Abstract
Background
Dashboards are increasingly being used in sub-Saharan Africa (SSA) to support health policymaking and governance. However, their use has been mostly limited to routine care, not emergency services like emergency obstetric care (EmOC). To ensure a fit-for-purpose dashboard, we conducted an online survey with policymakers and researchers to understand key considerations needed for developing a policy-ready dashboard of geospatial access to EmOC in SSA.
Methods
Questionnaires targeting both stakeholder groups were pre-tested and disseminated in English, French, and Portuguese across SSA. We collected data on participants’ awareness of concern areas for geographic accessibility of EmOC and existing technological resources used for planning of EmOC services, the dynamic dashboard features preferences, and the dashboard's potential to tackle lack of geographic access to EmOC. Questions were asked as multiple-choice, Likert-scale, or open-ended. Descriptive statistics were used to summarise findings using frequencies or proportions. Free-text responses were recoded into themes where applicable.
Results
Among the 206 participants (88 policymakers and 118 researchers), 90% reported that rural areas and 23% that urban areas in their countries were affected by issues of geographic accessibility to EmOC. Five percent of policymakers and 38% of researchers were aware of the use of maps of EmOC facilities to guide planning of EmOC facility location. Regarding dashboard design, most visual components such as location of EmOC facilities had almost universal desirability; however, there were some exceptions. Nearly 70% of policymakers considered the socio-economic status of the population and households relevant to the dashboard. The desirability for a heatmap showing travel time to care was lower among policymakers (53%) than researchers (72%). Nearly 90% of participants considered three to four data updates per year or less frequent updates adequate for the dashboard. The potential usability of a dynamic dashboard was high amongst both policymakers (60%) and researchers (82%).
Conclusion
This study provides key considerations for developing a policy-ready dashboard for EmOC geographical accessibility in SSA. Efforts should now be targeted at establishing robust estimation of geographical accessibility metrics, integrated with existing health system data, and developing and maintaining the dashboard with up-to-date data to maximise impact in these settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Globally, about 295,000 women lose their lives due to complications of pregnancy and childbirth annually, with 66% of these deaths occurring in sub-Saharan Africa (SSA) [1]. Similarly, there are about two million stillbirths annually, and 58% of these deaths occur in SSA [2]. These deaths are mostly associated with complications of pregnancy and childbirth, such as bleeding, high blood pressure, infection, and abortion, which can be worsened by events happening between the onset of the complication and the time when the woman receives care [3]. However, it has long been established that delays in travel to access emergency obstetric care (EmOC) can lead to deaths of mothers and their unborn child(ren). Indeed, access to EmOC reduces maternal deaths by 15–50% and stillbirths by 45–75% [4]. EmOC is a package of nine clinical and surgical evidence-based interventions including parenteral antibiotics, uterotonic drugs, parenteral anticonvulsants, manual removal of placenta, removal of retained products of conception, assisted vaginal delivery, neonatal resuscitation, blood transfusion and caesarean section [5]. Before women needing EmOC can access care, they need to travel from the community or be referred from other facilities to health facilities with EmOC capacity. Delays in reaching such health facilities have significant negative impacts on pregnancy outcomes of mothers and newborns [6,7,8,9].
For policymakers and other pertinent stakeholders of health systems, addressing access barriers which pregnant women with obstetric emergencies face is an ethical obligation [10] and very much in line with achieving universal health coverage (UHC), which is a key component of the Sustainable Development Goal (SDG) 3 to reduce maternal mortality to 70 per 100,000 live births globally by 2030 [11, 12]. To support the EmOC service planning function of policymakers, including deciding location of new facilities, upgrading the existing facilities, or siting of ambulance services in SSA, researchers have mainly used modelled approaches to assess geographical accessibility [13]. However, modelled approaches, which are typically static and report one moment in time (depending on available data, this time might not be recent), do not reflect the dynamic reality of travel which may be affected by traffic, terrain difficulties, and weather conditions [14, 15]. For example, in Dhaka, Bangladesh, ignoring variability in traffic conditions results in as much as a three-fold overestimation of geographic accessibility to emergency healthcare [16]. In another study in Lagos, Nigeria, mean errors of > 45 min were estimated when modelled travel time was compared to actual travel time [14, 15].
