Abstract
Aim
To evaluate the distribution of a generic diastolic pressure ratio (dPR) after angiographically successful percutaneous coronary intervention (PCI) and to assess its association with the 2‑year incidence of target vessel failure (TVF), defined as a composite of cardiac mortality, target vessel revascularisation, target vessel myocardial infarction and stent thrombosis.
Methods
The dPR SEARCH study is a post hoc analysis of the prospective single-centre FFR-SEARCH registry, in which physiological assessment was performed after angiographically successful PCI in a total of 1000 patients, using a dedicated microcatheter. dPR was calculated offline with recently validated software in a subset of 735 patients.
Results
Mean post-PCI dPR was 0.95 ± 0.06. Post-PCI dPR was ≤ 0.89 in 15.2% of the patients. The cumulative incidence of TVF at 2‑year follow-up was 9.4% in patients with a final post-PCI dPR ≤ 0.89 as compared to 6.1% in patients with a post-PCI dPR > 0.89 (adjusted hazard ratio [HR] for dPR ≤ 0.89: 1.53; 95% CI 0.74–3.13; p = 0.249). dPR ≤ 0.89 was associated with significantly higher cardiac mortality at 2 years; adjusted HR 2.40; 95% CI 1.01–5.68; p = 0.047.
Conclusions
In a real-world setting, despite optimal angiographic PCI results, 15.2% of the patients had a final post-PCI dPR of ≤ 0.89, which was associated with a higher incidence of TVF and a significantly higher cardiac mortality rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
-
The resting index diastolic pressure ratio (dPR) is an excellent alternative to the instantaneous wave-free ratio (iFR).
-
Despite angiographically successful percutaneous coronary intervention (PCI), in a significant number of vessels the post-PCI dPR remains suboptimal (≤ 0.89).
-
Post-PCI dPR is associated with clinical outcome at follow-up.
Introduction
An increasing body of evidence supports the use of either fractional flow reserve (FFR) or the non-hyperaemic instantaneous wave-free ratio (iFR) for intracoronary physiological assessment of intermediate coronary artery lesions [1, 2]. Recently, a series of so-called non-hyperaemic pressure ratios (NHPRs) have been validated and proved to have a nearly perfect correlation to iFR, enhancing the adoption of general NHPRs in real-world clinical practice [3,4,5]. At the same time, the use of post-percutaneous coronary intervention (post-PCI) physiological assessment is gaining attention. A strong and linear association has been demonstrated between post-PCI FFR and the risk for both future repeat revascularisation as well as hard clinical endpoints such as death and myocardial infarction [6,7,8]. The relevance of the latter was strengthened by recent work by our group demonstrating that post-PCI FFR values were < 0.90 in up to 37.8% of stented vessels despite optimal angiographic results [9]. With respect to post-PCI NHPRs, the recently published DEFINE PCI study showed that 22.6% of treated vessels had a final post-PCI iFR ≤ 0.89 [10].
To date, limited data are available on the distribution of post-PCI NHPRs and their prognostic value. The aim of the present study was to evaluate the distribution of a recently validated generic diastolic pressure ratio (dPR) after angiographically successful PCI in an all-comers study population and to study its association with 2‑year clinical outcome.
Methods
Study design and patient population
The dPR SEARCH study was a post hoc analysis of the FFR-SEARCH registry (Stent Evaluated at Rotterdam Cardiology Hospital), a prospective single-centre registry in which routine FFR measurements were performed after angiographically successful PCI in a total of 1000 patients between March 2016 and May 2017 [9]. Exclusion criteria were: (1) patients presenting with cardiogenic shock, (2) ‘high-risk’ procedures defined as use of mechanical circulatory support, (3) age < 18 years and (4) an estimated vessel size < 2.25 mm. A total of 735 patients (735 vessels) with available undamped pressure waveform data were selected for the present study (Fig. 1).
The study was performed in accordance with the Declaration of Helsinki. The study protocol was approved by the local ethics committee of the Erasmus Medical Centre. Participants were informed about the study by the physician responsible for the procedure and provided informed consent for the procedure and the use of anonymous datasets for research purposes in alignment with the Dutch Medical Research Act.
