Abstract
Background
In our institution, we have redefined our criteria for direct availability of red blood cell (RBC) units in the operation room. In this study, we sought to evaluate the safety of applying this new logistical policy of blood transfusion in the first preliminary group of patients.
Methods
In March 2010, we started a new policy concerning the elective availability of RBC units in the operation room. This policy was called: No Elective Red Cells (NERC) program. The program was applied for patients undergoing primary isolated coronary artery bypass grafting (CABG) or single valve surgery. No elective RBC units were preoperatively ordered for these patients. In case of urgent need, blood was delivered to the operating room within 20 min. The present study includes the first 500 patients who were managed according to this policy. Logistic regression analyses were performed to investigate the impact of biomedical variables on fulfilling this NERC program.
Results
The majority of patients (n = 409, 81 %) did not receive any RBCs during the hospital stay. In patients who did receive RBCs (n = 91, 19 %), 11 patients (2.2 %) received RBCs after 24 h postoperatively. Female gender, left ventricular ejection fraction (LVEF) and EuroSCORE were significant predictors for the need of blood transfusion (OR = 3.12; 2.79; 1.17 respectively).
Conclusion
In a selected group of patients, it is safe to perform cardiac surgery without the immediate availability of RBCs in the operating room. Transfusion was avoided in 81 % of these patients. Female gender, LVEF and EuroSCORE were associated with blood transfusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Perioperative transfusion of red blood cells (RBCs) has been associated with increased mortality, morbidity, costs and decreased long-term survival after cardiac surgery [1, 2]. The severity of the adverse effects of perioperative RBC transfusion is dose-dependent. Unnecessary transfusion might cause postoperative complications and subsequent hospitalisation costs [1, 3]. In an earlier report [4], we identified the independent, patient-related risk factors of RBC transfusion after coronary artery bypass grafting (CABG). Identification of these risk factors led us to follow a new policy concerning the direct availability of packed RBCs in the operating theatre. It was standard practice in our hospital to have two units of RBCs directly available in the operating theatre for every patient who is scheduled for an elective CABG. If these two units are not used, they are returned to the laboratory to be used for another patient. The quality of these RBCs is sometimes reduced and the RBCs cannot be used anymore. Since March 2010, we have followed a policy that is called: No Elective Red Cells (NERC) protocol. With this new protocol, in a selected group of patients, no units of RBCs are directly available in the operating theatre. According to this protocol, RBCs that are available in the blood bank are delivered into the operating room within 20 min after request.
In the present study, we have analysed our results of the first consecutive 500 patients who were managed according to the NERC protocol.
Materials and methods
The NERC protocol
In our institution, we have started a new strategy concerning direct availability of RBC units in the operating room for a selected group of patients undergoing cardiac surgery. In this group of patients, only ABO typing and screening for irregular antibodies without cross matching were performed. Units of RBCs were kept in the hospital’s blood bank. All patients were examined in the preoperative screening in the outpatient clinic to select suitable candidates for the NERC program. For patients included in the protocol, no RBCs were ordered before the operation. Patients included in the NERC program were screened for blood type and irregular antibodies the day before surgery. In case of urgent need for transfusion of RBCs during or immediately after the operation, the local blood bank prepared the RBCs, including electronic cross matching, and delivered them within 20 min. Uncross-matched blood was not given to any of the patients in this population.
We always perform a double ABO screening including the Rh typing. In addition, we performed one screening on irregular antibodies for every patient. These tests are valid for 48 h. Afterwards, a double ABO and antibody screenings should be repeated.
Patients
The study included the first consecutive 500 patients who were managed according to the NERC protocol starting in March 2010. Approval was obtained from the institution’s research review board that waived the need for informed consent. Data of demographics, operative techniques, blood transfusions and adverse events were prospectively collected in the computerised database of our department.
Patients were managed according to the NERC protocol when they fulfilled the following criteria:
-
Isolated primary coronary artery bypass grafting (CABG), isolated aortic valve replacement (AVR) or isolated mitral valve surgery.
-
Preoperative haemoglobin (Hb) level of >7.0 mmol/L (11.3 g/dL).
-
Body surface area (BSA) of >1.7 m2.
-
Negative test for irregular antibodies.
