Abstract
Aims
Follow-up studies of patients with cardiac syndrome X (CSX) generally report good prognosis. However, some recent studies report an adverse outcome for women.
Methods and results
Structured literature search and meta-analysis for studies regarding prognosis of cardiac syndrome X patients. We identified 85 studies, ultimately selecting 16 for inclusion. Meta-analysis yielded a pooled major cardiac event percentage of 1.5% per 5 years and a pooled vascular event percentage of 4.8% per 5 years (n = 16 studies, n = 1694 patients). Fourteen studies reported upon the recurrence rate of angina pectoris: the pooled percentage of angina recurrence was 55% (n = 1336 patients).
Conclusion
The present review of recent archival literature demonstrates an overall major cardiac event rate of 1.5% per 5 years. Although this is an excellent prognosis for CSX patients, the quality of life is impaired because of the high recurrence rate of angina pectoris (55%).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac syndrome X (CSX) is the syndrome of angina pectoris during a positive stress test despite a normal coronary arteriogram. CSX is an important clinical entity [1–19]. About 3–11% of patients undergoing coronary angiography because of typical chest pain have normal coronary arteries and qualify for the definition of CSX [19].
Follow-up studies of patients with CSX generally report good prognosis [7, 9]. However, a recent study reported an adverse cardiovascular outcome for women with chest pain and normal coronary arteries [6].
Therefore, the present paper reviews the recent literature on CSX to discuss in detail the long-term prognosis.
Methods of identifying and selecting the literature
A review and meta-analysis of the literature was conducted with a comprehensive search of the PubMed database to identify clinical studies on CSX that considered prognosis. The prognosis of CSX patients was derived from the cardiac event rate per year for each study and the recurrence rate of angina (when included in the studies).
Studies were eligible for review if they met the following standardised inclusion criteria [20–22]: Full-length articles; studies including CSX or patients with angina and normal coronary arteries; minimum number of 10 patients; studies presenting follow-up data of more than 2 years; and publication dates between April 1985 and February 2010.
The criteria for excluding studies were: metabolic syndrome X; studies including patients with near-normal coronary angiography (CAG) results; and studies of patients with myocardial infarction and/or cardiomyopathy were excluded.
In detail, the PubMed database was used to identify papers in which definitions and prognosis for CSX are described via the following terms:
‘((Prognosis or follow up) AND ((((cardiac syndrome x OR (angina pectoris AND normal coronary arteries) OR microvascular angina)) AND (((“microvascular angina”[TIAB] NOT Medline[SB]) OR “microvascular angina”[MeSH Terms] OR cardiac syndrome x[Text Word]))) AND ((“syndrome x”[All] OR (((angina pectoris) OR (chest pain)) AND normal AND (coronary[tw] OR angiogra*[tw])) OR (microvascular angina)))) AND ((Humans[Mesh]) AND (English[lang]) AND (adult[MeSH])))’; with limits set to English language and humans.
The search strategy identified 85 studies from PubMed. These became the source population for this review. The titles were screened for eligibility by one of the reviewers (I.V.), followed by two reviewers (I.V. and P.R.) independently assessing the abstracts by consensus. In this initial screening a total of 23 articles were excluded because of:
-
(a)
Metabolic syndrome X, myocardial infarction and tako-tsubo cardiomyopathy (14 references).
-
(b)
Non-performance of coronary angiography (2 references).
-
(c)
Studies with coronary spasm (3), case report (1), antiphospholipid syndrome (1) and non-obstructive coronary artery disease (2) in the title.
The titles of the remaining papers contained cardiac syndrome X (44 papers), normal coronary arteries (14 papers) and microvascular angina (4 papers).
The full texts of all 62 papers were retrieved for further selection, notably as to whether they considered prognosis. Only 17 included prognosis, but checking the references from all 17 resulted in another 4 papers being selected [1, 6, 12, 14]. Of these remaining 21 papers, 9 described CSX, 11 described AP and normal coronary arteries (NCA), and 1 described microvascular angina.