Coronary angiography and calculation of FFR
All procedures were performed according to standard local clinical practice with the use of intracoronary imaging and physiology at the operator’s discretion. All vessels, including in-stent restenosis cases, were treated with a stent. Comprehensive quantitative coronary angiography analyses were performed pre- and post-stent implantation in all treated lesions. An angiographic view with minimal foreshortening of the lesion and minimal overlap with other vessels was selected. Similar angiographic views were used pre- and post-stent implantation. Measurements included: pre- and post-procedural percentage diameter stenosis; reference vessel diameter; lesion length and minimal luminal diameter (MLD). In patients with a total occlusion (those presenting with ST-elevation myocardial infarction [STEMI] or a chronic total occlusion [CTO]), the MLD was considered zero and percentage diameter stenosis 100%. Reference vessel diameter and lesion length were calculated from the first angiographic view with restored flow. All angiographic measurements were performed using CAAS for Windows, version 2.11.2 (Pie Medical Imaging, Maastricht, The Netherlands).
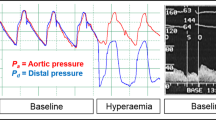
Pressure measurements were performed after an intracoronary bolus of nitrates (100–200 µg) using a dedicated rapid exchange monorail microcatheter (Navvus RXi system; ACIST Medical Systems Inc., Eden Prairie, MN, USA), with a fibre-optic-based sensor technology compatible with standard 0.014-inch guidewires [11, 12]. After equalisation of the system based on undampened pressure waveforms, the device was inserted over the previously used coronary guidewire approximately 20 mm distal to the most distal stent edge, at which point Pd/Pa was measured. FFR values were subsequently recorded at four different positions in the coronary artery: (1) 20 mm distal to the distal stent edge, (2) at the distal stent edge, (3) at the proximal stent edge and (4) at the coronary ostium to verify the occurrence of drift. In cases of significant drift (≥ 3 units) measurements were repeated. All analyses performed in the present study were based on values measured 20 mm distal to the most distal stent edge. In patients in which dPR was assessed in multiple vessels, only the vessel with the lowest dPR was included.
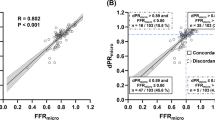
Definition and calculation of dPR
Pd/Pa was defined as the ratio of mean distal coronary artery pressure to mean aortic pressure in the resting state during the whole cardiac cycle. FFR was defined as the lowest ratio of mean distal coronary artery pressure divided by mean aortic pressure during maximal hyperaemia. dPR was defined as the ratio between the mean diastolic pressure distal to the stenosis and the mean diastolic aortic pressure in resting conditions, taken over an average of 5 consecutive heartbeats, based on the initial distal resting Pd/Pa. The dPR was calculated retrospectively using recently validated dedicated software developed at the Erasmus Medical Centre [3]. Briefly, the diastolic period used to calculate the dPR was automatically delineated based on the dP/dt curve of the aortic pressure at the point at which the resistance was low, constant and stable. The dP/dt curve represents the increase and decrease of the pressure over time during the heart cycle. dP is the pressure difference between sample points and dt is the time difference between the same sample points.
Endpoint definitions and clinical follow up
The primary endpoint consisted of target vessel failure (TVF), defined as a composite of cardiac mortality, target vessel revascularisation (TVR), target vessel myocardial infarction (TVMI) and stent thrombosis (ST) at 2 years. Secondary endpoints included the individual components of the primary endpoint and all-cause mortality. Clinical follow-up data were obtained from electronic medical records of the hospital and general practitioner. Survival data were obtained from the municipal civil registry. In addition, all surviving patients were contacted in person or by telephone with specific queries on clinical outcome. Cardiac mortality was defined as any death due to a proximate cardiac cause, unwitnessed death or death of unknown cause [13]. Myocardial infarction was diagnosed in accordance with the expert consensus document, defined as a rise and/or fall of troponin with at least one value above the 99th percentile of the upper reference limit together with evidence of myocardial ischaemia with at least one of the following: (1) symptoms of ischaemia, (2) electrocardiographic changes indicative of new ischaemia (new ST-segment and T‑wave changes or new left bundle branch block), (3) development of pathological waves in the electrocardiogram and (4) imaging evidence of new loss of viable myocardium or new regional wall motion abnormality [14, 15]. ST was defined as angiographically defined thrombosis within the stent or 5 mm proximal or distal to the stent with the presence of a flow-limiting thrombus, accompanied by acute symptoms. Event adjudication was performed by trained study personnel unaware of the final physiological assessment.