Policymakers require closer-to-reality and up-to-date travel time estimates to be able to comprehensively assess geographic accessibility within their jurisdiction, which will translate to allowing them to effectively address the issue of EmOC access, as has been shown in Lagos, Nigeria [17]. To address this need, a new effort to develop an innovative policy-ready dynamic dashboard using closer-to-reality travel time estimates to EmOC in SSA is being championed as part of the ‘On Tackling In-transit delays for Mothers in Emergency’ (OnTIME) project [18]. Dashboards such as this have been used mostly in high-income countries and increasingly in low- and middle-income countries (LMICs) to support health policymaking. However, their use has been mostly limited to geographical accessibility to routine care, not emergency services like EmOC [19,20,21,22]. During the 2019 Coronavirus Disease pandemic, policy dashboards were put forward and ultimately aided the pandemic response of governments and international stakeholders [23, 24]. Dashboards allow a “visual display of the most important information needed to achieve one or more objectives; consolidated and arranged on a single screen so the information can be monitored at a glance” [25]. If available, such visual display would make recognising areas of poor EmOC geographical accessibility easier for policymakers and facilitate evidence-based policy response [17, 26]. To guide the development of such fit-for-purpose dashboard, guarantee its uptake, and promote ownership, it is essential to gather user needs at the development stage from individuals who will use the dashboard [27,28,29] As such, our objective in this study was to survey policymakers and researchers on considerations needed for developing a policy-ready dashboard of geospatial access to EmOC in SSA.
2 Methods
2.1 Study design
We conducted an online survey of policymakers and researchers involved in health service planning, including for EmOC services in SSA.
2.2 Survey questionnaire
The survey questionnaire was initially developed in English and translated into French and Portuguese by health professionals who are native speakers to capture at least one official language for every country in SSA. Two versions of the survey were designed, one for policymakers and the other for researchers, and were made available online via Mentimeter (Mentimeter, Stockholm, Sweden). Separate versions were deemed necessary to ensure that the tool was pitched at the level of understanding of technical jargon matching each stakeholder group, with more simplified language used in the tool targeting policymakers. The online questionnaire was piloted with target participants, resulting in minor language changes being made to the tool before it was socialised to prospective participants.
The survey started with a demographic section that collected information about the participants’ profession and the sub-Saharan African country in which they primarily worked as policymakers or conducted research on as researchers. The questionnaire consisted of three substantive sections collecting data on participants’ awareness of areas of concern of EmOC geographic accessibility and existing tools, dynamic online dashboard features preferences among participants and perceptions of the potential of dashboard applicability to tackle geographic access to EmOC. Across the three substantive sections, questions were structured in different formats, including multiple-choice, Likert-scale, and open-ended text. In the first section, we asked the participants to describe the areas in their country of work that were affected by poor geographic access to EmOC services and existing technological resources used for planning of EmOC services. The second section pertained to the dashboard design features that they deemed relevant and desirable. For this section, we enquired about preference for a pre-set list of dashboard visual components including a base geomap showing EmOC service points, a display of various travel barriers, a heatmap showing travel time, the socio-economic status of the population and households, carparks at EmOC facilities, and public transport access points. These visual components were based on insight garnered from previous research [17]. We also asked participants for their opinion on the spatial granularity at which EmOC accessibility indicators and metrics are to be presented for maximum relevance and what modelling scenarios in the dashboard would help support policymaking and improve geographic access to EmOC services. Lastly, we collected information on the frequency of updates. The final section of the survey tool focused on the participant’s perception of the future potential and usability of a dynamic dashboard in tackling geographic access to EmOC service. A copy of the questionnaire for the policymakers and researchers in all languages used for the survey is available in Additional file 1.
2.3 Recruitment of survey participants and data collection
The inclusion criteria for the survey were: policymakers currently working on EmOC service planning in SSA, and researchers interested in EmOC service planning in SSA, as established through their recent publication history and responses to screening questions while filling the online questionnaire. Using a quota sampling to ensure all countries in the region were represented [30], we targeted between two to four participants per country in SSA (48 countries in the sub-region, totalling 92-184 participants). Researchers were recruited through contact email addresses provided in published research on accessing critical maternal health services in SSA. Policymakers were recruited through targeted emails to national Ministries of Health from the listservs of the African Centres for Disease Control and Prevention and the West African Network of Emerging Leaders in Health Policy and Systems Research. We also distributed the survey through colleagues at the WHO’s Partnership for Maternal, Newborn and Child Health. Data collection for the online survey commenced on 1st August 2022 and continued until 30th November 2022. The emails inviting participants to the study include a link to the informed consent sheet (containing the participant information sheet and the certificate of consent), which participants must complete before accessing the online survey. The survey took approximately 20 min to complete.