Finally, the 21 papers were independently surveyed by two authors (IV and PR) with respect to the definition of CSX and prognosis. This resulted in 5 papers being excluded as follows: an NCA study [23] also included minimal lesions of the coronary arteries with a reduction in diameter of less than 50%; one turned out to be only a letter [24]; 2 intervention studies did not report cardiac events [25, 26]; and another appeared to be an intervention study of only 7 patients [27], whereas the agreed minimum number of patients for our review was 10.
This survey left 16 papers for the present review. These papers covered a total of 1694 patients. For each paper we extracted the number of patients; cardiovascular event rates; percentage of female/male patients (for studies including both female and male patients); and the percentage of patients with recurrent chest pain. In more detail:
-
(1)
Major adverse cardiac event rates included cardiac death, myocardial infarction and revascularisation as defined by the most recent ACC/AHA guidelines 2010 and other studies [28–30].
-
(2)
The vascular events included myocardial infarction, cardiac death, development of CAD, heart failure, and the occurrence of cerebrovascular events.
-
(3)
Since some of the studies had different follow-up periods, we normalised the event rates to those per 5 years.
-
(4)
Before calculation of the pooled estimates of major cardiac event rates, cardiovascular event rates, chest pain recurrence rates and gender distribution, the heterogeneity of these values was tested using calculation of I2 and the Chi-square test. The effects of follow-up period, gender distribution and mean age of the populations upon the cardiovascular event rates were studied using regression analysis: P values < 0.05 were considered to be significant.
Results
Table 1 lists the 16 studies included in this review. Note that (a) 2 studies did not report the frequency of chest pain [3, 6], (b) the follow-up period varied widely, from 2.4 years to 14 years, and (c) 3 studies did not have male and female patients [1, 3, 6].
CSX prognosis
The three most important results relating to prognosis are:
-
(1)
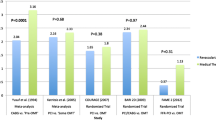
The major cardiac event rate varied from 0% to 3.8% per 5 years, with a pooled value of 1.5% per 5 years (95% CI: 1–2.2%, n = 1694 patients) (Fig. 1). There was no significant heterogeneity between included studies regarding the major cardiac event rate (p = 0.074). The estimated annual major cardiac event rate was 0.3%. This includes myocardial infarction, revascularisation and cardiovascular death (Table 1).
-
(2)
The general cardiovascular event rate varied from 0% to 16.7% per 5 years, with a pooled value of 4.8% for 5 years (95% CI: 3.8–5.9%). However, there was significant heterogeneity (p < 0.001) (Fig. 2).
-
(3)
There were 14 studies with 1336 patients for analysis of recurrent chest pain. The recurrence rate varied between 13.2% and 89.9% for the different study populations, with a pooled value of 55% (95% CI: 53–58%, n = 1336 patients). There was significant heterogeneity (p < 0.001) (Fig. 3).
The remaining results are:
-
(4)
The major cardiac event rate was not related to the length of follow-up (R2 = 0.0043), mean age (R2 = 0.000006) and percentage of female patients (R2 = 0.0268).
-
(5)
The total vascular cardiac event rate per study was not related to the length of follow-up (R2 =0.0011), mean age (R2 = 0.238) and percentage of female patients (R2 = 0.063).
Discussion
Overall cardiac event rates
This systematic review shows that the CSX prognosis in terms of the overall cardiac event rate is excellent, with a risk of myocardial infarction or cardiovascular death of 1.5% per 5 years. The Framingham Heart Study reported annual hard (death, myocardial infarction) coronary event rates of 1.2% (men < 65 years); 2.7% (men > 65 years); 0.5% (women < 65 years); and 1.6% (women > 65 years). These rates are all higher than the major adverse cardiac event rate for CSX patients determined from our systematic review.