Statistical analysis
Baseline, categorical variables are reported as either counts or percentages and reported as mean ± standard deviation. The association between dPR and clinical endpoints was analysed by Cox proportional hazard regression analysis. Univariate predictors of outcomes were identified using the Cox proportional-hazards model. Clinically relevant variables (age, male gender, diabetes mellitus and STEMI at presentation) were introduced into the multivariate Cox proportional-hazards model using the ‘enter’ method. Data are presented as hazard ratio (HR) with a 95% confidence interval (95% CI). All tests were two-tailed and a p-value < 0.05 was considered statistically significant. The Kaplan-Meier method was applied to show the cumulative incidence of the primary and secondary endpoints, whereas log-rank tests were used to evaluate differences between the groups. Patients that were lost to follow-up were censored at the date of the last contact. Receiver-operating characteristic (ROC) curve analysis was performed to assess the optimal cut-off value of post-PCI dPR for predicting clinical outcome. However, due to the limited number of events, the ROC curve was not able to identify a final post-PCI dPR value to predict TVF (Electronic Supplementary Material, Fig. S1). Given the exploratory nature of the present study, we deliberately took the accepted ischaemic dPR threshold of 0.89 as a cut-off value to predict clinical outcome. A predefined subgroup analysis was performed in patients presenting with stable- or unstable angina or non-STEMI (NSTEMI). Statistical analyses were performed using SPSS statistics for Windows, version 24.0 (SPSS, Chicago, IL, USA).
Results
Patient demographics and procedural data
A total of 735 patients (735 vessels) were included. Patients’ baseline characteristics are depicted in Tab. 1. In brief, 75% of the patients were male and average age was 64 ± 12 years. Hypertension was present in 51% of the cases and 19% were diabetic. Clinical presentation was stable angina in 31% of the cases, whereas 36% and 33% of the patients presented with NSTEMI and STEMI, respectively. Vessel and lesion characteristics are presented in Tab. 2.
Distribution of dPR and clinical outcome at 2 year follow up
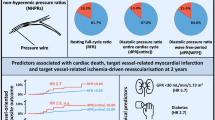
Mean post-PCI dPR was 0.95 ± 0.06. Mean drift was 0.01 ± 0.01. Post-PCI dPR was ≤ 0.89 in 15.2% of the cases (Fig. 2). The cumulative incidence of TVF was 6.1% in patients with a final post-PCI dPR ≤ 0.89 as compared to 9.4% in patients with a post-PCI dPR > 0.89 [adjusted HR for dPR ≤ 0.89: 1.53; 95% CI 0.74–3.13; p = 0.249]. Cardiac mortality rates were significantly higher in patients with a final post-PCI dPR ≤ 0.89 as compared to those with a dPR > 0.89 [7.4% vs 3.1%, adjusted HR 2.40, 95% CI 1.01–5.68; p = 0.047] (Fig. 3; Tab. 3; and Electronic Supplementary Material, Tab. S1).
Cumulative incidence of target vessel failure (TVF) and cardiac death at 2‑year follow-up. (TVR target vessel revascularisation, TVMI target vessel myocardial infarction, ST stent thrombosis, HR hazard ratio, CI confidence interval, PCI percutaneous coronary intervention, dPR diastolic pressure ratio)
Stratified analysis in patients presenting with stable or unstable angina or NSTEMI
A total of 494 patients (67.2%) presented with stable- or unstable angina or NSTEMI. The cumulative incidence of TVF was 11.8% in patients with a final post-PCI dPR ≤ 0.89 as compared to 6.5% in patients with a post-PCI dPR > 0.89 [adjusted HR for dPR ≤ 0.89: 1.92; 95% CI 0.91–4.01; p = 0.070] (Electronic Supplementary Material, Fig. S2).
Discussion
In the present study focusing on the real world impact of post-PCI dPR, we demonstrated that: (1) despite optimal angiographic results 15.2% of the vessels have a final post-PCI dPR of ≤ 0.89; (2) the incidence of TVF was higher in patients with post-PCI dPR ≤ 0.89; however, (3) a post-PCI dPR ≤ 0.89 was associated with a higher cardiac mortality rate.
Despite the unequivocal evidence supporting the use of pre-PCI physiological lesion assessment, the use of the technology in a post-PCI setting is still rare. Instead, post-PCI results are routinely assessed by visual angiographic assessment, a technique that has repeatedly been shown to correlate poorly with invasive functional assessment [16,17,18]. The importance of the latter is further illustrated by a growing body of evidence showing the strong predictive value of post-PCI FFR for future adverse events [19,20,21,22]. However, little is known about the use of post-PCI dPR and its predictive value. To the best of our knowledge, the present study is the largest on the distribution and predictive value of post-PCI dPR to date and the first to assess the correlation between post-PCI dPR and 2‑year clinical outcome.
