significantly affects sweat lactate concentration or total output. Four articles were identified as relevant to the discussion of relating sweat lactate with fitness; three of which claim to support the hypothesis that fitness affects sweat lactate.
A three-subject study (sedentary, fit and very fit by VO2max) [39] utilized exercise at constant relative maximal aerobic power and exercise at increasing workloads. Sweat rate was positively correlated with fitness across all both workloads. The mean sweat lactate concentration during the increasing work load study showed a significant inverse relationship with fitness level (p < 0.001 significant difference between sedentary and both fit and very fit, p < 0.025 significant difference between fit and very fit).
A later study of 22 males aimed to investigate the effect of physical training on exercise-induced sweating [41, 42]. The subjects were graded as either sedentary (S) or trained (T) by measurements of their VO2max (S = 33.4 ± 5.4 ml min−1 kg−1, T = 60.1 ± 6.1 ml min−1 kg−1, p < 0.001 significant difference). The exercise protocol for stimulating sweating was a bout on a bicycle ergometer set at a constant load of 3 kpm for 10 min at work rates of 900 kpm min−1; the authors state that this was not maximal aerobic power for any of the subjects, and in fact utilising a standard workload means that means fit and less fit subjects exert a different percentage of their maximal capacity. The results showed that sweat rate was significantly higher (p < 0.05) in sedentary individuals compared with trained subjects. This is most likely due to the exercise protocol not being strenuous enough to cause a significant rise in internal heat load for the trained individuals and therefore not eliciting a large sweating response. Whilst the exercise protocol was the same for all subjects, the degree of stress would have been very different; it is for this reason that most studies use relative protocols. The difference between the two groups is highlighted in blood lactate, in which the sedentary group showed a significant increase (p < 0.001) over the trained group. A significant difference (p < 0.001) is also shown in sweat lactate; the sedentary group had a higher sweat lactate concentration in comparison to the trained group (37.5 ± 7.9 and 24.5 ± 4.9 mM, respectively). However, lactate levels could well be affected by the amount of sweating, since higher levels of sweating can lead to a dilution of lactate. Using regression analysis, the authors demonstrated the following significant relationships: a positive relationship between blood lactate and sweat lactate (r = 0.646, p < 0.01), a negative relationship between VO2max and sweat lactate (r = 0.547, p < 0.01), and a negative relationship between sweat rate and VO2 max (r = 0.463, p < 0.05). Whilst these relationships may show a significant physiological difference in sweat lactate depending on fitness level, it is also possible that it is a reflection of the exercise protocol employed, i.e. as discussed above, the trained group most likely did not experience as great an internal heat load.
A different study compared the sweat rate, total lactate secretion and sweat lactate concentration of ten women [52], five of whom were classified as sedentary and the other five as active depending on their VO2max results (41.0 ± 1.62 and 51.2 ± 3.20 ml kg−1 min−1, respectively). The exercise protocol employed for sweat stimulation was a 60-min bout at 70 % of the subjects VO2max on a friction-braked cycle ergometer in a laboratory held at between 17 and 21 °C dry bulb and 11 and 21 °C wet bulb. Sweat collection was achieved using a full body wash-down protocol using known quantities of distilled water so that sweat volume could be calculated. The results showed that, in agreement with common observation, the active group sweated significantly (p < 0.05) more than the sedentary group. Blood lactate in the sedentary group rose consistently throughout the protocol, whereas it levelled off after 15 min in the active group; this most likely shows the improved lactate clearing mechanism of the active subjects compared to the sedentary subjects. Sweat lactate concentration in the sedentary group was significantly (p < 0.05) higher than the active group (100.4 ± 32.37 vs. 42.6 ± 14.08 mM, respectively); these are much higher concentrations than normally seen in studies of sweat lactate. Total sweat lactate amount was also significantly (p < 0.05) greater in the sedentary group compared to the active group (50.2 ± 6.61 vs. 29.8 ± 5.03 mmol, respectively). The results showed that sweat rate and lactate concentration were inversely correlated (r = −0.79, p < 0.01). Regression analysis showed that blood lactate concentration was not significantly correlated with the rate of sweat lactate excretion; <1 % of the variance in sweat lactate secretion between subjects could be accounted for by changes in blood lactate concentration. The authors make a number of hypotheses as to why an inverse relationship was observed between sweat rates and lactate excretion, including increased reabsorption of lactate or decreased reabsorption of water at the sweat gland, improved blood flow at the surface of the skin leading to more aerobically produced sweat, and improved metabolic efficiency of the sweat gland. Previous workers have concluded that, even despite the relatively high lactate concentration, the majority of sweat gland metabolism is aerobic [12]. The hypothesis the authors concluded with was that active subjects may have lower circulating catecholamine levels during exercise leading to sweat that has lower lactate levels.