2.4 Data analysis
Responses were exported from the online data collection portal as Microsoft Excel sheets. Translation of survey responses completed in French and Portuguese to English were carried out before data analysis. Subsequently, data cleaning was performed and the extent of missingness reported. Corresponding to the three substantive sections of the questionnaire, we conducted a descriptive analysis to summarise the data by stakeholder group (overall, policymakers, researchers); multiple-choice and Likert-scale questions are reported as frequencies and percentages and are visually presented as maps or bar charts. We compared the proportion of policymakers who gave certain responses with those of researchers. Each response in the participants’ free text responses were individually reviewed, coded as one of the original categories provided, where applicable, or recoded as a new category, following deliberations by co-authors who led the data analysis.
3 Results
3.1 Participants’ demographics
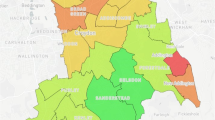
A total of 206 participants (118 researchers and 88 policymakers) took part in the survey. The commonest age group was 31 to 40 years old (42%). Of the 206 participants, 188 reported the SSA countries where they worked including 32 respondents (15%) who worked in Nigeria, 25 (13%) in Cameroon, and another 14 (7%) each in Kenya or Uganda. Altogether, 34 countries were represented on the survey (Fig. 1). Twenty participants did not specify their country of work.
3.2 Participants’ awareness of areas affected by poor EmOC geographic accessibility and related technological tools to improve access
Of the 153 participants who responded to this question, over 90% described areas affected by EmOC access issues as being characterised by rurality, including other similar characteristics, such as being hard-to-reach or sparsely populated. In comparison, 23% of participants described areas affected by EmOC access issues as typified by urbanicity, including peri-urban areas and urban peripheries. A higher percentage of policymakers (29%) had concern for urban areas compared to researchers (19%) (Fig. 2).
Disaggregated by country, respondents from the majority of represented countries in SSA only or mostly mentioned rural areas as areas affected by poor geographic access to EmOC. However, a relatively larger share of respondents working in the Democratic Republic of Congo (DR Congo) (five of seven respondents), Ghana (three of five respondents), and Nigeria (nine of 24 respondents) expressed concern about geographic access to EmOC in urban areas alone or both urban and rural areas. On the other hand, in Liberia, Ethiopia, Tanzania, for instance, no participants (at least five in each country) expressed concerns for geographic access to EmOC in urban areas (Fig. 3).
Forty-three percent of participants reported knowing at least one technological tool being used to deal with poor geographic access to EmOC in the countries where they worked – 38% of policymakers and 50% of researchers. Further, when asked about whether they were aware of the use of static digital maps of EmOC facilities to help guide service planning, 21% of the participants responded positively (5% among policymakers and 38% among researchers).
3.3 Dashboard design and functionality preferences
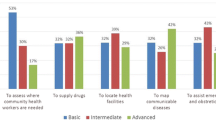
Regarding visual components desired by participants, the most highly regarded visual components were a map showing EmOC facilities’ locations (80% answered “somewhat relevant” and “absolutely essential”) and the display of various travel barriers (75%). When disaggregated by respondent type, there was consensus on desirability of several visual components of interest for policymakers and researchers, including a map of EmOC facilities (policymakers: 76%; researchers: 83%), travel barriers (e.g., difficult terrain and congested roads) (policymakers: 75%; researchers: 75%), public transport access points (policymakers: 64%; researchers: 57%), and carpark provided at EmOC facilities (policymakers: 29%; researchers: 25%). However, there were some notable differences. Almost 70% of policymakers considered the socio-economic status of the population and households relevant to the dashboard. The desirability for heatmap showing travel time was lower among policymakers (53%) when compared to researchers (72%), with a greater proportion of researchers (29%) feeling neutral about such heatmaps than policymakers (19%) (Fig. 4).
Most participants considered the facility catchment area of the buffer area as the most relevant spatial scale to display accessibility measures (91%). Both policymakers and researchers were largely in agreement with the levels of relevance of different spatial scales, except for the first administrative subdivision, which was more highly regarded among policymakers (53%) than researchers (22%) (Table 1).
Nearly 90% of participants considered three to four data updates per year or less frequent updates per year adequate for the dashboard, while 3% of researchers and no policymakers considered real-time updates relevant for the dashboard (Table 1).
When asked if 24/7 ambulance availability and various facility upgrade modelled scenarios on the dashboard might help with decision-making to improve geographic access to EmOC services, over 85% of respondents answered positively. About 50% of respondents also suggested other modelled scenarios they considered useful, with the most common being alternative human resource for health (HRH) scenarios – e.g., more skilled health personnel and other allied health personnel (Table 1).