We were able to demonstrate that in an all-comers study population, despite satisfactory angiographic results, 15.2% of the patients had a post-PCI dPR ≤ 0.89. Our work thereby complements the findings of the DEFINE PCI study, in which 22.6% of the treated vessels had a final post-PCI iFR ≤ 0.89 [10]. Our work, however, differed from the DEFINE PCI study by enrolling a larger and more real-world patient population, in which patients with prior coronary artery bypass graft, CTO treatment, STEMI and TIMI flow < 3 were not excluded. Especially the inclusion of patients presenting with STEMI and the lower number of patients with diabetes (19% vs 34%, respectively) might explain the lower number of patients with a post-PCI dPR ≤ 0.89 as compared to those in the DEFINE PCI study [23]. Despite the restoration of epicardial flow through PCI, patients with STEMI have abnormal myocardial perfusion at the end of the procedure [24]. This phenomenon is thought to be related to microvascular obstruction due to distal embolisation, reperfusion injury and tissue inflammation due to myocyte necrosis [25]. In addition, physiological assessment in patients with diabetes mellitus underestimates the disease severity because of diffuse coronary atherosclerosis, microvascular disease and a tendency for negative remodelling [26]. The last-mentioned resulted in the pre-defined subanalysis in patients presenting with stable or unstable angina or NSTEMI, in which a more pronounced effect of post-PCI dPR ≤ 0.89 was seen to predict 2‑year TVF rates.
In the present study pressure measurements were performed approximately 20 mm distal to the distal stent edge, while in the DEFINE PCI study the investigators reported consistently placing their pressure sensors in the distal third of the study vessel, which is another potential explanation for the lower proportion of patients with dPR ≤ 0.89 in the present study.
Despite a growing body of evidence on the strong correlation between post-PCI FFR and the risk for future adverse cardiovascular events, the present study is the first to assess the correlation between post-PCI dPR and clinical outcome at 2 years [21, 22]. We found a higher incidence of TVF in patients with post-PCI dPR ≤ 0.89 as compared to those with a dPR > 0.89. More specifically, a post-PCI dPR ≤ 0.89 proved to be associated with a 2.4-fold increased risk for cardiac mortality at 2 years when corrected for clinically relevant variables such as age, gender, diabetes mellitus and STEMI at presentation (p = 0.047). Association of low post-PCI dPR and increased risk for cardiac mortality is in line with the results of the recently presented 1‑year follow-up of the DEFINE PCI study, which showed that post-PCI iFR < 0.95 was associated with lower event rates [27].
The microcatheter-based FFR system has a small lumen profile (maximum diameter 0.036 inch at sensor level and 0.025 inch at optical-fibre level) offering some potential advantages as compared to the conventional pressure-wire-based systems, including easy delivery over routine coronary guidewires and the use of a fibre-optic sensor that proved to significantly reduce drift as compared to conventional pressure wires with piezoelectric sensors [28]. Conversely, previous studies demonstrated that microcatheter-based systems may slightly overestimate stenosis severity as compared to the conventional wire-based FFR systems. The mean overall bias between microcatheter FFR and conventional wire-based FFR was −0.029 (microcatheter FFR was lower), a bias that proved mostly relevant in the case of lower FFR values or small-calibre vessels [29, 30]. In the present study the measurements were performed after angiographically successful stenting. Subsequent mean FFR values were therefore relatively high (mean 0.90) and significantly higher as compared to, for instance, the mean FFR values in the ACIST-FFR study (FFR 0.81) [28]. Therefore, the authors believe that in the present study the impact of smaller luminal diameters on the bias between microcatheter- and pressure-wire-based values was limited.
The present study demonstrates the feasibility of post-PCI physiological assessment using a dedicated monorail microcatheter without the need for hyperaemic agents associated with increased time, costs and side-effects. Routine physiological post-PCI dPR assessment identifies a significant number of patients with suboptimal post-PCI results that are at increased risk for future adverse cardiac events. The ongoing randomised FFR-REACT trial will assess whether invasive imaging and PCI optimisation (using additional stents and post-dilation) will improve outcomes in patients with suboptimal post-PCI physiological measurements [31].
