Abstract
Background
Smart-bar device (SBD) is a newly developed device to measure the body range of motion (ROM) by a kinetic sensor and to provide an exercise program with augmented reality (AR) guidance of body-frame image and audio feedback by mobile application.
Objective
This study aims to compare the performance of SBD with AR function with a goniometer and to verify the clinical utility of SBD with AR guide function`
Methods
Ten healthy individuals were enrolled and measured the ROM of body lateral flexion, extension, and rotation using a goniometer and SBD simultaneously. To evaluate the accuracy of an AR-guided exercise, we enrolled three patients with adolescent idiopathic scoliosis and measured the ROM of trunk lateral flexion and rotation during stretching exercises using SBD with or without AR guidance.
Results
Concurrent validity between the goniometer and SBD was statistically significant, with a very high correlation coefficient from r = 0.836–0.988 (p < 0.05). All patients with scoliosis showed higher accuracy when we used SBD with AR guidance than when we used SBD without AR guidance (p < 0.05).
Conclusions
The SBD could be a valid device to measure the joint angle of neck, shoulder, and trunk. AR guidance increased the accuracy of the stretching exercise, and mobile application of AR-guided stretching exercises with SBD should be useful for scoliosis patients to correct their posture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Spinal deformities have been cited in numerous studies, and range from 0.4 in 1000 for idiopathic scoliosis [1] to 2.5 in 1000 for adolescent idiopathic scoliosis [2]. Recent studies indicate that posture during use of tablets and smartphones increase the load on the neck and trunk in adolescents [3]. A multiple logistic regression model revealed that those with smartphone overuse were approximately six times more likely to have neck pain (95% CI 4.44–8.09, p < 0.001) [4]. Smartphone overuse significantly increases the chance of musculoskeletal pain by six times [4]. The prolonged time in keeping the body in a poor posture will induce paravertebral muscle pain, unbalanced force application to the vertebral bone, and even worse, permanent spinal malformation, including scoliosis [5]. To prevent developmental spine problems in adolescence, many educators promoted the physical activity in schools and developed guidelines for restricting hours of smart phone usage [6, 7]. To treat and prevent these posture problems, the lengthened muscles should be shortened, and the shortened muscles should be lengthened again, to restore the spine’s vertical axis [8]. Self-stretching exercises decreased muscle spasms on the concave side and hyperactivity, and corrected the curvature of the lumbar region by lengthening the shortened muscles [9]. Stretching exercises can improve the yield of sports practices in the young [10,11,12], besides reducing work-related musculoskeletal pain in adults [13]. Self-stretching interventions can reduce the burden of upper extremity musculoskeletal disorders depending on their training, knowledge, and experiences. Self-stretching at home, the patient does not have the inconvenience and cost of logistics from home to the clinic and can carry out rehabilitation activities in the comfort of his/her home, being likely to show a motivation to progress and follow the treatment [14].
Nowadays, augmented reality (AR) technology, in particular, is widely used in the rehabilitation, because three factors (repetition, rapid feedback, and motivation) conveyed through AR have been found to be very effective [15].
Another method for stretching is one-to-one personal training. In a 24-week study that consisted of weekly exercise sessions, a control group with minimal supervision vs. those assigned a personal trainer had better adherence (84% vs. 69%) [16]. In the clinical environments, the instructions to help patients do these specific movements correctly are given by the therapist. Without any guidance, the patients may do the stretching exercise with compensation, and the alignment may go in the wrong direction if they shake their limbs. It is most important to maintain the correct position and movement during the stretching exercise.
AR is a technology that combines the real world and 3D virtual-object digital content with additional information into a single image in real time [17]. AR solutions have been used for motor rehabilitation and allow the patients to receive information in real time while performing their activities or exercises [18, 19]. However, there is still insufficient data about whether AR information actually contributes to maintaining an accurate posture during stretching exercises. Although the literature on the effects of stretching exercises presents many differences in its prescriptions, absence of a control group, and randomized trials [20,21,22,23,24,25], but few studies have investigated this topic to guide rehabilitation exercises where movement correctness can affect the therapeutic effectiveness [14].