3.4 Perception of the potential usability of the dashboard to tackle geographic access to EmOC
The potential usability of a dynamic dashboard such as the one proposed was high amongst all respondents (72% among non-missing responses). Disaggregated by stakeholder group, the potential usability of the dashboard amongst researchers was 82%, while amongst researchers was 60% (Table 2).
Two-thirds of the policymakers (67%) believed that the dashboard would add value and benefits to ministries of health and equivalent government health authorities, with 27% indicating that the dashboard will also benefit the work of other government departments and offices (including scientific offices, regional planning, road construction departments, etc.). On the other hand, researchers tended more to think that the dashboard would be of use to researchers, research institutes, and academic institutes (Table 2).
4 Discussion
We set out in this study to conduct a survey with policymakers and researchers on considerations needed for developing a policy-ready dashboard of geospatial access to EmOC in SSA. Of all the 206 respondents who took part in the survey, 90% reported that rural areas and 23% that urban areas in their countries were affected by issues of geographic accessibility to EmOC. Five percent of policymakers and 38% of researchers and 5% of policymakers were aware of the use of maps of EmOC facilities to guide planning of EmOC facility location. Regarding dashboard design, most visual components such as location of EmOC facilities had almost universal desirability; however, the desirability of socio-economic status of the population and households relevant and a heatmap showing travel time to care differed between policymakers and researchers. Nearly 90% of participants considered three to four data updates per year or fewer adequate for the dashboard. The potential usability of a dynamic dashboard was high amongst both policymakers (60%) and researchers (82%).
Participants almost unanimously thought that rural areas are affected by lack of EmOC access. About a quarter expressed urban areas are also affected by EmOC geographical accessibility issues and were mainly respondents from/working in DR Congo, Ghana, and Nigeria. When compared, policymakers tended more to be concerned about EmOC geographical accessibility in urban areas than researchers. The consensus on rural areas as areas of concerns is not surprising. Indeed, evidence in the literature shows that women in these areas have limited access to EmOC [31]. Though, recent evidence shows that women in urban and peri-urban areas also experience difficult access [32] and, in the largest SSA metropolis (Lagos), have higher odds of poor pregnancy outcomes for themselves and their newborns than those in rural areas [7, 9]. In our survey, since the countries from where a larger share of participants deemed urban as a problem are also countries that house two of the most-populated megacities (population > 10 million) in SSA [33], this observation might be because these are stakeholders who are already experiencing some of the impacts of urbanisation. It might also explain why policymakers tended more to be concerned about EmOC geographical accessibility in urban areas, as many typically live and work in such settings. Indeed, the challenges with access to healthcare in fast-growing, urbanising countries in SSA, including Ghana and Nigeria, have been flagged by researchers, who advocated for a need to rethink health systems more broadly in the context of urbanisation [34].
Participants reported some current use of digital technology to understand and address EmOC access issues. It is worth noting that the use of static maps showing facility locations was more frequently reported by researchers than policymakers. This is despite the fact that policymakers are the ones who need such evidence to support/guide EmOC service planning. As authors, we are aware of only two published studies reporting dashboards focused on geographical accessibility to health services in LMICs. There is one focused on primary health care in the Ifanadiana district of Tanzania called Lalana (https://research.pivot-dashboard.org/) [22] and another one which is concentrated on emergency healthcare services in Cali, Colombia called the AMORE Project (https://www.iquartil.net/proyectoamore/) [35]. There are probably other dashboards that are not publicly available. However, the 5% v. 38% awareness rate amongst policymakers and researchers that we observed in our survey suggests a significant disconnect between the creation of digital tools which is typically developed by researchers and their institutionalisation for supporting EmOC access policy actions. In a recently published qualitative study, policymakers specifically highlighted that digital tools that are dynamic and reflective of reality are more useful for decision-making [36]. We argue that these tools also need to be available beyond single districts of entire countries, as is the case with the two dashboards mentioned earlier, to realise their policy-influencing potential fully.
According to our survey respondents, the most highly desired visual component for a dynamic dashboard was a map showing facility locations. This desire is a legitimate need, as it is a fundamental requirement of a dashboard focused on EmOC access. The socio-economic status of populations and households was also reported as a desirable feature, especially among policymakers, indicating the interest in understanding access from the equity perspective, which is very much in line with the emphasis of the global community. Travel barriers showing difficult terrain and congested roads were also visual components of interest. We noted that compared to researchers, policymakers tended more to feel neutral about the relevance of a heatmap showing travel time. In static form, a heatmap based on closer-to-reality travel time estimates which showed congested roads was used to identify hotspots for EmOC geographical accessibility in Lagos, Nigeria [17]. The potential of these features may need to be brought to the attention of policymakers.
