Abstract
Donor milk from the human milk bank is important for vulnerable infants without their mothers’ own milk. Longitudinal changes in toxic metals in donor milk has not been reported. This study aimed to assess the effect of donors’ demographic characteristics, life habits and dietary habits on the concentration of metals in breastmilk donated to a human milk bank and to assess the health risk of lead (Pb) and mercury (Hg) exposure of donor mothers’ offspring through breastfeeding and the vulnerable recipients. A total of 228 samples, which were longitudinally donated to the human milk bank by 39 donors, were selected specifically to assess the levels of Pb, Hg, and MeHg. Donors’ offspring were also enrolled as mother-infant-dyads to monthly obtain the milk consumption and body weight. The results showed significant differences in the infant risk in exclusive breastfeeding months. The average Pb level of breast milk was 6.49 ± 5.23 µg/L (mean ± standard deviation), and the Hg level was 0.76 ± 0.98 µg/L. The sources of these toxins—residential districts, cleaning products, cosmetics, drinking water, viscera, eggs, seafood, and canned food—have a significant influence on the concentration of toxic metals in human milk. This study showed an unacceptable non-cancerous health risk (95th percentile hazard index, HI = 1.37 > 1) for Pb and Hg. In the future, the breast milk offered by the bank should be strictly monitored, especial for Pb, to ensure high-quality donor milk for vulnerable recipients but also donor mothers’ offspring who depend on it.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human milk has been recognized as the main source of nutrition for infants (Agostoni et al. 2010; Tudehope 2013; de Halleux et al. 2017) because of its abundant nutritional content: energetic macronutrients and fatty acids (Grote et al. 2016), bioactive content, important enzymes (Khaldi et al. 2014), antimicrobial and anti-inflammatory properties (Laiho et al. 2003; Lepage and Perre 2012), and docosahexaenoic (omega-3 fatty) acid (Affinito et al. 1996). The antibodies (Lepage and Perre 2012; Rogier et al. 2014; Sherry et al. 2015; Marangoni et al. 2016) in human milk reduce the risk of diseases, such as necrotizing enterocolitis (Zhou et al. 2015; Buckle and Taylor 2017; Pammi and Suresh 2017), nosocomial infections, sepsis (Cortez et al. 2018), lung disease (Villamor-Martinez et al. 2018), severe diarrhea, otitis media, and respiratory infections (Comite de nutrition de la Societe francaise de et al. 2013). In addition, human milk has been linked with long-term health conditions, such as decreased susceptibility to allergies and obesity (Admyre et al. 2007; Newburg et al. 2010; Crume et al. 2011). Human milk consumption is associated with improved neurodevelopmental outcomes in vulnerable infants (Lucas et al. 1992; Stefanescu et al. 2016; Cortez et al. 2018).
For Taiwanese infants, breastfeeding has been promoted by the Health Promotion Administration (HPA), Ministry of Health and Welfare since 2001 (Taiwan-Health-Promotion-Administration 2015). The HPA reported that the exclusive breastfeeding rate 1 month after birth rose dramatically from 5.4% in 1989 to 61.8% in 2011, when 24.2% of 6-month postpartum women reported exclusive breastfeeding (Taiwan-Health-Promotion-Administration 2012). As for exclusive breastfeeding rate, 40.1% of Taiwanese mothers reported exclusive breastfeeding at 1 month and 29.3% at 2 months postpartum (Chang et al. 2019). According to a 2016 telephone interview in Taiwan by the HPA, the breast milk feeding rate for infants under 4 months was more than 50% and 44.8% for infants under 6 months, which is comparable to the 41% recorded in the global database (MOHW-HPA 2019).
Although the advantages associated with breastfeeding are well known, heavy metal toxicity in human milk has received increased research attention (Chao et al. 2014; Jeong et al. 2017; Dix-Cooper and Kosatsky 2018; Vahidinia et al. 2019). Mining, battery manufacturing, drinking water tubes, paint, makeup, and other consumer products are sources of Pb exposure (Nriagu et al. 1996; Piomelli 2002; Cardoso et al. 2014); heavy metals can also be found in the soil, water, air, and the food chain. The concentrations of toxic and trace metals are higher in pig and cattle verscera than in the muscle (Niemi et al. 1991; Sedki et al. 2003; Akan et al. 2010). The postpartum confinement is popular in many cultures, especially in traditional Chinese culture worldwide (Dennis et al. 2007). Including Taiwan, dietary pattern of Chinese-style postpartum confinement provides pig liver, pig kidney, fish, sea food, and chicken heart etc. to postpartum mothers during the confinement month after childbirth. As mentioned, those foods make women exposed to heavy metals. If Pb and Hg, which are both regarded as neurotoxicants, accumulate in human breast milk (Braun et al. 2008; Díez 2009; Caserta et al. 2013; Kvestad et al. 2018), they will be passed down to infants (Sowers et al. 2002; Park et al. 2018).