The most recent study [25] comparing sweat lactate concentrations in subjects of varying fitness was comprised of 13 young males, split into two groups depending on the VO2peak achieved during a trial [≥58 ml kg−1 min−1 (n = 6) and ≤49 ml kg−1 min−1 (n = 7)]. Given the trial protocol employed in this study, VO2peak is analogous to the VO2max test used in other studies. The exercise protocol for stimulating sweating was a 60-min bout of cycling on a cycle ergometer set at a resistance designed to achieve exercise intensity at 90 % of the subject’s ventilatory threshold. The results showed that males with high aerobic fitness had a significantly (p < 0.05) higher sweat rate compared to those with low aerobic fitness, consistent with common observation. No significant (p > 0.05) difference in sweat lactate concentration between the two groups was observed at any time interval.
In conclusion, the degree to which physical fitness affects sweat lactate is still unclear. Limited evidence is presented for an inverse relationship between sweat lactate and physical fitness. This relationship may become clearer if total sweat rates are taken into account, since high sweat rates tend to lead to dilution of lactate; however, total rates were not recorded for some studies. However, in many cases, total sweat rate was not recorded.
Effect of climate adaptation on sweat lactate
Research into the effect of acclimatisation on lactate content in sweat is very limited. Studies on thermoregulatory responses to hot climates have shown that in general acclimatised individuals can sustain higher sweat rates than non-acclimatised individuals [48, 59, 60]. It follows that, with changes to sweat gland metabolism, changes to sweat composition may also be seen.
Early work presented results that showed a distinct reduction in lactic acid concentration over the space of 20 days of acclimatisation in a male subject [4]. The authors presented this as analogous to trained muscles working more efficiently. However, these results were obtained using an arm-bag, which they later showed to not truly reflect whole-body concentrations [5]. Three years later, a much more detailed article was published by the same group which showed different results [6], i.e. that sweat lactate concentration does not vary with acclimatisation or changes in sweat rate, although total lactate output was dependent on sweat output, both of which increased with acclimatisation. After 13 days of acclimatisation, a subject’s arm-bag sweat lactate concentration fell from 24.4 to 12.3 mM with the whole-body sweat lactate concentration falling from 9.4 to 8.1 mM.
Potential applications for sweat lactate measurements
Detection of pressure ischemia
Pressure ischemia describes the condition of reduced oxygen perfusion in tissue due to an applied force. This can in turn lead to decubitus ulcers if perfusion remains low for an extended period of time. This is a critical condition within hospitals and care homes for the elderly or disabled, since patients are often not capable of making positional adjustments to relieve the ischemia themselves. Currently, nurses or care assistants are making manual checks of common pressure points to detect the early signs of decubitus, so allowing steps to be taken to prevent them from developing.
It has been shown that reduced oxygen tissue perfusion lowers sweat rate [1] and raises sweat lactate in an occluded arm [4, 61]. Initial studies into the measurement of sweat composition as a diagnostic marker for pressure ischemia presented results that showed small pressure indentation resulted in similar sweat composition to a whole occluded arm [15], demonstrating that local tissue oxygen perfusion was the critical factor and not just blood oxygenation per se.