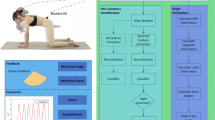
Recently, the smart-bar device (SBD) is a newly developed hand-held device that could measure body movement by a kinetic sensor and provide the mobile exercise program with AR guidance of the body-image frame and audio feedback (Fig. 1). We developed the stretching-exercise program for adolescent idiopathic scoliosis using the SBD and mobile application. Thus, we tested the concurrent validity of joint-angle measurement by SBD by comparing it with a goniometer and evaluated the accuracy of AR-guided stretching exercises by using SBD and mobile application for clinical usefulness.
2 Methods
Patients hold the SBD in both hands and do exercises with the guidance of a mobile application, which should be the same exercise as with the guidance of a physician. The SBD equipment measures movement posture using a nine-axis sensor (MPU-9250, InvenSense Inc.) and communicates the movement situation to the user via an LED indicator and vibration element. The equipment weighs 60 g and has dimensions of 25 mm × 150 mm × 25 mm (width, height, and length). After noise is removed, the data collected by the SBD is analyzed to measure the three-dimensional angle of physical performance using Roll, Pitch, and Yaw (Fig. 2). During exercise, the device's kinetic sensor tracks the body's range of motion (ROM), while the mobile application measures the body angle using a formula.
At the same time, the mobile application provides the AR guidance of body-image frames for correct exercises, and the audio feedback makes the body maintain the correct position.The study of concurrent validity was approved by Dongguk University Ilsan Hospital’s Institutional Review Board (IRB No. DUIH 2019-09-009), who also approved the study of clinical usefulness (IRB No. DUIH 2020-09-001-002), which was registered at Clinical Research Information Service (CRIS; Registration No.: KCT0004440). Informed consent was obtained from all individual participants included in the study.
2.1 Validity Test
2.1.1 Subjects
For the concurrent validity test, we enrolled ten healthy adults who had no Musculoskeletal problems and measured the body range of motion (ROM) in neck lateral flexion and extension, trunk lateral flexion and rotation, and shoulder horizontal flexion. The angle of horizontal flexion was measured after 90°. Their demographic characteristics are the mean age of 32.00 ± 7.00, the mean height of 166.30 ± 10.80, and the mean weight of 61.70 ± 13.22 (Table 1).
2.1.2 Measurements
We selected these body ROM because they are used movements for developed stretching exercise in this study. The angles during these ROM were measured by a physiotherapist who used a conventional method for a goniometer [26] and collected the data of SBD simultaneously 5 times.
2.2 Clinical Usefulness Test
2.2.1 Subjects
To evaluate the clinical usefulness of SBD with AR guidance (SBD-AR), three adolescent idiopathic scoliosis patients participated in this study. They had been diagnosed radiologically and did not have fixed spinal deformity or previous surgical correction of the spine. They could do stretching exercise for 30 min without any pain. Their characteristics are the mean age of 14.33 ± 0.577, the mean height of 169.60 ± 7.50, the mean weight of 56.13 ± 8.62 (Table 4). All patients have the right thoracic curve and the mean of cobb angle is 14 ± 10 (Table 4).
2.2.2 Intervention
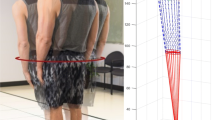
Subjects performed two types of stretching exercise: trunk lateral flexion and trunk rotation. They are developed by the human anatomical structure and generally accepted stretching exercise in the clinic. Trunk lateral flexion is the position of grasp each end of the SBD with elbow extension and raise the arm to overhead and trunk flexion laterally. Trunk rotation is the position of grasp each end of the SBD with elbow extension and rotate the arm on transverse plane with horizontal adduction of one shoulder and horizontal adduction of the other shoulder. Each exercise consisted of a 2-s movement phase from the starting position to the ending position, and a 13-s stop phase at the ending position. Before the intervention, Subjects are provided the education of two types of stretching exercises and how to use the SBD for 10 min. After that, Subjects pick a paper with SBD or SBD-AR written on it and determine the order randomly.