Attention should be given to the metal effects on children for several reasons. First, their tolerance for toxins is lower than that of adults (Needleman 2004). Second, maternal prenatal nutrition and a child's nutrition during the first 2 years are crucial for healthy neurodevelopment and lifelong mental health (Al-Saleh et al. 2016; Schwarzenberg and Georgieff 2018). Therefore, low levels of Pb and methylmercury (MeHg) exposure from breastfeeding can pass through the blood–brain barrier and cause neurological and developmental disorders (Chien et al. 2006; Díez 2009; Kern et al. 2020).
Considerable research reported heavy metal inspections in foodstuffs. In Algeria, the levels of Pb in 15 fruits and vegetables measured 12.33–39.33 mg/kg dry weight, and several values exceeded the international threshold. The estimated daily intake (EDI) and total hazard quotient (HQ) were also all higher than the thresholds set by the Food and Agriculture Organization and World Health Organization (FAO/WHO) (Cherfi et al. 2014). In Uganda, measurements of Pb levels in beef, mutton, chicken, and their viscera showed levels ranging from 0.04 to 1.11 mg/kg, which were higher than the suggested level (0.5 mg/kg wet weight) set by the European Food Safety Authority. Moreover, the risk assessment showed that the HQ was above 1 for sheep intestines and beef liver, kidney, and lung, whereas the HQ of 0.99 was detected for chicken liver (Ogwok et al. 2020). Burger et al. measured arsenic (As), cadmium (Cd), chromium (Cr), Pb, manganese (Mn), Hg, and selenium (Se) levels, and although the average Hg level in all fish did not exceed the 1.0 ppm limit set by the Taiwan Food and Drug Administration (FDA), the 18% Hg level in tuna did. Furthermore, the Pb levels in shellfish and shrimp exceeded the Codex Alimentarius Commission suggestion of 0.2 ppm (Burger and Gochfeld 2004, 2005). In Taiwan, regarding the measurement of Cd, Pb and Hg in 1939 foodstuffs, only Pb levels in one chickpea exceeded 0.2 µg/g, whereas the Cd level in one shellfish exceeded the 2 µg/g set by the FDA (Lee et al. 2018). Although numerous studies have reported metals levels in foodstuff, the measurements of toxic metals in breast milk are still limited (Iwai-Shimada et al. 2015; Al-Saleh et al. 2016; Vollset et al. 2019), especially for longitudinal measurement on the breast milk donated to the human milk bank.
The study sought to determine whether the demographic characteristics, life habits and dietary pattern of breastfeeding mothers is related to the accumulation of Pb, Hg, and MeHg in their breast milk, and to assess the health risk of Pb and Hg exposure of the offspring and recipients through breast milk. Finally, further to evaluate whether these metals should be measured before the milk is donated.
Materials and Methods
Subject Enrollment
This study was approved by the Ethics Committee of the National Cheng Kung Hospital (Tainan, Taiwan, encoded: A-ER-108-193). The study was conducted at the Taiwan Southern Human Milk Bank (TSHMB) of National Cheng Kung University Hospital, the second human milk bank in Taiwan. TSHMB is a non-profit unit supported by HPA Taiwan. The operation of the TSHMB is similar to that of the first bank in Taiwan (Chang et al. 2013) and other banks worldwide (Moro et al. 2019). One local rule of the TSHMB is that the donor must make contact within 3 months postpartum and be willing to cooperate with a long-term donation. Single-batch donations are not allowed. All participants must prove to have a healthy medical history and have their blood tested for infectious diseases, including hepatitis A, B, and C virus, human immunodeficiency virus, Human T-lymphotropic virus, and cytomegalovirus. The cost of tests is supported by TSHMB. All participants are volunteers without incentive payments and commit to donate long-term. After receiving certificated of blood test report, donors are supplied with sterile glass bottles. Expressed or pumped milk was collected and refrigerated by donors immediately. A staff from the TSHMB visits the donors once a week to bring the frozen milk back for processing and pasteurization. Under a friendly support system, qualified donors can donate breast milk by their will without time limitation but maximally up to 9 months postpartum (Chen et al. 2022).