A series of articles [17–20] show that sweat lactate is potentially a very useful early warning indicator of pressure ischemia. An indentation study showed significant (p < 0.01) elevation in sweat lactate. Short-term occlusion of an arm did not yield a significant rise, suggesting that it takes time for oxygen perfusion of the sweat gland to affect sweat output to measureable levels. Short-term (around 50 min) sitting in a wheelchair or lying down also did not significantly raise sweat lactate. A subsequent study investigated much longer collection times, but only in three subjects, one of which had cerebral palsy and a history of decubitus. After 9 h, they found that the two control patients, neither of which had exerted pressure on the collection site, had significantly lower sweat lactate than the cerebral palsy sufferer who was sat in a stationary position for the entire duration. A further study, comprised of 11 debilitated subjects, found that basal sweat lactate in the unloaded state was significantly higher for the debilitated group than able-bodied controls. Furthermore, sweat lactate rose significantly in these patients when loading was applied to the sites. Finally, a study was performed on able-bodied subjects in which varying loads were applied to their backs; a significant correlation between applied load and sweat lactate concentration being found. Currently, the monitoring of sweat lactate would appear to be a potential application for the prevention of developing decubitus. Publications by the European Pressure Ulcer Advisory Board (EPUAB) have concluded that this is a research area of interest [62, 63]. They also mention that a biosensor suitable for detecting sweat lactate at the pressure sites in situ would be beneficial.
Tissue perfusion
The effect of peripheral arterial occlusive disease on sweat lactate from the calf [16] showed, consistent with other studies on ischemia, that sweat rate was significantly lowered and that sweat lactate concentration was significantly raised in a diseased group in comparison to a control group. It is hypothesised that, as tissue oxygen perfusion is lower, the sweat glands increasingly rely on anaerobic glycolysis for energy and that this results in reduced output and greater sweat lactate concentration.
Currently, there are no simple diagnostic tools for monitoring tissue perfusion in patients where this is a concern. We strongly believe that continuous monitoring of sweat lactate could yield vital data about the extent of tissue perfusion and crucially detect whether a patient’s condition is deteriorating or improving, thereby allowing clinicians to adapt treatment with greater speed.
Diagnosis of cystic fibrosis
Cystic fibrosis is characterised by increased sodium and chloride sweat concentrations; this forms the basis of newborn early screening programs. Since cystic fibrosis impairs lung function, it is conceivable that this condition could lead to decreased oxygenation, especially during exercise and an increase in anaerobic metabolism leading to higher lactate levels. Should this reduced oxygenation affect sweat gland metabolism, patients could display increased sweat lactate. Only two studies appear to have been carried out, showing that there are no significant differences in sweat lactate between cystic fibrosis patients and control subjects. One study exposed 6 cystic fibrosis and 11 normal children (5 months to 14 years old) to external thermal load (45 °C) and analysed sweat taken from the forehead [13]. Total lactate was shown to increase with sweat rate, but there was no significant difference between the two groups. In another study, examination of single sweat glands from healthy individuals and cystic fibrosis patients showed similar levels of lactate and bicarbonate production at similar sweat rates [14].
Alternative to blood lactate measurements
Blood lactate is of critical importance in the field of sports science as well as medicine. Determination of blood lactate is by necessity invasive and therefore difficult to perform continuously. A non-invasive alternative would in this context be very well received within both the sports science and medical communities. However, the overwhelming majority of the literature indicates that that blood and sweat lactate concentration are independent of one another since lactate within sweat is entirely a by-product of sweat gland metabolism, and evidence from a wide variety of studies can be used to support this view [8, 21, 40, 45, 46].
Other applications
Two other potential applications of sweat lactate have been identified but no follow-up work performed. One application is the use of sweat composition as a diagnostic marker of panic disorder (PD) [64]. This is a paroxysmal neuropsychiatric disorder characterised by recurring severe panic attacks. Current diagnosis is purely based on psychological factors as described in the American Psychiatric Associations’ diagnostic manual [65]. Significant differences were observed between patients with active PD (n = 10) compared with both patients in remission (n = 9) and control subjects (n = 11) in sweat lactate concentration (p < 0.05), sweat glucose concentration (p < 0.001) and sweat magnesium concentration (p < 0.05). Significant differences between patients with active PD and patients with PD in remission were observed between sweat sodium concentration (p < 0.01), sweat potassium concentration (p < 0.05) and sweat chloride concentration (p < 0.05); it is possible that these would be useful as indicators for successful treatment. The authors did not find any significant difference in blood parameters of the three groups and proposed that sweat analysis could potentially be used to diagnose panic disorder.