The lower cardiac event rates for CSX patients suggest that they may benefit from protective factors against coronary macrovascular disease. These factors could be (a) cardioprotective medication, (b) a healthier lifestyle to avoid angina and myocardial infarction, e.g. becoming non-smokers, and (c) another biological mechanism. A possible example of the last mentioned is the observation that platelet reactivity decreases after stress in patients with CSX, in contrast to patients with coronary artery disease (CAD) [31, 32]. On the other hand, the better prognosis of CSX patients compared with the general population may result from a selection process. CSX patients all have, by definition, normal coronary arteries, which is not necessarily the case in the general population. The difference in prevalence of coronary atherosclerosis between CSX patients and the general population may explain the difference in cardiac event rates.
The notion of the benign nature of CSX has been challenged by reports of a high risk of future cardiac events in patients with angina and normal coronary arteries [1, 33, 34]. A recent study, named the Women’s Ischaemia Syndrome Evaluation (WISE) study, involved 540 symptomatic women referred for coronary angiography and followed up for a mean of 5.2 years. The control group was asymptomatic, and consisted of community-based age- and race-matched women with no history of heart disease, and who were followed up for 10 years.
The WISE study showed a cardiovascular event rate of 7.9% per 5 years for women with angina and normal coronary arteries (CSX), compared with 2.4% per 5 years for the asymptomatic control group [6]. The WISE study CSX event rate lies outside the 95% confidence interval of 3.8%–5.9% per 5 years that we found from our reviewed studies.
However, the rate of cardiovascular death was not significantly different between the CSX women and the control (asymptomatic) women in the WISE study. The increased cardiovascular event rate in symptomatic women with normal coronary arteries was largely accounted for by an increased incidence of hospitalisation for heart failure and stroke. It remains unexplained why the incidence of heart failure and stroke are increased in this specific population, although microvascular dysfunction might precede macrovascular atherosclerosis.
CSX and non-obstructive CAD cardiac event rates
It is important to distinguish between CSX, with normal coronary arteries, and non-obstructive CAD [19]. The cardiac event rate for CSX patients is significantly better than that for patients with angina and non-obstructive CAD. This is illustrated by Sicari et al. [35], who reported that a subgroup of patients with angina and non-obstructive CAD (incorrectly identified as CSX), and with positive dipyridamole echocardiography tests, had a survival rate of only 76% after 7.1 years follow-up.
Five-year cardiac event rates for cardiovascular events were significantly different for three subgroups in the WISE study: 16% per 5 years for women with angina and non-obstructive CAD (stenosis <50%); 7.9% per 5 years for women with angina and normal coronary arteries (CSX); and 2.4% per 5 years for the asymptomatic control group (P ≤ 0.002) [6]. Hence, in this large study a higher incidence of events in symptomatic women with non-obstructed CAD was found compared with patients with symptoms and normal coronary arteries.
CSX and coronary microvascular dysfunction
Lanza and Crea recently proposed to rename CSX as stable primary coronary microvascular dysfunction (CMVD) [36]. This proposal was made on the premise that abnormalities in the coronary microcirculation are the probable cause of CSX ischaemia and angina. However, Herzog obtained contemporary positron emission tomography (PET) data that suggest an increased cardiac event rate for patients with microvascular dysfunction, irrespective of abnormalities in the epicardial coronary arteries [37]. (Note: this study was not included in our literature review because CAGs were not performed.)
In the study by Herzog the patients with a reduced flow reserve, defined as a CFR < 2.0, had a higher annual cardiac event rate and a higher risk of cardiac death, and this included patients with a normal perfusion PET [37]. Specifically, a subgroup of patients with normal perfusion but impaired CFR had a significantly higher major annual cardiac event rate (6.25%) compared with patients with a normal CFR (1.4%). Also, the annual cardiac death rate was higher: 3.1% for patients with normal perfusion but impaired CFR, compared with 0.5% for patients with normal CFR. Thus it is possible for patients with a normal perfusion, who are therefore unlikely to have epicardial coronary obstructive disease, to already have a reduced CFR, and that this is associated with a higher cardiac event rate or higher risk of cardiac death. The reduced CFR was most likely caused by microvascular or endothelial dysfunction [37]. Therefore one should be cautious about equating CSX (which has a generally good prognosis) with coronary microvascular dysfunction.