When donor mother contacted the TSHMB by themselves through the internet to donate breast milk, mother-infants-dyads were prospectively invited to this study, and consent was obtained before the first donation. The exclusion criteria were that the delivery could not be a multiple-gestation and the participants did not live adjacent to, or have an occupation related to, a smelter or metal recycling plant (radius < 1 km).
Of 41 lactating women, 39 mothers aged 20–40 years old were recruited. Two dyads were excluded for the non-qualified of breast milk or temporary donation. The mothers filled out a background information questionnaire in their demographic, age, occupation, education, life habits (smoking, exercising, and cosmetic or perfume usage), residential environment, outdoor activities, type of drinking water, and eating frequency and quantity. For dietary intake, oil, viscera, milk, fish, and seafood intake were all recorded separately categories based on Taiwan National Food Consumption Database. For each dyads, the monthly body weights and estimated daily milk volume of infants were obtained from the mothers by the telephone visits. Using the information from mother-infant-dyads, exposures for vulnerable recipients of donor milk would be further estimated.
Samples Collection and Metal Measurement
One additional tube of a participant’s blood was taken during the required TSHMB blood tests when donors joined the donation. One milliliter (mL) of venous blood from each participant was stored at − 20 °C for metals analysis.
Participants’ breast milk was collected every 1–2 weeks from their first donation and maximally up to 9 months. The staff of the TSHMB helped to obtain samples for further analysis during the handling unpasteurized donor milk. Fifteen mL of breast milk were collected in glass bottles and stored at − 20 °C before metals analysis. The body weight and daily breast milk consumption of infants were also reported from their mother along with each breast milk sampling for calculating the health risk for those infants from breast milk consumption. As well, the changes in food intake of lactating women and breast milk feeding of infants were also recorded at each sampling time.
During the analysis, the breast milk was thawed at 4 °C, heated to 40 °C, and shaken for homogeneity. Then, 1.5 mL 67% HNO3 was added to 500 μL of breast milk, and 2.5 mL 67% HNO3 was added to 250 μL of blood, which were adopted from the analysis method for metals in beverages and dairy food, reported from Taiwan FDA (MOHWH0023.00) (TFDA 2020).
The Pb levels in the milk and blood samples were measured by inductively coupled plasma mass spectrometry (ICP–MS, Nexion 2000, PerkinElmer) (MOHWH0023.00) (TFDA 2020).
The Hg concentrations were analyzed by an automatic mercury analyzer (MA-2000), and the method was modified from Hg in solids and solutions by thermal decomposition, amalgamation, and atomic absorption spectrophotometry (USEPA 7473), respectively. The breast milk was de-freeze at 40 °C water bath for reducing the delamination of fat from liquid. Then 100 µL was obtained for Hg analysis by automatic mercury analyzer.
The MeHg levels were measured by liquid chromatograph/inductively coupled plasma mass spectrometry (LC/ICP–MS, Nexion 2000, PerkinElmer), which were adopted from the analysis method for MeHg in foodstuff, reported from Taiwan FDA (MOHWH0018.00). The accuracy of the analysis and instrumentation were validated using certified reference materials from the PerkinElmer Pure Plus NexION Setup solution (Lot#32-13GSX1).
The recovery efficiency tests for Pb, Hg, and MeHg were conducted using the same sample analysis procedure but with the addition of a standard solution. In the current study, recovery rates were respectively 103%, 109%, and 89% for Pb, Hg, and MeHg in breast milk and 108% and 93% for Pb and Hg in blood. The method detection limit (MDL) was shown using a concentration slightly lower than the lowest concentration of the calibration curve. Measurements at this concentration were repeated seven times to estimate the standard deviation, and the MDL was set at a 3-time standard deviation. The MDLs for Pb, Hg, and MeHg in breast milk were 0.047, 0.132, and 0.082 μg/L, respectively, and for Pb, Hg in the blood it was 0.230 and 0.132 μg/L.
Exposure Measurement and Risk Characteristics
Due to the breast milk will be donated to TSHMB for vulnerable recipients, the exposure and risk assessment was processed based on the donor mothers and their infant dyads for assessing their consumption safety of breast milk. Estimated breast milk consumption and body weight (BW) of infants in each dyads were provided by mother during monthly interviews. This data was provided for calculating the estimated daily intake (EDI) of dietary exposure to toxic metals from breast milk consumption for infants in each dyads. The hazard quotient (HQ) of Pb was calculated based on the BMDL01 (0.5 µg/kg·BW/day), set by EFSA in 2010. The HQ for Hg was calculated based on the PTWI (4 µg/kg·BW/week), set by the WHO in 2011. The EDI, HQ and hazard index (HI) risks are expressed by the following equations:
In addition, the HI can be calculated as the sum of the individual HQ of metals based on their reproductive effects. An HQ or HI < 1 indicated that the daily exposure dose may not cause adverse health effects and vice versa.