Limitations
Several limitations deserve to be mentioned. First of all, post-physiological assessment was performed using the Navvus microcatheter, which is an over-the-wire microcatheter with a profile of 0.022 inch that resulted in a slightly but significantly lower FFR (by 1–3%) as compared to the conventional 0.014-inch pressure wires [32]. In addition, the results are based on a single-centre experience in which we restricted our analyses to recordings with adequate pressure waveforms. The latter could have artificially influenced our results, since previous work, assessing the prevalence of erroneous or suboptimal FFR measurements in clinical practice, demonstrated that in up to 30% of the recordings, pressure signals were inadequate [33]. Furthermore, due to the nature of our real-world registry, in which most patients were referred for PCI by satellite hospitals, left ventricular (LV) function was missing in a considerable number of cases. Given the high number of missing values we decided to refrain from adjusting our findings for LV function. Finally, the data acquisition protocol of the FFR-SEARCH registry included only a pullback during maximum hyperaemia, precluding us from analysing detailed post-procedural dPR gradients within the treated vessel.
Conclusion
Despite optimal angiographic PCI results, 15.2% of the patients had a final post-PCI dPR of ≤ 0.89, which was associated with a significantly higher cardiac mortality rate. The incidence of TVF was higher in patients with post-PCI dPR ≤ 0.89.
References
Davies JE, Sen S, Dehbi HM, et al. Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N Engl J Med. 2017;376:1824–34.
Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–24.
Ligthart J, Masdjedi K, Witberg K, et al. Validation of resting diastolic pressure ratio calculated by a novel algorithm and its correlation with distal coronary artery pressure to aortic pressure, instantaneous wave-free ratio, and fractional flow reserve. Circ Cardiovasc Interv. 2018;11:e6911.
Svanerud J, Ahn JM, Jeremias A, et al. Validation of a novel non-hyperaemic index of coronary artery stenosis severity: the Resting Full-cycle Ratio (VALIDATE RFR) study. EuroIntervention. 2018;14:806–14.
Van’t Veer M, Pijls NHJ, Hennigan B, et al. Comparison of different diastolic resting indexes to iFR: are they all equal? J Am Coll Cardiol. 2017;70:3088–96.
Agarwal SK, Kasula S, Hacioglu Y, Ahmed Z, Uretsky BF, Hakeem A. Utilizing post-intervention fractional flow reserve to optimize acute results and the relationship to long-term outcomes. JACC Cardiovasc Interv. 2016;9:1022–31.
Leesar MA, Satran A, Yalamanchili V, Helmy T, Abdul-Waheed M, Wongpraparut N. The impact of fractional flow reserve measurement on clinical outcomes after transradial coronary stenting. EuroIntervention. 2011;7:917–23.
Pijls NH, Klauss V, Siebert U, et al. Coronary pressure measurement after stenting predicts adverse events at follow-up: a multicenter registry. Circulation. 2002;105:2950–4.
Diletti R, Masdjedi K, Daemen J, et al. Impact of poststenting fractional flow reserve on long-term clinical outcomes: the FFR-SEARCH study. Circ Cardiovasc Interv. 2021;14:e9681.
Jeremias A, Davies JE, Maehara A, et al. Blinded physiological assessment of residual ischemia after successful angiographic percutaneous coronary intervention: the DEFINE PCI study. JACC Cardiovasc Interv. 2019;12:1991–2001.
Diletti R, Van Mieghem NM, Valgimigli M, et al. Rapid exchange ultra-thin microcatheter using fibre-optic sensing technology for measurement of intracoronary fractional flow reserve. EuroIntervention. 2015;11:428–32.
Menon M, Jaffe W, Watson T, Webster M. Assessment of coronary fractional flow reserve using a monorail pressure catheter: the first-in-human ACCESS-NZ trial. EuroIntervention. 2015;11:257–63.
Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115:2344–51.
Thygesen K. ‘Ten commandments’ for the fourth universal definition of myocardial infarction 2018. Eur Heart J. 2019;40:226.
Thygesen K. What’s new in the fourth universal definition of myocardial infarction? Eur Heart J. 2018;39:3757–8.
Nakamura M, Yamagishi M, Ueno T, et al. Prevalence of visual-functional mismatch regarding coronary artery stenosis in the CVIT-DEFER registry. Cardiovasc Interv Ther. 2014;29:300–8.
Park SJ, Kang SJ, Ahn JM, et al. Visual-functional mismatch between coronary angiography and fractional flow reserve. JACC Cardiovasc Interv. 2012;5:1029–36.
Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816–21.
Agarwal SK, Kasula S, Almomani A, et al. Clinical and angiographic predictors of persistently ischemic fractional flow reserve after percutaneous revascularization. Am Heart J. 2017;184:10–6.
Ishii H, Kataoka T, Kobayashi Y, et al. Utility of myocardial fractional flow reserve for prediction of restenosis following sirolimus-eluting stent implantation. Heart Vessels. 2011;26:572–81.
Johnson NP, Toth GG, Lai D, et al. Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol. 2014;64:1641–54.
Nam CW, Hur SH, Cho YK, et al. Relation of fractional flow reserve after drug-eluting stent implantation to one-year outcomes. Am J Cardiol. 2011;107:1763–7.
Jeremias A, Davies JE, Maehara A, Matsumura M, Schneider J, Tang K, et al. Blinded physiological assessment of residual ischemia after successful angiographic percutaneous coronary intervention: the DEFINE PCI study. JACC Cardiovasc Interv. 2019;12:1991–2001.
Stone GW, Webb J, Cox DA, et al. Distal microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction: a randomized controlled trial. JAMA. 2005;293:1063–72.
Shah NR, Al-Lamee R, Davies JE. Fractional flow reserve in acute coronary syndromes: a review. Int J Cardiol Heart Vasc. 2014;5:20–5.
Bishop AH, Samady H. Fractional flow reserve: critical review of an important physiologic adjunct to angiography. Am Heart J. 2004;147:792–802.
Patel MR, Jeremias A, Maehara A, Matsumura M, Zhang Z, Schneider J, et al. 1‑Year outcomes of blinded physiological assessment of residual ischemia after successful PCI: DEFINE PCI trial. JACC Cardiovasc Interv. 2022;15:52–61.
Fearon WF, Chambers JW, Seto AH, et al. ACIST-FFR study (assessment of catheter-based interrogation and standard techniques for fractional flow reserve measurement). Circ Cardiovasc Interv. 2017;10:e5905.
Ali ZA, Parviz Y, Brinkman M, et al. Pressure wire compared to microcatheter sensing for coronary fractional flow reserve: the PERFORM study. EuroIntervention. 2018;14:e459–e66.
Seligman H, Shun-Shin MJ, Vasireddy A, et al. Fractional flow reserve derived from microcatheters versus standard pressure wires: a stenosis-level meta-analysis. Open Heart. 2019;6:e971.
van Zandvoort LJC, Masdjedi K, Tovar Forero MN, et al. Fractional flow reserve guided percutaneous coronary intervention optimization directed by high-definition intravascular ultrasound versus standard of care: Rationale and study design of the prospective randomized FFR-REACT trial. Am Heart J. 2019;213:66–72.
Pouillot C, Fournier S, Glasenapp J, et al. Pressure wire versus microcatheter for FFR measurement: a head-to-head comparison. EuroIntervention. 2018;13:e1850–e6.
Matsumura M, Johnson NP, Fearon WF, et al. Accuracy of fractional flow reserve measurements in clinical practice: observations from a core laboratory analysis. JACC Cardiovasc Interv. 2017;10:1392–401.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. Masdjedi: institutional research grant support from ACIST Medical. L.J.C. van Zandvoort: institutional research grant support from ACIST Medical. N.M. Van Mieghem: research grant support from Edwards, Medtronic, Abbott, Boston Scientific, Pulse Cath, ACIST Medical, Essential Medical. J. Daemen: institutional grant/research support from Astra Zeneca, Abbott Vascular, Boston Scientific, ACIST Medical, Medtronic, Pie Medical, and ReCor Medical. T. Neleman, I. Kardys, J. Ligthart, W.K. Den Dekker, R. Diletti and F. Zijlstra declare that they have no competing interests.
Supplementary Information
12471_2022_1680_MOESM3_ESM.tif
Fig. S2 Cumulative incidence of target vessel failure (Cardiac death, TVR, TVMI, ST) in patients without SETMI. HR hazard ratio, CI confidence interval, PCI percutaneous coronary intervention, dPR diastolic pressure ratio.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Masdjedi, K., van Zandvoort, L.J.C., Neleman, T. et al. Prognostic value of post-percutaneous coronary intervention diastolic pressure ratio. Neth Heart J 30, 352–359 (2022). https://doi.org/10.1007/s12471-022-01680-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-022-01680-0