Limitations to the significance of the study by Herzog et al. are (a) the relatively small number of patients in the subgroup with normal perfusion and impaired CFR (n = 32), and (b) that after 10 years follow-up the impaired CFR could not predict any cardiac event in this subgroup [37]. Hence larger prospective studies are needed. Be that as it may, we may conclude that a distinguishing diagnosis between CSX and CMVD requires evaluation of the distal compartment (intramural arterioles) as well as the proximal compartment (the large epicardial coronary arteries).
Recurring chest pain
As stated earlier, recurrence of chest pain occurred in an average of 55% of the CSX cases included in our systematic review. In the study by Lantinga et al., 85% had at least weekly episodes of chest pain up to 1 year after the angiograms, with the pain unchanged or even worse; and 33% underwent at least one more coronary angiography [38].
The most important therapy consists of reassurance, risk factor modification, and symptom relief (ACC/AHA guidelines 2002, www.acc.org/qualityandscience/clinical/statements.htm). There are conflicting data about the exact cause of chest pain in patients with CSX, There is evidence for ischaemia [17, 39], and alternatively, psychological factors such as an increased anxiety may play a role in CSX [18]. The number of pain episodes can be reduced by β-blockers, calcium antagonists, nitrates and imipramine, which is particularly successful [40]. Similar success has been claimed for oestrogen replacement therapy [41, 42]. In a patient with coronary spasms we found an increase of the myocardial blood flow and decrease of symptoms using bosentan, an endothelin receptor antagonist [43]. However, the therapeutic measures remain largely empirical, and the symptoms persist in many patients.
Limitations
Systematic reviews are hampered by publication bias, i.e., the preferential publication of studies with significant positive results rather than those with negative results. However, in studies regarding prognosis and survival this phenomenon is probably less frequent compared with studies evaluating therapeutic strategies.
Another potential problem is that clinical prognostic studies are almost inevitably different in their length of follow-up, which can affect the study results because longer follow-up periods might yield more exact prognostic figures. However, in our review we found no relation between the length of follow-up and event rates.
There are possible limitations owing to varying inclusion criteria for the different studies. These variations can cause heterogeneous meta-analysis results. For example, we found in earlier work that there were more than 50 different criteria (nine different inclusion criteria and 43 different exclusion criteria) for CSX, resulting in a varying reported incidence of CSX [19]. Also, the heterogeneity of the different study populations may have contributed to the heterogeneity that we found with respect to the prognoses from the studies.
On the other hand, the advantages of reviews and meta-analyses are an increase in statistical power, the ability to assess sources of heterogeneity, and the provision of overall estimates of prognostic variables.
Conclusions
The present review found an overall major adverse cardiac event rate of 1.5% per 5 years. This represents a better prognosis compared with the general population. However, angina pectoris in CSX is recurrent and persistent in 55% of the patients, and significantly impairs the quality of life.
Whether CSX patients benefit from protective factors against acute coronary events is a challenging issue that should be addressed in future studies.
References
Bugiardini R, Manfrini O, Pizzi C, et al. Endothelial function predicts future development of coronary artery disease: a study of women with chest pain and normal coronary angiograms. Circulation. 2004;109(21):2518–23.
Chauhan A, Mullins PA, Thuraisingham SI, et al. Clinical presentation and functional prognosis in syndrome X. Br Heart J. 1993;70(4):346–51.
Delcour KS, Khaja A, Chockalingam A, et al. Outcomes in patients with abnormal myocardial perfusion imaging and normal coronary angiogram. Angiology. 2009;60(3):318–21.
Foussas SG, Adamopoulou EN, Kafaltis NA, et al. Clinical characteristics and follow-up of patients with chest pain and normal coronary arteries. Angiology. 1998;49(5):349–54.
Fragasso G, Chierchia SL, Arioli F, et al. Coronary slow-flow causing transient myocardial hypoperfusion in patients with cardiac syndrome X: long-term clinical and functional prognosis. Int J Cardiol. 2009;137(2):137–44.
Gulati M, Cooper-DeHoff RM, McClure C, et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the Women’s Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch Intern Med. 2009;169(9):843–50.