The Monte Carlo method is a probabilistic distribution function that characterizes the parameters used in estimating daily doses and risks. Sensitivity analysis was used to illustrate and rank variation in input variables based on their relative contributions to model output variability and uncertainty (US EPA 2001). The correlation coefficient (r) measures the strength and direction of the linear association between the values of two quantitative variables. If the model output variable (e.g., HI) and input variable are highly correlated, it means that the output is sensitive to that input variable. By squaring the coefficient, the result can be expressed as a percentage contribution to the variance of the output. The Monte Carlo simulation used @Risk 7.5.1 (Palisade Corp., Ithaca, NY, USA).
Results
The average age of the 39 lactating women in the study was 33.1 years, and no smokers or nor drinkers (Table 1). Twenty-one lived near the potential sources of air pollution, including traffic, industrial pollution, a night market, or a temple. Thirteen (33%) subjects reported using incense, and 18 (46%) used cosmetics frequently.
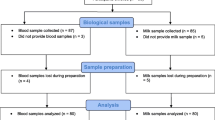
Figure S1 shows the numbers of samples in each postpartum month. A total of 228 breast milk samples were obtained from the donors, and the distribution of metal concentration is shown in Table 2. The average Pb level of breast milk was 6.49 µg/L (standard deviation: 5.23 µg/L), and the Hg level was 0.76 µg/L (0.98 µg/L).
A mother who lived within 1 km of traffic, industrial pollution, night markets or temple incense had significantly higher Pb levels than the other mothers (mean Pb level 10.30 µg/L vs. 5.49 µg/L; p = 0.025) (Table 3). A significantly higher average of Pb level was also found in mothers exposed to house dust without wearing a mask, and who used cosmetics and lipstick (9.43, 9.23, and 10.90 µg/L, respectively) than those who did not (5.06, 4.82, and 4.85 µg/L).
A significant difference in the Pb levels of breast milk was found among lactating mothers who did or did not consume viscera (10.20 vs. 4.54 µg/L, respectively, p < 0.001). A significantly higher Pb level was found in those who ate the eggs (9.08 vs. 5.46 µg/L), shellfish (7.39 vs. 6.59 µg/L), and canned food (8.01 vs. 5.30 µg/L) than those who did not (Table 4). Similarly, for Hg levels, a significant difference was found among those who ate the viscera (0.84 vs. 0.57 µg/L, p = 0.043), shellfish (0.77 vs. 0.59 µg/L), large sea fish (1.11 vs. 0.62 µg/L), and cephalopods (0.79 vs. 0.58 µg/L) than those who did not consume (p < 0.05 for all).
A significant difference in Pb levels was also observed among lactating women who drank only tap water (18.3 µg/L), tap water plus reverse osmosis water or bottled water (6.95 µg/L), or water without any tap water (5.30 µg/L).
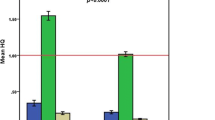
The average infant EDIs of Pb were 0.628 and 0.069 ng/kg·body weight (BW)/day of Hg (Table 5). The exact values for 50% HQ for Pb and Hg exposure were 0.989 and 0.097, respectively, and the total HI for Pb and Hg was more than 1. Meanwhile, 95% of the upper limit of HQ was 3.782 for Pb and 0.326 for Hg exposure. According to the monthly measurements of Pb and Hg levels in breast milk, significant differences in EDI and HQ for Pb and Hg exposure were found each month (p < 0.05, separately) (Table S1).
The decreasing trend of EDI and HQ of Hg and Pb exposure was found by their delivery month, and such finding may be due to the increase in infant BW. However, the HQs of Pb (Fig. 1a) in M1–M9 were higher than 1, and that of Hg (Fig. 1b) in M1–M4 was higher than 0.5. If the total HQs of Pb and Hg were summarized at 4 months after delivery, the HIs before month 4 were all higher than 1, and the most predominant risk contributor was Pb (Figs. S2 and S3).
The results of sensitivity analysis showed that the most influential variables in HI were the concentration of Pb in breast milk (52.8%) and the amount ingested by infants (34.2%) (Fig. S2). In addition, the literature cites environmental pollution sources, mask wearing while performing household cleaning, amalgam fillings, cosmetic usage, drinking water, and consumption of viscera and canned food as important factors.