The intervention used SBD alone and SBD-AR. The intervention of SBD alone was done while the subject watched the mobile application showing real time image of himself or herself without any AR guide He or she could check the exercise time of the 2-s movement and the 13-s stop phase by the mobile application. The intervention of SBD-AR was also done while the patient watched the mobile application showing himself or herself in the AR image in the mobile application (Smart Medical Device Co., Ltd., South Korea), which was the exercise guidance that provided the pre-programmed precise exercise around their real body image (Fig. 1).
2.2.3 Measurements
The SBD measured and stored the angle of trunk lateral flexion and rotation every 0.1 s. Each value of every 0.1 s minus the average value of whole stop phase indicate the value of shaking every 0.1 s. The average value of this shaking value of each 0.1 s during the stop phase is defined as "deviation angle" in this study. The greater the deviation angle was, the less accurate was the exercise. To evaluate the accuracy of the exercise, we measured the deviation angle of the actual exercise from the AR guidance and compared the mean values between SBD and SBD-AR.
The maximum tilting angle is the average accumulated values for every 0.3 s by SBD during the exercise and the stop phase. The tilting angles were in two opposite directions: the front and rear directions during trunk lateral flexion, the up and down directions during trunk rotation. The greater the tilting angle was, the wider the tremor was.
2.3 Statistics
The mean angles of ROM measured by both a goniometer and an SBD were compared using the t-test. All values are presented as mean ± standard deviation (mean ± SD). We analyzed the relationships between the ROM of the goniometer and SBD by using Pearson’s correlations. We assessed the significance of accuracy between SBD and SBD-AR by paired t-tests, and did all statistical analyses using SPSS Ver.22 (IBM Corporation, US), setting the statistical significance level at p < 0.05.
3 Results
3.1 The Validity Test
Ten healthy persons participated. The angles of neck lateral flexion and rotation, shoulder horizontal flexion, and trunk later flexion and rotation were not significantly different between the values from the goniometer and SBD (Table 2). The relationships between the values by goniometer and SBD for all angles showed statistical significance, with very high correlation coefficients from r = 0.836–0.988 (Table 3).
3.2 The Clinical Usefulness Test
Three scoliosis patients participated (Table 4). In the comparison of mean deviation angles between SBD and SBD-AR, the deviation angle of trunk lateral flexion and rotation was reduced significantly in SBD-AR (Table 5). All patients showed higher accuracy during the trunk lateral flexion and rotation exercise in SBD-AR than in SBD (Fig. 3). The tilting angle of both directions also reduced significantly in SBD-AR. All patients showed less tremor during the stop phase in SBD-AR than in SBD (Table 6).
4 Discussion
Spinal deformities related to poor postures have affected postural imbalance and unequal loads in the trunk muscles [27]. Postural asymmetry and muscle imbalance could be improved by physical exercises based on stretching exercises [28]. However, the lack of posture feedback of the exercise can lead adverse effect and many recent works have addressed this problem [29,30,31]. Actually. there are many technologies and system were developed in various field of pose estimation [32] and motion prediction [33, 34] and they can provide real time feedback of physical exercises. Actually, a few recent studies represent the advantage and effectiveness of home-based exercise program with an AR system in various filed of patients with stroke [35] and elderly [36]. In the result of one RCT trial indicated that AR-based telerehabilitation is more effective than a brochure-based home exercise program [37].
The SBD is a newly developed that could measure body movement and provide the mobile exercise program with AR guidance of the body-image frame and audio feedback. We conduct the clinical test to evaluate whether the AR-based guidance can increase the accuracy of the posture during the stretching exercise. This concurrent validity test provides evidence that the SBD can be a valid tool for measuring neck, shoulder, and trunk ROM in healthy individuals. In the validity test, we confirmed the concurrent validity and clinical usefulness of SBD to measure the range of motion. Thus, we conducted the clinical usefulness test of SBD to evaluate the AR-based guidance, which could increase the accuracy of the posture during the stretching exercise.