In addition, despite the premise of the survey being an online interactive dynamic dashboard showing EmOC access, the majority of survey participants considered three to four updates per year as adequate instead of more frequent updates (e.g., monthly) and no policymakers considered real-time updates as relevant. Bearing in mind the need to ensure optimum use of resources while assuring value for money of interventions such as this, which are aimed at improving outcomes for mothers and their newborns [37], this consideration will be critical for the sustainability of such dashboards. It also probably reflects that EmOC service planning from a supply side is not a real-time issue for policymakers. A dashboard updated three to four times a year or even less frequently, to aid in medium and long-term health policy planning is highly achievable. It minimises the need to collect primary data to update the inputs for the dashboard and efforts to re-run backend algorithms needed to keep the dashboard relevant for the times. In addition, most respondents wanted the dynamic dashboard to have the capacity to include modelled scenarios that offering comparison to the current situation in order to generate outputs to support better service planning and provision. In particular, the modelling scenarios of various locations and levels of ambulance availability and functionality of lower-tier health facilities, which could be upgraded for EmOC provision, were of interest to policymakers and researchers. For the latter, the functionality of EmOC facilities is known to vary even in settings such as urban areas where comprehensive EmOC is expected [38,39,40]. Ultimately, for such modelling features to work, there is a need to ensure that the dashboard is interlinked with other databases [41]. A feature allowing modelling various provision scenarios such as HRH, cost of service provision, or service outcomes could extend the utility of the dashboard for service planning and allow it to be more informative for policymakers in their efforts to identify areas of inequalities in healthcare utilisation, achieve cost-efficiency in provision of maternal and newborn health services and reduce maternal and neonatal morbidity and mortality [42, 43]. There are also other potential gains of a dashboard like this in SSA countries, including improving the routine health management information systems and enhancing accountability/stewardship of health systems and policymakers toward the population, as was the case with the routine immunisation dashboard implemented in Nigeria [21].
A key strength of the survey is that we covered almost all counties of SSA with 34 out of 48 countries in the sub-region included, representing 97% of the total population across the entire SSA region. However, there were some countries from which we could not secure any participant despite our best effort to disseminate the survey across all countries in SSA. We enlisted the major potential dashboard visual components in the survey but were unable to provide the participants with all the possibilities. Despite following up with an open-ended question in order to gauge other responses, respondents with little prior exposure to related tools were probably less able to provide further responses. Despite this, our findings provide critical insights that now need to be taken forward in the design and development of a user-friendly, context-specific, and customisable dashboard with the potential to inform and guide policymaking to address inequities in EmOC geographical accessibility in the sub-region.
In terms of the implication of our study findings for practice and policy, there is an appetite in government to improve EmOC geographical accessibility for women. However, efforts to do this are rarely data-driven [44, 45]. Dashboards like the one proposed in this study which will be built on up-to-date data on health facility functionality and closer-to-reality travel time [46] provide this much-needed evidence to support policymaking. The potential usability of similar dashboards may even extend beyond health service provision and the health sector in general and can benefit other crucial components of EmOC access, including road construction and urban and regional planning. However, currently, algorithms of navigation platforms which have the capacity to estimate closer-to-reality travel times, such as Google Maps (https://maps.google.com) developed by Google, Waze (https://waze.com) developed by Waze Mobile, Here WeGo (https://wego.here.com/) developed by HERE Global B.V., and the open-source, World Bank supported platform, OpenTraffic (http://opentraffic.io/) are more reflective of the situation in more urbanised settings compared to rural ones [15]. To put this in context, the team that worked on Lalana, which was done in a rural district, had to map over 100,000 buildings and 23,000 km of footpaths [22]. More work is needed to grow the functionality of the platforms and any resulting dashboards for rural areas, as these remain priority areas of inequities requiring attention. To ensure that when such dashboards become available, they are used, we have captured critical insights from policymakers and researchers that allow us to co-design a policy-ready dashboard study. At the minimum, a policy-ready dashboard should provide data on facility locations, the socio-economic status of populations and households, and travel barriers showing difficult terrain and congested roads. Its utility will be optimised if it is connected to other databases, and it can be updated quarterly. Some of the considerations highlighted by policymakers and researchers from their health system lens might be relevant for corollary dashboards at a facility-level and for demand-side dashboards for service users such as pregnant women.
In terms of future research, there is a need to test strategies aimed at augmenting uptake, utilisation, and fidelity of these dashboards amongst stakeholders when they are implemented [47] while also capturing impact stories on how it is making a difference in the functionality of service planners and policymakers and most ultimately in the lives of women and their newborns. This will stimulate more evidence-based planning and policymaking in SSA.