Application of sweat lactate measurements towards the diagnosis of Frey’s Syndrome has been proposed and a biosensor developed for this purpose [66, 67]. Frey’s Syndrome is characterised by increased sweating around the jaw in response to food stimuli (gustatory sweating). It is either congenital or more often brought on by a full parotidectomy (the removal of the parotid gland). Traditional diagnosis is the use of iodine and starch to visualise sweating. The authors suggest that this is subjective and that lactate measurements of the skin would be a more quantitative measure. Samples from 12 patients with Frey’s syndrome were analysed using biosensors for lactate and amino acids [66]. The levels of lactate could be successfully measured using the biosensor (the amino acid biosensor was too insensitive). They conclude that it is possible to detect increased sweating associated with Frey’s Syndrome using their methodology, but that no additional information regarding the severity of the condition could be obtained. This appears to be the only study made on this topic.
Concluding remarks
In this review, we have attempted to describe many of the factors that affect sweat lactate concentration. It appears that there are several important conclusions that can be drawn. The first is that the actual collection of the sweat is important, with both the sites of the body used and the methods of collection having major effects on measured lactate concentrations. There appears to be very little effect of factors such as age or gender on the concentration of lactate, whereas there is some evidence that factors such as fitness and the type of exercise have significant effects. One potential application of sweat lactate determination would be if it were possible to use it as a non-invasive method of determining blood lactate; however, many studies unfortunately indicate that there is no correlation and the level of sweat lactate is simply a function of sweat gland metabolism. A number of other potential applications have been described, one of which is the possible use of sweat lactate as an early indicator of ischemic decubitus.
References
Kuno Y (1934) The physiology of human perspiration. Churchill, London
Whitehouse AGR (1935) The dissolved constituents of human sweat. Proc R Soc Lond B 11:139–154
Mickelsen O, Keys A (1943) The composition of sweat, with special reference to the vitamins. J Biol Chem 149:479–490
Weiner JS, Heyningen REV (1949) Lactic acid and sweat gland function. Nature 164:351–352
Heyningen REV, Weiner JS (1952) A comparison of arm-bag sweat and body sweat. J Physiol 116:395–403
Weiner JS, Heyningen REV (1952) Observations on lactate content of sweat. J Appl Physiol 4:733–744
Kuno Y (1956) Human perspiration. Thomas, Springfield
Wolfe S, Cage G, Epstein M, Tice L, Miller H, Gordon RS Jr (1970) Metabolic studies of isolated human eccrine sweat glands. J Clin Invest 49:1880–1884
Gordon RS Jr, Thompson RH, Muenzer J, Thrasher D (1971) Sweat lactate in man is derived from blood glucose. J Appl Physiol 31:713–716
Sato F, Burgers M, Sato K (1974) Some characteristics of adrenergic human eccrine sweating. Experientia 30:40–41
Benson JW Jr, Buja ML, Thompson RH, Gordon RS Jr (1974) Glucose utilization by sweat glands during fasting in man. J Invest Dermatol 63:287–291
Sato K (1977) The physiology, pharmacology, and biochemistry of the eccrine sweat gland. Rev Physiol Biochem Pharmacol 79:51–131
Fellmann N, Labbe A, Gachon AM, Coudert J (1985) Thermal sweat lactate in cystic fibrosis and in normal children. Eur J Appl Physiol Occ Phys 54:511–516
Bijman J, Quinton PM (1987) Lactate and bicarbonate uptake in the sweat duct of cystic fibrosis and normal subjects. Pediat Res 21:79–82
Ferguson-Pell M, Hagisawa S (1988) Biochemical changes in sweat following prolonged ischemia. J Rehabil Res Devel 25:57–62
Fellmann N, Fabry R, Coudert J (1989) Calf sweat lactate in peripheral arterial occlusive disease. Am J Physiol Heart Circ Physiol 257:H395–H398