Patients were excluded from the NERC protocol in case of the following criteria:
-
Combined CABG and/or valve surgery.
-
Prior cardiac surgery.
-
Positive test for irregular antibodies.
Operative technique
All patients received short-acting anaesthetic drugs to facilitate early extubation and rapid recovery according to our daily practice. Normothermic extracorporeal circulation (ECC) was performed using non-pulsatile flow. Cold crystalloid cardioplegia (St Thomas’ solution) or warm blood cardioplegia was used to induce and maintain cardioplegic cardiac arrest, according to the surgeon’s preference. Cell saver was used to collect all shed and/or residual blood, which was retransfused immediately after the operation.
Indications of RBC transfusion
In our hospital, transfusion of one or more units of RBC is indicated in the postoperative period in case of a haemoglobin level of <5 mmol/L (8 g/dL) or a haematocrit value of <0.25. A haemoglobin level of <6 mmol/L (9.5 g/dL) is adopted in case of haemodynamically unstable patients or patients with postoperative ischaemia or excessive bleeding. If the patient did not fulfil any of these criteria, no blood transfusion was given.
Statistics
Continuous variables are expressed as mean ± SD and categorical data are expressed as numbers (percentage). Univariate logistic regression analyses were performed to investigate the impact of biomedical variables on fulfilling the NERC protocol. A P-value < 0.05 was used for all tests to indicate statistical significance. Odds ratios (OR) with a confidence interval (CI) of 95 % with p-values are reported. All statistical analyses were performed using SPPS version 17.0 (SPSS Inc, Chicago, IL).
Results
Starting in March 2010, 500 consecutive patients underwent cardiac surgery in our hospital and fulfilled the criteria for the NERC protocol. Demographic data and comorbidities are shown in Table 1. The majority of patients were male (82 %). The following comorbidities were present: diabetes (19 %), hypertension (52.8 %), severe renal function impairment (1.2 %), chronic obstructive pulmonary disease (COPD) (9 %), peripheral vascular disease (PVD) (13.6 %), history of preoperative atrial fibrillation (4.4 %) and preoperative myocardial infarction (37.6 %). The mean logistic EuroSCORE was 3.2 ± 3.3 and the mean additive EuroSCORE was 3.1 ± 2.3.
Table 2 shows the type of the operations performed. The majority of patients underwent coronary artery bypass grafting (CABG) including on pump (74 %) and off pump (OPCAB) (12 %) surgery. An overview of the number of transfusions of blood products in the first 24 h is given in Table 3.
The number of patients who did not receive any RBCs during hospital stay was 409 (81 %). Sixty-one patients (12.2 %) received 1–2 units of blood and 14 patients (2.8 %) received 3–5 units of blood within the first 24 h after surgery. In all these patients, blood was available within 20 min as planned. Only 11 patients (2.2 %) received RBCs on the ward after 24 h of surgery.
The mean serum haemoglobin was 6.4 ± 0.8 mmol/l (10.3 ± 1.3 g/dL) on the first postoperative day, and 6.8 ± 0.8 mmol/l (11 ± 1.3 g/dL) on the third postoperative day.
Table 3 shows the number of transfused blood products, the level of serum haemoglobin, transfusion of RBCs as well as fresh frozen plasma (FFP) units. The serum haemoglobin levels in the first and third postoperative days are also shown.
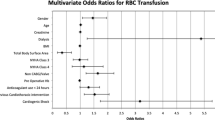
Postoperative complications (Table 4) included re-exploration for bleeding (4.6 %), myocardial infarction (3.2 %), cerebrovascular accident (CVA) (0.4 %) and deep sternal wound infection (0.6 %). Results of the univariate logistic regression analysis for the need for blood transfusion are shown in Table 5. Female gender (OR = 3.12) and LVEF <35 % (OR = 2.79) predicted a higher risk of blood transfusion. A higher logistic (OR = 1.06) and a higher additive EuroSCORE (OR = 1.17) are significant predictors for the need of RBC transfusion.
Discussion
This study demonstrated, in a selected group of patients, that it is safe to perform cardiac surgery without the immediate availability of RBCs in the operating room. This resulted in a considerable reduction in cross-matching and transportation with possible damage of non-used RBC. We used data from an earlier report of our group [4] to identify patients with a relatively low risk for receiving perioperative RBC transfusions.