5 Conclusion
This study has provided vital considerations for developing a policy-ready dashboard for EmOC geographical accessibility in SSA. Insights gathered from the survey informed by two groups of stakeholders take us one step closer to the ‘utopia’ of geographical accessibility of maternal health services, where geographical information systems built on better data for better analytics will be available to support policymaking, as was imagined by researchers in this field previously [26]. Efforts now need to be placed on establishing partnerships that ensure the capture of closer-to-reality travel time, integration with existing health system data, and the development and maintenance of such policy-ready dashboards for EmOC geographical accessibility. If well implemented, the tool has all potential to contribute to critical policy decisions that will be lifesaving for mothers and their newborns.
Availability of data and materials
Data used in this study are available from the authors upon reasonable request.
Abbreviations
- EmOC:
-
Emergency Obstetric Care
- HRH:
-
Human Resource for Health
- LMIC:
-
Low- and Middle-Income Country
- OnTIME :
-
On Tackling In-transit delays for Mothers in Emergency
- SDG:
-
Sustainable Development Goal
- SSA:
-
Sub-Saharan Africa
- UHC:
-
Universal Health Coverage
References
WHO, UNICEF, UNFPA, World Bank Group, UNDP. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization. 2019;1–119.
UNICEF, WHO, World Bank, UNPD. A neglected tragedy: The global burden of stillbirths. New York: United Nations Children’s Fund. 2020;1–90.
GBD 2015 Maternal Mortality Collaborators. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1775–812.
Paxton A, Maine D, Freedman L. The evidence for emergency obstetric care. Int J Gynaecol Obstet. 2005;88:181–93.
WHO, UNFPA, UNICEF, Averting Maternal Deaths and Disabilities. Monitoring emergency obstetric care: a handbook. Geneva, Switzerland: WHO Press. 2009.
Chavane LA, Bailey P, Loquiha O, Dgedge M, Aerts M, Temmerman M. Maternal death and delays in accessing emergency obstetric care in Mozambique. BMC Pregnancy Childbirth. 2018;18(1):71.
Banke-Thomas A, Avoka CK on, Gwacham-Anisiobi U, Benova L. Influence of travel time and distance to the hospital of care on stillbirths: a retrospective facility-based cross-sectional study in Lagos, Nigeria. BMJ Glob Health. 2021;6(10):e007052.
Thaddeus S, Maine D. Too far to walk: Maternal mortality in context. Soc Sci Med. 1994;38(8):1091–110.
Banke-Thomas A, Avoka CK on, Gwacham-Anisiobi U, Omololu O, Balogun M, Wright K, et al. Travel of pregnant women in emergency situations to hospital and maternal mortality in Lagos, Nigeria: a retrospective cohort study. BMJ Glob Health. 2022 Apr 1;7(4):e008604.
Office of the United Nations High Commissioner for Human Rights. CESCR General Comment No. 14: The Right to the Highest Attainable Standard of Health (Art. 12). In: Twenty-second Session of the Committee on Economic, Social and Cultural Rights [Internet]. Geneva, Switzerland: United Nations; 2000. p. 1–21. Available from: https://www.refworld.org/pdfid/4538838d0.pdf.
United Nations. Sustainable Development Goals: 17 goals to transform our world. Sustainable Development Goals. 2016. Available from: http://www.un.org/sustainabledevelopment/sustainable-development-goals/.
Acharya S, Lin V, Dhingra N. The role of health in achieving the sustainable development goals. Bull World Health Organ. 2018;96(9):591.
Banke-Thomas A, Wright K, Collins L. Assessing geographical distribution and accessibility of emergency obstetric care in sub-Saharan Africa: a systematic review. J Glob Health. 2019;9(1):010414.
Ouma P, Macharia PM, Okiro E, Alegana V, Ouma P, Macharia PM, et al. Methods of Measuring Spatial Accessibility to Health Care in Uganda. In: Makanga PT, editor., et al., Practicing Health Geography Global Perspectives on Health Geography. Springer: Cham; 2021. p. 77–90.
Banke-Thomas A, Wong KLM, Ayomoh FI, Giwa-Ayedun RO, Benova L. “In cities, it’s not far, but it takes long”: comparing estimated and replicated travel times to reach life-saving obstetric care in Lagos. Nigeria BMJ Glob Health. 2021;6:e004318.
Ahmed S, Adams AM, Islam R, Hasan SM, Panciera R. Impact of traffic variability on geographic accessibility to 24/7 emergency healthcare for the urban poor: A GIS study in Dhaka, Bangladesh. Wilson FA, editor. PLoS One. 2019;14(9):e0222488.