Polliack A, Taylor R, Bader DL (1993) Analysis of sweat during soft tissue breakdown following pressure ischemia. J Rehabil Res Develop 30:250–259
Taylor RP, Polliack AA, Bader DL (1994) The analysis of metabolites in human sweat: analytical methods and potential application to investigation of pressure ischaemia of soft tissues. Ann Clin Biochem 31:18–24
Polliack A, Taylor R, Bader DL (1997) Sweat analysis following pressure ischaemia in a group of debilitated subjects. J Rehabil Res Dev 34:303–308
Knight SL, Taylor RP, Polliack AA, Bader DL (2001) Establishing predictive indicators for the status of loaded soft tissues. J Appl Physiol 90:2231–2237
Green JM, Bishop PA, Muir IH, McLester JRJ, Heath HE (2000) Effects of high and low blood lactate concentrations on sweat lactate response. Int J Sports Med 21:556–560
Green JM, Bishop PA, Muir IH, Lomax RG (2000) Gender differences in sweat lactate. Eur J Appl Physiol 82:230–235
Green JM, Bishop PA, Muir IH, Lomax RG (2001) Lactate-sweat relationships in younger and middle-aged men. J Aging Phys Act 9:67–77
Green JM, Pritchett RC, Crews TR, McLester JR, Tucker DC (2004) Sweat lactate response between males with high and low aerobic fitness. Eur J Appl Physiol 91:1–6
Green JM, Pritchett RC, Tucker DC, Crews TR, McLester JR (2004) Sweat lactate response during cycling at 30 °C and 18 °C WBGT. J Sports Sci 22:321–327
Sato K (1993) The mechanism of eccrine sweat secretion. Perspectives in exercise science and sports medicine. Exerc Heat Thermoregul 6:85–118
Rodman MJ (1952) The anhidrotic action of atropine on human thermoregulatory sweating. J Am Pharm Assoc 41:484–487
Quinton PM (1987) Physiology of sweat secretion. Kidney Int 32I:S102–S108
Dobson RL, Sato K (1972) The secretion of salt and water by the eccrine sweat gland. Arch Dermatol 105:366–370
Foster KG, Ginsburg J, Weiner JS (1967) Adrenaline and sweating in man. J Physiol 191:131P–132P
Javle H, Keaney NP, Smy JR, Dillon S, Lee M (1989) Lactate excretion in sweat produced with and without pharmacological stimulation before and during steady state exercise. Brit J Clin Pharmacol 28:746–747
Javle H, Keaney NP, Smy JR, Lee M, Dillon S (1990) The effect of late restimulation with pilocarpine on the output of lactate in sweat in volunteers. Br J Clin Pharmacol 29:636–637
Javle H, Keaney NP, Smy JR, Lee M, Dillon S (1990) The effect of restimulation with pilocarpine on the output of lactate in sweat. Br J Clin Pharmacol 29:150
Patterson MJ, Galloway SDR, Nimmo MA (2002) Effect of induced metabolic alkalosis on sweat composition in men. Acta Phys Scand 174:41–46
Iyer EM, Dikshit MB, Banerjee PK, Suryanarayana S (1983) 100 % Oxygen breathing during acute heat stress: effect on sweat composition. Aviat Space Environ Med 54:232–235
Faridnia MH, Palleschi G, Lubrano GJ, Guilbault GG (1993) Amperometric biosensor for determination of lactate in sweat. Anal Chim Acta 278:35–40
Cai X, Yan J, Chu H, Wu M, Tu Y (2010) An exercise degree monitoring biosensor based on electrochemiluminescent detection of lactate in sweat. Sens Act B 143:655–659
Robergs RA, Ghiasvand F, Parker D (2004) Biochemistry of exercise-induced metabolic acidosis. Am J Physiol Regul Integr Comp Physiol 287:R502–R516
Fellmann N, Grizard G, Coudert J (1983) Human frontal sweat rate and lactate concentration during heat exposure and exercise. J Appl Physiol Resp Environ Exerc Physiol 54:355–360
Buono MJ, Lee NVL, Miller PW (2010) The relationship between exercise intensity and the sweat lactate excretion rate. J Physiol Sci 60:103–107
Pilardeau PA, Chalumeau MT, Harichaux P, Vasseur P, Vaysse J, Garnier M (1988) Effect of physical training on exercise induced sweating in men. J Sports Med Phys Fit 28:176–180
Pilardeau PA, Lavie F, Vaysse J, Garnier M, Harichaux P, Margo JN, Chalumeau MT (1988) Effect of different work-loads on sweat production and composition in man. J Sports Med Phys Fit 28:247–252
Pilardeau P, Vaysse J, Garnier M, Joublin M, Valeri L (1979) Secretion of eccrine sweat glands during exercise. Br J Sports Med 13:118–121