Kaski JC, Rosano GM, Collins P, et al. Cardiac syndrome X: clinical characteristics and left ventricular function. Long-term follow-up study. J Am Coll Cardiol. 1995;25(4):807–14.
Lamendola P, Lanza GA, Spinelli A, et al. Long-term prognosis of patients with cardiac syndrome X. Int J Cardiol. 2010;140(2):197–9.
Leu HB, Lin CP, Lin WT, et al. Circulating mononuclear superoxide production and inflammatory markers for long-term prognosis in patients with cardiac syndrome X. Free Radic Biol Med. 2006;40(6):983–91.
Lichtlen PR, Bargheer K, Wenzlaff P. Long-term prognosis of patients with anginalike chest pain and normal coronary angiographic findings. J Am Coll Cardiol. 1995;25(5):1013–8.
Radice M, Giudici V, Marinelli G. Long-term follow-up in patients with positive exercise test and angiographically normal coronary arteries (syndrome X). Am J Cardiol. 1995;75(8):620–1.
Scholz M, Wegener K, Unverdorben M, et al. Long-term outcome in patients with angina-like chest pain and normal coronary angiograms. Herz. 2003;28(5):413–20.
Shintani S, Nishiyama Y, Yamamoto K, et al. Different long-term course between chest pain and exercise-induced ST depression in syndrome X. Jpn Heart J. 2003;44(4):471–9.
Sullivan AK, Holdright DR, Wright CA, et al. Chest pain in women: clinical, investigative, and prognostic features. BMJ. 1994;308(6933):883–6.
Sun SS, Huang JL, Tsai SC, et al. The higher likelihood of developing cardiomegaly during follow-up in patients with syndrome X and abnormal thallium-201 myocardial perfusion SPECT. Int J Cardiovasc Imaging. 2001;17(4):271–8.
Suzuki H, Matsubara H, Koba S, et al. Clinical characteristics and follow-up in patients with microvascular angina. Circ J. 2002;66(7):691–5.
Vermeltfoort IA, Bondarenko O, Raijmakers PG, et al. Is subendocardial ischaemia present in patients with chest pain and normal coronary angiograms? A cardiovascular MR study. Eur Heart J. 2007;28(13):1554–8.
Vermeltfoort IA, Raijmakers PG, Odekerken DA, et al. Association between anxiety disorder and the extent of ischemia observed in cardiac syndrome X. J Nucl Cardiol. 2009;16(3):405–10.
Vermeltfoort IA, Raijmakers PG, Riphagen II, et al. Definitions and incidence of cardiac syndrome X: review and analysis of clinical data. Clin Res Cardiol. 2010;99(8):475–81.
Mijnhout GS, Riphagen II, Hoekstra OS. Update of the FDG PET search strategy. Nucl Med Commun. 2004;25(12):1187–9.
Raijmakers PG, Paul MA, Lips P. Sentinel node detection in patients with thyroid carcinoma: a meta-analysis. World J Surg. 2008;32(9):1961–7.
Temmerman OP, Raijmakers PG, Berkhof J, et al. Accuracy of diagnostic imaging techniques in the diagnosis of aseptic loosening of the femoral component of a hip prosthesis: a meta-analysis. J Bone Joint Surg Br. 2005;87(6):781–5.
Juelsgaard P, Ronnow Sand NP. Somatic and social prognosis of patients with angina pectoris and normal coronary arteriography: a follow-up study. Int J Cardiol. 1993;39(1):49–57.
Kronhaus KD, Lawson WE. Enhanced external counterpulsation is an effective treatment for Syndrome X. Int J Cardiol. 2009;135(2):256–7.
de Vries J, Dejongste MJ, Durenkamp A, et al. The sustained benefits of long-term neurostimulation in patients with refractory chest pain and normal coronary arteries. Eur J Pain. 2007;11(3):360–5.
Sgueglia GA, Sestito A, Spinelli A, et al. Long-term follow-up of patients with cardiac syndrome X treated by spinal cord stimulation. Heart. 2007;93(5):591–7.