The validity test showed that the SBD could be a valid device for a physiotherapist to measure the joint angle by using a goniometer in a conventional method of ROM measurement. To evaluate the clinical usefulness of SBD-AR, three adolescent idiopathic scoliosis patients underwent the intervention with SBD and SBD-AR. To analyze the effectiveness of the AR-based guidance on accuracy and maintain the posture during stretching exercise, we provide a new concept of predictor as "deviation angle" and it can indicate the accuracy of the stretching exercise. The SBD measured red and stored the angle of trunk lateral flexion and rotation every 0.1 s. Each value of every 0.1 s minus the average value of whole stop phase indicate the value of shaking every 0.1 s. The average value of this shaking value of each 0.1 s during the stop phase is defined as "deviation angle" in this study. The greater the deviation angle was, the less accurate was the exercise. To evaluate the accuracy of the exercise, we measured the deviation angle of the actual stretching exercise and compared between SBD and SBD-AR. There was higher accuracy during the stretching exercise in SBD-AR than in SBD. The AR image in the mobile application was the exercise guidance that provided the pre-programmed precise exercise around their real body image. It also provided the audio feedback to correct the posture when the real-time body image deviated significantly from the AR image. During the stretching exercise, the patients tried to correct their movement by means of the AR guidance and audio feedback warning about the deviant movement out of image. In order to analyze the movements performed by the patient and to provide feedback for guidance and correction, the AR solution needs to track the body segment executing the movement, can provide the visibility needed for user interaction [38], and contributes to early learning, helping the beginner understand the movement [39]. Using multimodal feedback information in rehabilitation solutions helps users to do the correct movement [39, 40]. Newly developed SBD-AR guidance increased the accuracy of the exercise and should be useful for scoliosis patients to correct their posture. The clinical usefulness test had a small sample size from one hospital. We could not control the potential bias in the order of intervention of SBD and SBDAR. Although we randomly determined the order of intervention, one subject performed the SBDAR first, and two of them performed SBD first. Because two interventions of SBD and SBDAR were performed within a day despite the resting time, variables such as exercise adaptation and abdominal muscle preparation can be affected in the second stretching exercise. These biases need to be considered in the next studies with a sufficient number of subjects. In addition, we need to follow the effect of SBD and SBD AR over a long-term period. Because adolescent scoliosis would improve by exercise effectively, we could confirm the effect of SBDAR with the improvement of Cobb's angle.
Abbreviations
- AR:
-
Augmented reality
- SBD:
-
Smart bar device
References
Akbarnia, B. A. (2007). Management themes in early onset scoliosis. JBJS, 89(suppl_1), 42–54.
Morais, T., Bernier, M., & Turcotte, F. (1985). Age-and sex-specific prevalence of scoliosis and the value of school screening programs. American Journal of Public Health, 75(12), 1377–1380.
Eitivipart, A. C., Viriyarojanakul, S., & Redhead, L. (2018). Musculoskeletal disorder and pain associated with smartphone use: A systematic review of biomechanical evidence. Hong Kong Physiotherapy Journal, 38(02), 77–90.
Derakhshanrad, N., Yekaninejad, M. S., Mehrdad, R., & Saberi, H. (2021). Neck pain associated with smartphone overuse: Cross-sectional report of a cohort study among office workers. European Spine Journal, 30, 461–467.
Hanphitakphong, P., Thawinchai, N., & Poomsalood, S. (2021). Effect of prolonged continuous smartphone gaming on upper body postures and fatigue of the neck muscles in school students aged between 10–18 years. Cogent Engineering, 8(1), 1890368.
Rather, M., & Rather, S. (2019). Impact of smartphones on young generation. Library Philosophy and Practice, 1–9.
Guddal, M. H., Stensland, S. Ø., Småstuen, M. C., Johnsen, M. B., Zwart, J., & Storheim, K. (2017). Physical activity level and sport participation in relation to musculoskeletal pain in a population-based study of adolescents: The young-HUNT study. Orthopaedic Journal of Sports Medicine, 5(1), 2325967116685543.
Yang, J., Lee, J., & Lee, D. (2015). Effects of consecutive application of stretching, Schroth, and strengthening exercises on Cobb’s angle and the rib hump in an adult with idiopathic scoliosis. Journal of Physical Therapy Science, 27(8), 2667–2669.
