Abstract
Background
The size of congenital pulmonary malformation (CPM) in infants might interfere with the feasibility of thoracoscopic resection. This study was undertaken to evaluate the impact of the size of CPM on the applicability of video-assisted thoracic surgery (VATS) in infants.
Methods
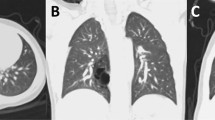
Twenty-two infants were operated on for CPM from November 2000 to June 2009. The intra- and postoperative course was analyzed retrospectively from patient charts. Preoperative scans were evaluated blindly by a radiologist to calculate the relation between the maximum size of the lesion and the thoracic diameter in VATS and open procedures.
Results
VATS was performed in 14 (64%) of the 22 patients and thoracotomy in 8. VATS was successfully performed in 11 (79%) of the 14 patients, whereas VATS was converted to thoracotomy due to lack of overview in 3 (21%). The mean relative size of CPM at preoperative imaging was 0.34 ± 0.05 (range: 0.3–0.4) in patients who received successful VATS, 0.57 ± 0.06 (range: 0.5–0.6) in converted cases, and 0.68 ± 0.10 (range: 0.5‥8) in infants who underwent thoracotomy. The relative CPM size was significantly lower in successful VATS than in cases of conversion (P<0.01) and thoracotomy (P<0.01).
Conclusions
The relative size of CPM at preoperative imaging might be useful information for a decision-making on the use of VATS in infants. A relative CPM size below 0.5, which is less than half of the thoracic diameter, indicates a good feasibility for thoracoscopic resection of CPM. A larger size may indicate that VATS might be technically difficult.
Similar content being viewed by others
References
Solaini L, Prusciano F, Bagioni P, Di Francesco F, Basilio Poddie D. Video-assisted thoracic surgery major pulmonary resections. Present experience. Eur J Cardiothorac Surg 2001;20:437–442.
Kalfa N, Allal H, Raux O, Lardy H, Varlet F, Reinberg O, et al. Multicentric assessment of the safety of neonatal surgery. Surg Endosc 2007;21:303–308.
Rothenberg S. First decade’s experience with thoracoscopic lobectomy in infants and children. J Pediatr Surg 2008;43:40–44.
Koontz CS, Oliva V, Gow KW, Wulkan ML. Video-assisted thoracoscopic surgical excision of cystic lung disease in children. J Pediatr Surg 2005;40:835–837.
Ure BM, Schmidt AI, Jesch NK. Thoracoscopic surgery in infants and children. Eur J Pediatr Surg 2005;15:314–318.
Sundarabajan L, Parikh DH. Evolving experience with video-assisted thoracic surgery in congenital cystic lung lesion in a British pediatric center. J Pediatr Surg 2007;42:1243–1250.
Stocker JT, Madewell JE, Drake RM. Congenital cystic adenamotoid malformation of the lung. Hum Pathol 1977;8:155–171.
Glüer S, Schwerk N, Reismann M, Metzelder ML, Nustede R, Ure BM, et al. Thoracoscopic biopsy in children with parenchymal lung disease. Pediatr Pulmonol 2008;43:992–996.
Metzelder ML, Kuebler JF, Reismann M, Lawal TA, Glueer S, Ure B. Prior thoracic surgery has a limited impact on the feasibility of consecutive thoracoscopy in children: a prospective study of 228 procedures. J Laparoendosc Adv Surg Tech A 2009;19(s1):s63–s66.
Glüer S, Reismann M, Ure BM. Congenital lobar emphysema. Ann Thorac Surg 2008;85:665.
Jesch NK, Leonhardt J, Sumpelmann R, Glüer S, Nustede R, Ure BM. Thoracoscopic resection of intra- and extralobar pulmonary sequestration in the first 3 months of life. J Pediatr Surg 2005;40:1404–1406.
Albanese CT, Rothenberg SS. Experience with 144 consecutive pediatric thoracoscopic lobectomies. J Laparoendosc Adv Surg Tech 2007;17:339–341.
Lawal TA, Gosemann JH, Kuebler JF, Glüer S, Ure BM. Thoracoscopy versus thoracotomy improves midterm musculoskeletal status and cosmesis in infants and children. Ann Thorac Surg 2009;87:224–228.
Assalia A, Gagner M. Laparoscopic Adrenalectomy. Br J Surg 2004;91:1259–1274.
Klingler PJ, Tsiotos GG, Glaser KS, Hinder RA. Laparoscopic splenectomy: evolution and current status. Surg Laparosc Endosc 1999;9:1–8.
Jesch NK, Metzelder ML, Kuebler JF, Ure BM. Laparoscopic transperitoneal nephrectomy is feasible in the first year of life and is not affected by the kidney size. J Urol 2006;176:1177–1179.
Priest J, Williams GM, Hill DA, Dehner LP, Jaffé A. Pulmonary cyst in early childhood and the risk of malignancy. Pediatr Pulmonol 2009;44:14–30.
Nasr A, Himidan S, Pastor AC, Taylor G, Kim PC. Is congenital cystic adenomatoid malformation a premalignant lesion for pleuropulmonary blastoma? J Pediatr Surg 2010;45:1086–1089.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reismann, M., Gossner, J., Glueer, S. et al. Thoracoscopic resection of congenital pulmonary malformations in infants: is the feasibility related to the size of the lesion?. World J Pediatr 8, 272–274 (2012). https://doi.org/10.1007/s12519-011-0283-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-011-0283-7