Transfusion of RBCs is not only associated with an increase in morbidity and mortality, but also with a longer ICU stay and total hospital stay [1]. Moreover, the effect of duration of storage of RBC on morbidity has been addressed [5–10]. In an earlier retrospective analysis of 10,626 patients undergoing cardiac surgery in our institution [2], we found a significant correlation between the number of RBC units received by the patients and the incidence of early mortality. McKenny et al. [9] also found the number of transfused RBC units to be associated with adverse outcome and longer hospital stay after cardiac surgery. Koch et al. [11] found significantly reduced survival among transfused patients compared with non-transfused patients. Both early (6 months) and late hazard phases (up to 10 years) showed that transfusion of red cells is associated with a decreased survival in isolated CABG patients. According to these authors, attention should be directed toward blood conservation methods and a more judicious use of the RBCs [11].
One of the primary rationales of the NERC protocol is to help maintenance of adequate preservation of the RBCs. Non-used units of blood must be returned back to the blood bank for further use. However, the quality of these RBC units is likely to be adversely influenced by the improper reservation in the operation room as well as during transport [12]. The value of transfusion of these RBC units is physiologically less effective and can even increase the incidence of postoperative complications [13–15].
The effect of storage time of RBCs on the outcome after cardiac surgery has gained an increasing interest in recent literature. In an earlier study, storage time of the RBCs was not found to be a significant predictor of early or late mortality after CABG in our centre [5]. The endpoint of that study was all-cause mortality without analysing the effect of storage time of RBCs on morbidity.
On the other hand, Sanders et al. [10] found that patients receiving older blood have an increased incidence of prolonged hospital stay and renal complications compared with those receiving new blood [10]. Koch et al.[6] also found a correlation between transfusion of old blood and mortality and both renal and pulmonary complications after cardiac surgery. The controversy between different reports might be explained by the various patient populations studied, differences in study design or analysis, or different methods of blood storage. [5]
The criteria of selected patients who are candidates of this NERC protocol are of utmost importance. We applied these criteria after studying the risk factors of perioperative transfusion in our centre [4]. These criteria can vary in different centres and according to the availability of RBC units. If the blood is not electively ordered, it must be possible to deliver it on time if urgently needed.
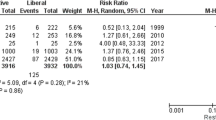
Several blood conservation strategies [16–18] have been proposed in order to improve outcome after cardiac surgery, reduce the need for donor blood and hence lower the overall costs of transfusion. A wide variation in clinical practice and the application of guidelines have been reported in as many as 1402 surveys in 1061 institutions in the United States and Canada [19] Most of these studies examined liberal versus restrictive transfusion practices in cardiac surgery. However, there is no prospective randomised trial comparing the outcomes of a program that practises blood conservation versus the common practice of blood use in cardiac surgery [20]. Our NERC protocol is prospectively designed and the data of patients are prospectively collected as well. Only 19 % of the patients needed blood transfusions during the whole hospital stay. In all these patients, the blood needed was immediately available on site in the hospital. In the present study, the incidence of postoperative complications is comparable with the general incidence of complications in our institution as demonstrated in previous studies of similar patients in our department [2]. Univariate predictors of postoperative need for blood transfusion were found to be gender (female sex), LVEF <35 %, logistic and additive EuroSCORE.
The use of cell saver for shed blood or residual blood is a routine in our daily cardiac surgical practice. Current evidence suggests that the use of a cell saver reduces exposure to allergenic blood products or red blood cell transfusion for patients undergoing cardiac surgery [21].
Limitations
The results of this observational single-centre study must be interpreted with caution. Our findings were the result of the local protocol agreed upon by a team of anaesthesiologists, ICU physicians, cardiac surgeons and the blood bank. Whether the same results can be applied to other institutions remains to be investigated. The lack of a control group is also a shortcoming. However, matching this group with another group that was operated earlier was not convenient.
Conclusions
In a selected group of patients, it is safe to perform cardiac surgery without the immediate availability of RBCs in the operating room. Preoperative univariate predictors of the need for postoperative RBC transfusion were female gender, left ventricular function (LVEF) <35 % and the EuroSCORE.