Zakaria, A., Hafez, A. R., Buragadda, S., & Melam, G. R. (2012). Stretching versus mechanical traction of the spine in treatment of idiopathic scoliosis. Journal of Physical Therapy Science, 24(11), 1127–1131.
Shrier, I. (2004). Does stretching improve performance?: A systematic and critical review of the literature. Clinical Journal of Sport Medicine, 14(5), 267–273.
Kokkonen, J., Nelson, A. G., Eldredge, C., & Winchester, J. B. (2007). Chronic static stretching improves exercise performance. Medicine & Science in Sports & Exercise, 39(10), 1825–1831.
Ferreira, G. N. T., Teixeira-Salmela, L. F., & Guimarães, C. Q. (2007). Gains in flexibility related to measures of muscular performance: Impact of flexibility on muscular performance. Clinical Journal of Sport Medicine, 17(4), 276–281.
Marangoni, A. H. (2010). Effects of intermittent stretching exercises at work on musculoskeletal pain associated with the use of a personal computer and the influence of media on outcomes. Work, 36(1), 27–37.
Da Gama, A. E. F., Chaves, T. M., Figueiredo, L. S., Baltar, A., Meng, M., Navab, N., Teichrieb, V., & Fallavollita, P. (2016). MirrARbilitation: A clinically-related gesture recognition interactive tool for an AR rehabilitation system. Computer Methods and Programs in Biomedicine, 135, 105–114.
Holden, M. K. (2005). Virtual environments for motor rehabilitation. Cyberpsychology & Behavior, 8(3), 187–211.
Mazzetti, S. A., Kraemer, W. J., Volek, J. S., Duncan, N. D., Ratamess, N. A., Gomez, A. L., Newton, R. U., Hakkinen, K., & Fleck, S. J. (2000). The influence of direct supervision of resistance training on strength performance. Medicine and Science in Sports and Exercise, 32(6), 1175–1184.
Van Krevelen, D., & Poelman, R. (2010). A survey of augmented reality technologies, applications and limitations. International Journal of Virtual Reality, 9(2), 1–20.
Regenbrecht, H., Hoermann, S., Ott, C., Mueller, L., & Franz, E. (2014). Manipulating the experience of reality for rehabilitation applications. Proceedings of the IEEE, 102(2), 170–184.
Sousa, M., Vieira, J., Medeiros, D., Arsenio, A., & Jorge, J. (2016). SleeveAR: Augmented reality for rehabilitation using realtime feedback. In Paper presented at the Proceedings of the 21st international conference on intelligent user interfaces (pp. 175–185).
Feland, J. B., Myrer, J. W., Schulthies, S. S., Fellingham, G. W., & Measom, G. W. (2001). The effect of duration of stretching of the hamstring muscle group for increasing range of motion in people aged 65 years or older. Physical Therapy, 81(5), 1110–1117.
Gajdosik, R. L., Vander Linden, D. W., McNair, P. J., Williams, A. K., & Riggin, T. J. (2005). Effects of an eight-week stretching program on the passive-elastic properties and function of the calf muscles of older women. Clinical Biomechanics, 20(9), 973–983.
Cristopoliski, F., Barela, J. A., Leite, N., Fowler, N. E., & Rodacki, A. L. F. (2009). Stretching exercise program improves gait in the elderly. Gerontology, 55(6), 614–620.
Bird, M., Hill, K., Ball, M., & Williams, A. D. (2009). Effects of resistance-and flexibility-exercise interventions on balance and related measures in older adults. Journal of Aging and Physical Activity, 17(4), 444–454.
Batista, L. H., Vilar, A. C., de Almeida Ferreira, J. J., Rebelatto, J. R., & Salvini, T. F. (2009). Active stretching improves flexibility, joint torque, and functional mobility in older women. American Journal of Physical Medicine & Rehabilitation, 88(10), 815–822.
Gallon, D., Rodacki, A., Hernandez, S. G., Drabovski, B., Outi, T., Bittencourt, L. R., & Gomes, A. (2011). The effects of stretching on the flexibility, muscle performance and functionality of institutionalized older women. Brazilian Journal of Medical and Biological Research, 44, 229–235.