Banke-Thomas A, Wong KLM, Collins L, Olaniran A, Balogun M, Wright O, et al. An assessment of geographical access and factors influencing travel time to emergency obstetric care in the urban state of Lagos. Nigeria Health Policy Plan. 2021;36(9):1384–96.
Banke-Thomas A, Macharia PM, Makanga PT, Beňová L, Wong KLM, Gwacham-Anisiobi U, et al. Leveraging big data for improving the estimation of close to reality travel time to obstetric emergency services in urban low- and middle-income settings. Front Public Health. 2022;10:931401.
Lock O, Bednarz T, Leao SZ, Pettit C. A review and reframing of participatory urban dashboards. City Cult Soc. 2020;20:100294.
Gee RE, Muncy ML. Dashboards to Support State Health Policy Making. JAMA Health Forum. 2020;1(4):e200469–e200469.
Etamesor S, Ottih C, Salihu IN, Okpani AI. Data for decision making: using a dashboard to strengthen routine immunisation in Nigeria. BMJ Glob Health. 2018;3(5):e000807.
Ihantamalala FA, Herbreteau V, Révillion C, Randriamihaja M, Commins J, Andréambeloson T, et al. Improving geographical accessibility modeling for operational use by local health actors. Int J Health Geogr. 2020;19:27.
Head MG. A real-time policy dashboard can aid global transparency in the response to coronavirus disease 2019. Int Health. 2020;12(5):373–4. Available from: https://academic.oup.com/inthealth/article/12/5/373/5869762.
Salehi M, Arashi M, Bekker A, Ferreira J, Chen DG, Esmaeili F, et al. A Synergetic R-Shiny Portal for Modeling and Tracking of COVID-19 Data. Front Public Health. 2021;27(8):1042.
Few S. Information Dashboard Design: Effective Visual Communication of Data. 1st ed. O′Reilly. 2006;34.
Matthews Z, Rawlins B, Duong J, Molla YB, Moran AC, Singh K, et al. Geospatial analysis for reproductive, maternal, newborn, child and adolescent health: gaps and opportunities. BMJ Glob Health. 2019;4(Suppl 5):e001702.
Salgado M, Nogueira P, Torres A, Oliveira MD. Setting Requirements for a Dashboard to Inform Portuguese Decision-Makers About Environment Health in an Urban Setting. Front Public Health. 2022;10:1723.
Nyapwere N, Dube YP, Makanga PT. Guidelines for developing geographically sensitive mobile health applications. Health Technol (Berl). 2021;11(2):379–87.
Dowding D, Randell R, Gardner P, Fitzpatrick G, Dykes P, Favela J, et al. Dashboards for improving patient care: Review of the literature. Int J Med Inform. 2015;84(2):87–100.
Im EO, Chee W. Quota sampling in internet research: Practical issues. CIN - Computers Informatics Nursing. 2011;29(7):381–5.
Phiri SNA, Fylkesnes K, Moland KM, Byskov J, Kiserud T. Rural-Urban Inequity in Unmet Obstetric Needs and Functionality of Emergency Obstetric Care Services in a Zambian District. PLoS ONE. 2016;11(1):e0145196.
Banke-Thomas A, Balogun M, Wright O, Ajayi B, Abejirinde IOO, Olaniran A, et al. Reaching health facilities in situations of emergency: qualitative study capturing experiences of pregnant women in Africa’s largest megacity. Reprod Health. 2020;17(1):145.
United Nations. World Urbanization Prospects: The 2018 Revision. New York: United Nations. 2019. Report No.: ST/ESA/SER.A/420). Available from: https://population.un.org/wup/Publications/Files/WUP2018-Report.pdf.
Elsey H, Agyepong I, Huque R, Quayyem Z, Baral S, Ebenso B, et al. Rethinking health systems in the context of urbanisation: challenges from four rapidly urbanising low-income and middle-income countries. BMJ Glob Health. 2019;4(3):e001501.
Cuervo LG, Martinez-Herrera E, Osorio L, Hatcher-Roberts J, Cuervo D, Bula MO, et al. Dynamic accessibility by car to tertiary care emergency services in Cali, Colombia, in 2020: cross-sectional equity analyses using travel time big data from a Google API. BMJ Open. 2022;12(9):e062178.
Banke-Thomas A, Macharia PM, Makanga PT, Beňová L, Wong KLM, Gwacham-Anisiobi U, et al. Innovative digital technology for planning emergency obstetric care in Nigeria: Qualitative study of technocrat perspectives. Health Policy Technol. 2023;In Press.