Mitsubayashi K, Suzuki M, Tamiya E, Karube I (1994) Analysis of metabolites in sweat as a measure of physical condition. Anal Chim Acta 289:27–34
Ament W, Huizenga JR, Mook GA, Gips CH, Verkerke GJ (1997) Lactate and ammonia concentration in blood and sweat during incremental cycle ergometer exercise. Int J Sports Med 18:35–39
Alvear-Ordenes I, Garcia-Lopez D, De Paz J, Gonzalez-Gallego J (2005) Sweat lactate, ammonia, and urea in rugby players. Int J Sports Med 26:632
Kondoh Y, Kawase M, Ohmori S (1992) D-Lactate concentrations in blood, urine and sweat before and after exercise. Eur J Appl Physiol Occ Physiol 65:88–93
Weiner JS (1945) The regional distribution of sweating. J Physiol 104:32–40
Sato K, Dobson RL (1970) Regional and individual variations in the function of the human eccrine sweat gland. J Invest Dermatol 54:443–449
Patterson MJ, Galloway SDR, Nimmo MA (2000) Variations in regional sweat composition in normal human males. Expt Physiol 85:869–875
Cotter JD, Patterson MJ, Taylor NAS (1995) The topography of eccrine sweating in humans during exercise. Eur J Appl Physiol Occ Physiol 71:549–554
Lamont LS (1987) Sweat lactate secretion during exercise in relation to women’s aerobic capacity. J Appl Physiol 62:194–198
Frye AJ, Kamon E (1983) Sweating efficiency in acclimated men and women exercising in humid and dry heat. J Appl Physiol Resp Environ Exerc Physiol 54:972–977
Wyndham CH, Morrison JF, Williams CG (1965) Heat reactions of male and female Caucasians. J Appl Physiol 20:357–364
Meyer F, Laitano O, Bar-Or O, McDougall D, Heigenhauser GJF (2007) Effect of age and gender on sweat lactate and ammonia concentrations during exercise in the heat. Braz J Med Biol Res 40:135–143
Al-Tamer YY, Hadi EA (1994) Age dependent reference intervals of glucose, urea, protein, lactate and electrolytes in thermally induced sweat. Eur J Clin Chem Clin Biochem 32:71–77
Astrand I (1963) Lactate content in sweat. Acta Phys Scand 58:359–367
Falk B, Bar-Or O, MacDougall JD, McGillis L, Calvert R, Meyer F (1991) Sweat lactate in exercising children and adolescents of varying physical maturity. J Appl Physiol 71:1735–1740
Saat M, Sirisinghe RG, Singh R, Tochihara Y (2005) Effects of short-term exercise in the heat on thermoregulation, blood parameters, sweat secretion and sweat composition of tropic-dwelling subjects. J Physiol Anthrapol Appl Human Sci 24:541–549
Buono MJ, Martha SL, Heaney JH (2009) Peripheral sweat gland function is improved with humid heat acclimation. J Therm Biol 34:127–130
Heyningen REV, Weiner JS (1952) The effect of arterial occlusion on sweat composition. J Physiol 116:404–413
Bader D, Bouten C, Colin D, Oomens C (2005) Pressure ulcer research: current and future perspectives. Springer, London
Bader D, Oomens C (2006) Recent advances in pressure ulcer research. In: Romanelli M, Clark M, Cherry G, Colin D, Defloor T (eds) Science and practice of pressure ulcer management. Springer, London
Kukumberg P, Valkovic P, Blazicek P, Guth A, Martinkova J, Provaznik V, Jagla F (2009) Sweat: a potential marker of clinical activity in panic disorder. Neuroendocrin Lett 30:400–402
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders (DMS-IV-TR). American Psychiatric Association, Washington, DC
Laccourreye O, Bernard D, de Lacharière O, Bazin R, Jouffre V, Brasnu D (1994) Contribution of l lactate and amino-acid enzymatic biosensors for the analysis of Frey syndrome. Ann Otolaryngol Chir Cervicofac 111:347–352
Laccourreye O, Bernard D, Lacharriere OD, Bazin R, Brasnu D (1993) Frey’s syndrome analysis with biosensor: a preliminary study. Arch Otolaryngol Head Neck Surg 119:940–944
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Derbyshire, P.J., Barr, H., Davis, F. et al. Lactate in human sweat: a critical review of research to the present day. J Physiol Sci 62, 429–440 (2012). https://doi.org/10.1007/s12576-012-0213-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-012-0213-z