Abstract
Background
Preterm infants with long-term parenteral nutrition (PN) therapy are at risk for cholestasis associated with total parenteral nutrition (PNAC). This study examined the safety and efficacy of ursodeoxycholic acid (UDCA) in preventing PNAC in preterm infants. Our research aimed to investigate the prophylactic effect of preventive oral UDCA on PNAC in preterm infants.
Methods
We compared oral administration of UDCA prophylaxis with no prophylaxis in a randomized, open-label, proof-of-concept trial in preterm neonates with PN therapy. The low-birth-weight preterm infants (< 1800 g) who were registered to the neonatal intensive care unit (NICU) within 24 hours after birth were randomized. The main endpoint was the weekly values of direct bilirubin (DB) of neonates during the NICU stay.
Results
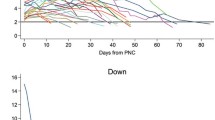
Eventually, a total of 102 preterm neonates from January 2021 to July 2021 were enrolled in this prospective study (42 in the UDCA group and 60 in the control group). Notably, the peak serum level of DB [13.0 (12–16) vs. 15.2 (12.5–19.6) μmol/L, P < 0.05)] was significantly lower in the UDCA group than that in the control group without prevention. The peak serum level of total bilirubin (101.1 ± 34 vs. 116.5 ± 28.7 μmol/L, P < 0.05) was also significantly lower in the UDCA group than in the control group. Furthermore, the proportion of patients who suffered from neonatal cholestasis (0.0% vs. 11.7%, P < 0.05) in the UDCA group was significantly lower.
Conclusion
UDCA prophylaxis is beneficial in preventing PNAC in NICU infants receiving prolonged PN.


Similar content being viewed by others
Data availability
The datasets generated and analyzed during this study are available from the corresponding author on reasonable request.
References
Sandeva M, Uchikov P. Analysis of pathology in premature infants in obstetrics and gynecology clinic at St George University Hospital, Plovdiv between 2013 and 2015. Folia Med (Plovdiv). 2021;63:88–96.
Schutzman DL, Porat R, Salvador A, Janeczko M. Neonatal nutrition: a brief review. World J Pediatr. 2008;2008:6.
Patel P, Bhatia J. Total parenteral nutrition for the very low birth weight infant. Semin Fetal Neonatal Med. 2017;22:2–7.
Barr PA, Mally PV, Caprio MC. Standardized nutrition protocol for very low-birth-weight infants resulted in less use of parenteral nutrition and associated complications, better growth, and lower rates of necrotizing enterocolitis. JPEN J Parenter Enteral Nutr. 2019;43:540–9.
Lee HH, Jung JM, Nam SH, Lim G, Chung ML. Risk factor analysis of parenteral nutrition-associated cholestasis in extremely low birth weight infants. Acta Paediatr. 2016;105:e313–9.
Lapillonne A, Kermorvant-Duchemin E. A systematic review of practice surveys on parenteral nutrition for preterm infants. J Nutr. 2013;143:2061S-S2065.
Nakajima H, Koga H, Okawada M, Nakamura H, Lane GJ, Yamataka A. Does time taken to achieve jaundice-clearance influence survival of the native liver in post-Kasai biliary atresia? World J Pediatrics. 2018;14:191–6.
Sultana H, Komai M, Shirakawa H. The role of vitamin K in cholestatic liver disease. Nutrients. 2021;2021:13.
Lapillonne A, Berleur MP, Brasseur Y, Calvez S. Safety of parenteral nutrition in newborns: results from a nationwide prospective cohort study. Clin Nutr. 2018;37:624–9.
He JP, Hao Y, Wang XL, Yang XJ, Shao JF, Feng JX. Comparison of different noninvasive diagnostic methods for biliary atresia: a meta-analysis. World J Pediatr. 2016;12:35–43.
Madnawat H, Welu AL, Gilbert EJ, Taylor DB, Jain S, Manithody C, et al. Mechanisms of parenteral nutrition-associated liver and gut injury. Nutr Clin Pract. 2020;35:63–71.
Jackson RL, White PZ, Zalla J. SMOFlipid vs intralipid 20%: effect of mixed-oil vs soybean-oil emulsion on parenteral nutrition-associated cholestasis in the neonatal population. JPEN J Parenter Enteral Nutr. 2021;45:339–46.
Montealegre-Pomar ADP, Bertolotto-Cepeda AM, Romero-Marquez Y, Munoz-Ramirez KJ. Effectiveness and safety of fast enteral advancement in preterm infants between 1000 and 2000 g of birth weight. JPEN J Parenter Enteral Nutr. 2021;45:578–86.
Abdalla AF, Fathy A, Zalata KR, Megahed A, Abo-Alyazeed A, El Regal ME. Morphometric assessment of liver fibrosis may enhance early diagnosis of biliary atresia. World J Pediatr. 2013;9:330–5.
Bischoff SC, Bernal W, Dasarathy S, Merli M, Plank LD, Schutz T, et al. ESPEN practical guideline: clinical nutrition in liver disease. Clin Nutr. 2020;39:3533–62.
Orso G, Mandato C, Veropalumbo C, Cecchi N, Garzi A, Vajro P. Pediatric parenteral nutrition-associated liver disease and cholestasis: novel advances in pathomechanisms-based prevention and treatment. Dig Liver Dis. 2016;48:215–22.