Lanza GA, Sestito A, Sandric S, et al. Spinal cord stimulation in patients with refractory anginal pain and normal coronary arteries. Ital Heart J. 2001;2(1):25–30.
Haude M, Baumgart D, Verna E, et al. Intracoronary Doppler- and quantitative coronary angiography-derived predictors of major adverse cardiac events after stent implantation. Circulation. 2001;103(9):1212–7.
Holmes Jr DR, Dehmer GJ, Kaul S, et al. ACCF/AHA clopidogrel clinical alert: approaches to the FDA “boxed warning”: a report of the American College of Cardiology Foundation Task Force on clinical expert consensus documents and the American Heart Association endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2010;56(4):321–41.
Lindsay Jr J, Pinnow EE, Pichard AD. Frequency of major adverse cardiac events within 1 month of coronary angioplasty: a useful measure of operator performance. J Am Coll Cardiol. 1999;34(7):1916–23.
Lanza GA, Sestito A, Iacovella S, et al. Relation between platelet response to exercise and coronary angiographic findings in patients with effort angina. Circulation. 2003;107(10):1378–82.
Sestito A, Maccallini A, Sgueglia GA, et al. Platelet reactivity in response to mental stress in syndrome X and in stable or unstable coronary artery disease. Thromb Res. 2005;116(1):25–31.
Britten MB, Zeiher AM, Schachinger V. Microvascular dysfunction in angiographically normal or mildly diseased coronary arteries predicts adverse cardiovascular long-term outcome. Coron Artery Dis. 2004;15(5):259–64.
Johnson BD, Shaw LJ, Buchthal SD, et al. Prognosis in women with myocardial ischemia in the absence of obstructive coronary disease: results from the National Institutes of Health-National Heart, Lung, and Blood Institute-Sponsored Women’s Ischemia Syndrome Evaluation (WISE). Circulation. 2004;109(24):2993–9.
Sicari R, Palinkas A, Pasanisi EG, et al. Long-term survival of patients with chest pain syndrome and angiographically normal or near-normal coronary arteries: the additional prognostic value of dipyridamole echocardiography test (DET). Eur Heart J. 2005;26(20):2136–41.
Lanza GA, Crea F. Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation. 2010;121(21):2317–25.
Herzog BA, Husmann L, Valenta I, et al. Long-term prognostic value of 13 N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J Am Coll Cardiol. 2009;54(2):150–6.
Lantinga LJ, Sprafkin RP, McCroskery JH, et al. One-year psychosocial follow-up of patients with chest pain and angiographically normal coronary arteries. Am J Cardiol. 1988;62(4):209–13.
Lanza GA, Buffon A, Sestito A, et al. Relation between stress-induced myocardial perfusion defects on cardiovascular magnetic resonance and coronary microvascular dysfunction in patients with cardiac syndrome X. J Am Coll Cardiol. 2008;51(4):466–72.
Cannon III RO, Quyyumi AA, Mincemoyer R, et al. Imipramine in patients with chest pain despite normal coronary angiograms. N Engl J Med. 1994;330(20):1411–7.
Rosano GM, Collins P, Kaski JC, et al. Syndrome X in women is associated with oestrogen deficiency. Eur Heart J. 1995;16(5):610–4.
Rosano GM, Peters NS, Lefroy D, et al. 17-beta-Estradiol therapy lessens angina in postmenopausal women with syndrome X. J Am Coll Cardiol. 1996;28(6):1500–5.
Vermeltfoort IA, Raijmakers PG, Kamphuisen PW. Improved myocardial perfusion preceding clinical response on bosentan treatment for coronary vasospasm. Acta Cardiol. 2009;64(3):415–7.
Acknowledgements
We thank Dr R.J.H. Wanhill PhD and Dr J. Bax PhD for their critical review and editing of the manuscript.
Conflict of interest
None declared
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Vermeltfoort, I.A.C., Teule, G.J.J., van Dijk, A.B. et al. Long-term prognosis of patients with cardiac syndrome X: a review. Neth Heart J 20, 365–371 (2012). https://doi.org/10.1007/s12471-012-0256-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-012-0256-z