Banke-Thomas A, Madaj B, Kumar S, Ameh C, van den Broek N. Assessing Value-for-Money in Maternal and Newborn Health. BMJ Glob Health. 2017;2:e000310.
Benova L, Macleod D, Footman K, Cavallaro F, Lynch CA, Campbell OMR. Role of the private sector in childbirth care: cross-sectional survey evidence from 57 low- and middle-income countries using Demographic and Health Surveys. Tropical Med Int Health. 2015;20(12):1657–73.
Wong KL, Banke-Thomas A, Sholkamy H, Dennis ML, Pembe AB, Birabwa C, et al. A tale of 22 cities: utilisation patterns and content of maternal care in large African cities. BMJ Glob Health. 2022;7(3):e007803.
Hsia RY, Mbembati NA, MacFarlane S, Kruk ME. Access to emergency and surgical care in sub-Saharan Africa: the infrastructure gap. Health Policy Plan. 2012;27(3):234–44.
Ibeneme S, Karamagi H, Muneene D, Goswami K, Chisaka N, Okeibunor J. Strengthening Health Systems Using Innovative Digital Health Technologies in Africa. Front Digit Health. 2022;4:854339.
Alemu SM, Tura AK, do Amaral GSG, Moughalian C, Weitkamp G, Stekelenburg J, et al. How applicable is geospatial analysis in maternal and neonatal health in sub-Saharan Africa? A systematic review. J Glob Health. 2022;12:04066.
Banke-Thomas A, Abejirinde IOO, Ayomoh FI, Banke-Thomas O, Eboreime EA, Ameh CA. The cost of maternal health services in low-income and middle-income countries from a provider’s perspective: a systematic review. BMJ Glob Health. 2020;5(6):e002371.
Banke-Thomas A, Wright K, Sonoiki O, Ilozumba O, Ajayi B, Okikiolu O, et al. Multi-stakeholder perspectives on access, availability and utilization of emergency obstetric care services in Lagos, Nigeria: A mixed-methods study. J Public Health Afr. 2017;8(2):717.
Calvello EJB, Tenner AG, Broccoli MC, Skog AP, Muck AE, Tupesis JP, et al. Operationalising emergency care delivery in sub-Saharan Africa: consensus-based recommendations for healthcare facilities. Emerg Med J. 2016;33(8):573–80.
Macharia PM, Wong KLM, Olubodun T, Beňová L, Stanton C, Sundararajan N, et al. A geospatial database of close-to-reality travel times to obstetric emergency care in 15 Nigerian conurbations. Scientific Data. 2023;10(1):736.
Eboreime EA, Olawepo JO, Banke-Thomas A, Abejirinde IOO, Abimbola S. Appraising and addressing design and implementation failure in global health: A pragmatic framework. Glob Public Health. 2020;16(7):1122–30.
Acknowledgements
We appreciate colleagues at the African Centres for Disease Control and Prevention, the West African Network of Emerging Leaders in Health Policy and Systems Research, the World Health Organization’s PMNCH for Women’s Children’s and Adolescents’ Health, Google, government representatives, and colleagues on Twitter and LinkedIn who helped in circulating the study questionnaire. We are particularly grateful to the policymakers and researchers who took time out of their busy schedules to participate in the survey that informed this study.
Funding
This study was funded by the Ideas Fund (Award 14650) from the University of Greenwich.
Author information
Authors and Affiliations
Contributions
AB-T conceptualised the study. AB-T and PMM conducted the literature review that informed the study. AB-T, JW, KLMW, and PMM developed the tool for the study. All authors were involved in the recruitment of participants for the survey. AB-T, JW, KLMW, TO, UG-A, and OO were involved in the data cleaning and recoding of the data. AB-T, JW, and KLMW conducted the analysis and prepared the first draft of the manuscript. All authors were involved in the preparation of subsequent drafts. In addition, all authors approved the final version.
Corresponding author
Ethics declarations
Ethical approval and consent to paticipant
As this was research involving human participants, it was performed in accordance with the Declaration of Helsinki. Ethical approval was obtained from the University of Greenwich Research and Ethics Committee (UREC/21.4.7.8). Informed consent was obtained from all participants before recruitment.
Consent for publication
Not applicable.
Competing interest
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, J., Wong, K.L.M., Olubodun, T. et al. Developing policy-ready digital dashboards of geospatial access to emergency obstetric care: a survey of policymakers and researchers in sub-Saharan Africa. Health Technol. 14, 69–80 (2024). https://doi.org/10.1007/s12553-023-00793-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-023-00793-9