Arie L, Maayan A, Shamir R, Dinari G, Sulkes J, Sirotta L. Parenteral nutrition-associated cholestasis in preterm neonates: evaluation of ursodeoxycholic acid treatment. J Pediatric Endocrinol Metabol. 1999;12:549–53.
Niccum M, Khan MN, Middleton JP, Vergales BD, Syed S. Cholestasis affects enteral tolerance and prospective weight gain in the NICU. Clin Nutr ESPEN. 2019;30:119–25.
Cabrera D, Arab JP, Arrese M. UDCA, NorUDCA, and TUDCA in liver diseases: a review of their mechanisms of action and clinical applications. Handb Exp Pharmacol. 2019;256:237–64.
Simic D, Milojevic I, Bogicevic D, Milenovic M, Radlovic V, Draskovic B, et al. Preventive effect of ursodeoxycholic acid on parenteral nutrition-associated liver disease in infants. Srp Arh Celok Lek. 2014;142:184–8.
Guarino A, Ashkenazi S, Gendrel D, Lo Vecchio A, Shamir R, Szajewska H, et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: update 2014. J Pediatr Gastroenterol Nutr. 2014;59:132–52.
Lewis T, Kuye S, Sherman A. Ursodeoxycholic acid versus phenobarbital for cholestasis in the Neonatal Intensive Care Unit. BMC Pediatr. 2018;18:197.
Levit OL, Calkins KL, Gibson LC, Kelley-Quon L, Robinson DT, Elashoff DA, et al. Low-dose intravenous soybean oil emulsion for prevention of cholestasis in preterm neonates. JPEN J Parenter Enteral Nutr. 2016;40:374–82.
De Marco G, Sordino D, Bruzzese E, Di Caro S, Mambretti D, Tramontano A, et al. Early treatment with ursodeoxycholic acid for cholestasis in children on parenteral nutrition because of primary intestinal failure. Aliment Pharmacol Ther. 2006;24:387–94.
Llorente-Pelayo S, Docio P, Lavin-Gomez BA, Garcia-Unzueta MT, de Las CI, de la Rubia L, et al. Modified serum ALP values and timing of apparition of knee epiphyseal ossification centers in preterm infants with cholestasis and risk of concomitant metabolic bone disease of prematurity. Nutrients. 2020;2020:12.
Fernando SM, Rochwerg B, Seely AJE. Clinical implications of the third international consensus definitions for sepsis and septic shock (sepsis-3). CMAJ. 2018;190:E1058–9.
Jones IH, Hall NJ. Contemporary outcomes for infants with necrotizing enterocolitis—a systematic review. J Pediatr. 2020;220:86-92e3.
Hollebrandse NL, Spittle AJ, Burnett AC, Anderson PJ, Roberts G, Doyle LW, et al. School-age outcomes following intraventricular haemorrhage in infants born extremely preterm. Arch Dis Child Fetal Neonatal Ed. 2021;106:4–8.
Stramara L, Hernandez L, Bloom BT, Durham C. Development of parenteral nutrition-associated liver disease and other adverse effects in neonates receiving SMOFlipid or intralipid. JPEN J Parenter Enteral Nutr. 2020;44:1530–4.
Israelite JC. Pediatric parenteral nutrition-associated liver disease. J Infus Nurs. 2017;40:51–4.
Heubi JE, Wiechmann DA, Creutzinger V, Setchell KD, Squires R Jr, Couser R, et al. Tauroursodeoxycholic acid (TUDCA) in the prevention of total parenteral nutrition-associated liver disease. J Pediatr. 2002;141:237–42.
Mouillot T, Beylot M, Drai J, Hillon P, Gelas P, Lauverjat M, et al. Effect of bile acid supplementation on endogenous lipid synthesis in patients with short bowel syndrome: a pilot study. Clin Nutr. 2020;39:928–34.
Lindor KD, Kowdley KV, Luketic VA, Harrison ME, McCashland T, Befeler AS, et al. High-dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis. Hepatology. 2009;50:808–14.
Mandato C, Di Nuzzi A, Vajro P. Nutrition and liver disease. Nutrients. 2017;2017:10.
Feldman AG, Sokol RJ. Neonatal cholestasis: emerging molecular diagnostics and potential novel therapeutics. Nat Rev Gastroenterol Hepatol. 2019;16:346–60.
Zhang Y, Jiang R, Zheng X, Lei S, Huang F, Xie G, et al. Ursodeoxycholic acid accelerates bile acid enterohepatic circulation. Br J Pharmacol. 2019;176:2848–63.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SL: conceptualization, data curation, writing—original draft, writing—review and editing, and software. WL: conceptualization, writing—review and editing, and supervision. LC and JW: investigation and project administration. LC and MX: software and supervision and validation. All authors have drafted the article or revised it critically for important intellectual content. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were conducted according to the guidelines of the 1994 Declaration of Helsinki, and approved by the Ethics Committee of Tongji Hospital (TJ-IRB20210828).
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Informed consent
Informed consents have been obtained from all individual participant’s parent or legal guardian included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, SY., Chang, LW., Wang, J. et al. Ursodeoxycholic acid prevention on cholestasis associated with total parenteral nutrition in preterm infants: a randomized trial. World J Pediatr 18, 100–108 (2022). https://doi.org/10.1007/s12519-021-00487-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-021-00487-0