References
Murphy GJ, Reeves BC, Rogers CA, et al. Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007;116(22):2544–52.
van Straten AH, Bekker MW, Soliman Hamad MA, et al. Transfusion of red blood cells: the impact on short-term and long-term survival after coronary artery bypass grafting, a ten-year follow-up. Interact Cardiovasc Thorac Surg. 2010;10(1):37–42.
Koch CG, Li L, Duncan AI, et al. Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med. 2006;34:1608–16.
van Straten AH, Kats S, Bekker MW, et al. Risk factors for red blood cell transfusion after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2010;24:413–7.
van Straten AH, Soliman Hamad MA, van Zundert AA. Martens EJ, ter Woorst JF, de Wolf AM Effect of duration of red blood cell storage on early and late mortality after coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2011;141(1):231–7.
Koch CG, Li L, Sessler DI, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med. 2008;20(358):1229–39.
Basran S, Frumento RJ, Cohen A, et al. The association between duration of storage of transfused red blood cells and morbidity and mortality after reoperative cardiac surgery. Anesth Analg. 2006;103:15–20.
Van de Watering L, Lorinser J, Versteegh M, et al. Effects of storage time of red blood cell transfusions on the prognosis of coronary artery bypass graft patients. Transfusion. 2006;46:1712–8.
McKenny M, Ryan T, Tate H, et al. Age of transfused blood is not associated with increased postoperative adverse outcome after cardiac surgery. Br J Anaesth. 2011;106:643–9.
Sanders J, Patel S, Cooper J, et al. Red blood cell storage is associated with length of stay and renal complications after cardiac surgery. Transfusion. 2011;51(11):2286–94.
Koch CG, Li L, Duncan AI, et al. Transfusion in coronary artery bypass grafting is associated with reduced long-term survival. Ann Thorac Surg. 2006;81(5):1650–7.
Zimrin AB, Hess JR. Current issues relating to the transfusion of stored red blood cells. Vox Sang. 2009;96(2):93–103.
Dzik W. Fresh blood for everyone? Balancing availability and quality of stored RBCs. Transfus Med. 2008;18(4):260–5.
Hod EA, Brittenham GM, Billote GB, et al. Transfusion of human volunteers with older, stored red blood cells produces extravascular hemolysis and circulating non-transferrin-bound iron. Blood. 2011;118(25):6675–82.
Tinmouth A, Fergusson D, Yee IC, et al. Clinical consequences of red cell storage in the critically ill. Transfusion. 2006;46(11):2014–27.
Beckmann SR, Carlile D, Bissinger RC, et al. Improved coagulation and blood conservation in the golden hours after cardiopulmonary bypass. J Extra Corp Technol. 2007;39:103–8.
Takagi H, Manabe H, Kawai N, et al. Aprotinin increases mortality as compared with tranexamic acid in cardiac surgery: a meta-analysis of randomized head-to-head trials. Interact Cardiovasc Thorac Surg. 2009;9:98–101.
Raghunathan K, Connelly NR, Kanter GJ. ε-Aminocaproic acid and clinical value in cardiac anesthesia. J Cardiothorac Vasc Anesth. 2011;25:16–9.
Likosky DS, FitzGerald DC, Groom RC, et al. The effect of the perioperative blood transfusion and blood conservation in cardiac surgery Clinical Practice Guidelines of the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists upon clinical practices. J Extra Corp Technol. 2010;42:114–21.
Moskowitz DM, McCullough JN, Shander A, et al. The impact of blood conservation on outcomes in cardiac surgery: is it safe and effective? Ann Thorac Surg. 2010;90:451–8.
Wang G, Bainbridge D, Martin J, et al. The efficacy of an intraoperative cell saver during cardiac surgery: a meta-analysis of randomized trials. Anesth Analg. 2009;109:320–30.
Conflict of interests
None declared
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Haanschoten, M.C., van Straten, A.H.M., Verstappen, F. et al. Reducing the immediate availability of red blood cells in cardiac surgery, a single-centre experience. Neth Heart J 23, 28–32 (2015). https://doi.org/10.1007/s12471-014-0618-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-014-0618-9