Physiopedia contributors. (2021). Goniometer. Physiopedia. Retrieved from https://www.physio-pedia.com/index.php?title=Goniometer&oldid=266690
Jung, J., Heo, M., & Kim, J. (2020). Effects of a personalized exercise rehabilitation device on dynamic postural balance for scoliotic patients: A feasibility study. Electronics, 9(12), 2100.
Smidt, N., de Vet, H. C., Bouter, L. M., & Dekker, J. (2005). Effectiveness of exercise therapy: A best-evidence summary of systematic reviews. Australian Journal of Physiotherapy, 51(2), 71–85.
Kanase, R. R., Kumavat, A. N., Sinalkar, R. D., & Somani, S. (2021). Pose estimation and correcting exercise posture. Paper presented at the ITM Web of Conferences, 40, 03031.
Fieraru, M., Zanfir, M., Pirlea, S. C., Olaru, V., & Sminchisescu, C. (2021). Aifit: Automatic 3d human-interpretable feedback models for fitness training. In Paper presented at the Proceedings of the IEEE/CVF conference on computer vision and pattern recognition (pp. 9919–9928).
Rangari, T., Kumar, S., Roy, P. P., Dogra, D. P., & Kim, B. (2022). Video based exercise recognition and correct pose detection. Multimedia Tools and Applications, 81(21), 30267–30282.
Gong, K., Li, B., Zhang, J., Wang, T., Huang, J., Mi, M. B., Feng, J., & Wang, X. (2022). PoseTriplet: co-evolving 3D human pose estimation, imitation, and hallucination under self-supervision. In Paper presented at the Proceedings of the IEEE/CVF conference on computer vision and pattern recognition (pp. 11017–11027).
Mao, W., Liu, M., & Salzmann, M. (2020). History repeats itself: Human motion prediction via motion attention. In Paper presented at the Computer Vision–ECCV 2020: 16th European Conference, Glasgow, UK, August 23–28, 2020, Proceedings, Part XIV 16 (pp. 474–489).
Kiciroglu, S., Wang, W., Salzmann, M., & Fua, P. (2020). Long term motion prediction using keyposes. Preprint https://arxiv.org/abs/2012.04731
Lee, J. I., Park, J., Koo, J., Son, M., Hwang, J. H., Lee, J. Y., & Chang, W. H. (2022). Effects of the home-based exercise program with an augmented reality system on balance in patients with stroke: A randomized controlled trial. Disability and Rehabilitation, 1–8.
Jeon, S., & Kim, J. (2020). Effects of augmented-reality-based exercise on muscle parameters, physical performance, and exercise self-efficacy for older adults. International Journal of Environmental Research and Public Health, 17(9), 3260.
Yeo, S. M., Lim, J. Y., Do, J. G., Lim, J., In Lee, J., & Hwang, J. H. (2021). Effectiveness of interactive augmented reality-based telerehabilitation in patients with adhesive capsulitis: Protocol for a multi-center randomized controlled trial. BMC Musculoskeletal Disorders, 22, 1–9.
Preece, J., Sharp, H., & Rogers, Y. (2015). Interaction design: Beyond human-computer interaction. Wiley.
Sigrist, R., Rauter, G., Riener, R., & Wolf, P. (2013). Augmented visual, auditory, haptic, and multimodal feedback in motor learning: A review. Psychonomic Bulletin & Review, 20, 21–53.
Cooper, R. A., Ohnabe, H., & Hobson, D. A. (2006). An introduction to rehabilitation engineering. CRC Press.
Acknowledgements
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. 2017M3A9F1032546).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by YGN and SYP. BSK made substantial contributions to the experimental design and drafting of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that there is no conflict of interest regarding the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nam, YG., Park, S.Y. & Kwon, B.S. Rehabilitation Exercise Using a Smart-Bar Device with Augmented Reality Guide Function. Int. J. Precis. Eng. Manuf. 24, 1263–1270 (2023). https://doi.org/10.1007/s12541-023-00815-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12541-023-00815-6