Discussion
Pb and Hg Concentrations in Breast Milk
When comparing the Pb and Hg levels with other studies (Table 6), the results of the current study were similar to those found in Korea (8.79 µg/L vs. 0.94 µg/L) (Park et al. 2018). The Pb level was higher than those found in Austria (1.63 µg/L), Greece (0.48 µg/L), and Norway (0.2 µg/L) (Gundacker et al. 2002; Leotsinidis et al. 2005; Vollset et al. 2019), but lower than those in Spain (15.56 µg/L) (García-Esquinas et al. 2011), Lebanon (18.17 µg/L), and Iran (median: 41.9 µg/L) (Bassil et al. 2018; Samiee et al. 2019). The Hg level in the current study was comparable to those of other research (García-Esquinas et al. 2011; Iwai-Shimada et al. 2015; Al-Saleh et al. 2016; Vollset et al. 2019), but considerably lower than that in Austria (Gundacker et al. 2002). The MeHg level was not detected in all breastmilk samples.
Habit Factors Influence Metal Concentration in Breast Milk
In this study, we identified several life habit factors, including living place, cosmetic usage, and lipstick usage, which may be related to the increased levels of the studied metals (Table 3). Given that particulate matter inside a house may contain Pb from paint or furniture covering, lactating mothers may inhale them while doing housework if they do not wear a mask (Khanjani et al. 2018). Meanwhile, they still need to go out to shop or work, but such variable was not considered in this study. Feizi et al. (2019) indicated that high Pb concentrations were found in lipstick and eye pencil; thus, childhood Pb poisoning from breast milk poses a concern (Hon et al. 2017). Moreover, a positive association between dental amalgam fillings and the risk of Hg exposure has been proven in other research (Norouzi et al. 2012; Grzunov LetiniĿ et al. 2016; Vollset et al. 2019), but clinically strong evidence is still limited (FDA 2017). Although the Hg level was high in lactating women who had amalgam fillings, it was not statistically significant.
Metal Concentration in Breast Milk Under Different Dietary Intake Patterns
We observed several dietary sources associated with metal concentration. These results are similar to those from previous studies regarding the positive relationship between Hg levels in breast milk and the consumption frequency of fish, shrimp, crab and other shellfish (Gaxiola-Robles et al. 2014; Grzunov LetiniĿ et al. 2016; Vollset et al. 2019). Moreover, other studies suggested that different canned food, especially fruit, may contain a contaminant (Al Zabadi et al. 2018; Fathabad et al. 2018).
A significant difference in Pb levels was also detected among lactating women who drank only tap water (18.3 µg/L), tap water plus reverse osmosis water or bottled water (6.95 µg/L), or water without any tap water (5.30 µg/L). The result was consistent with that of Cardoso et al. (2014), who indicated that drinking water is an important pathway for metal exposure through breast milk based on observations of similar profiles.
Estimating Exposure of Infants to Metals from Breast Milk
In Korea, the Hg and Pb levels in 207 breast milk samples were monitored. The results showed that 45% exceeded the normal range of Pb suggested by WHO, and that 71% of 15-day-old infants and 56% of 30-day-old infants were at potential risk from Pb exposure based on the Monte Carlo simulation (Park et al. 2018). In Brazil, MeHg accounted for 11.8% of total Hg, and the mean weekly intake for MeHg was 0.16 ± 0.22 μg/kg·BW (0.679 μg/kg BW/week in the present study, Table 5), which represented 10% of the provisional tolerable weekly intake (42.4% in the present study). Several studies indicated no health concern for the breastfed infants (Rebelo et al. 2017), but not for immature and vulnerable infants. In Iran, the highest levels of Pb were observed after 2 months of delivery, and up to 94% of the breast milk samples exceeded the suggested WHO limit of < 5 μg/L for Pb contamination (Samiee et al. 2019). In our study, 42.9% of breast milk samples were over 5 μg/L (Table S2). Samiee et al. (2019) suggested a 61% unacceptable non-cancerous health risk levels or HQ for Pb of the breast milk samples. These studies, including ours, all point to a potential risk of toxic metals, especially Pb, for infants via the consumption of breast milk (Park et al. 2018; Samiee et al. 2019).
Sensitivity Analysis of the EDI
Previous studies and our data all proved that infants are at risk of Pb exposure within 1 or 2 months postpartum (Park et al. 2018; Samiee et al. 2019). The breastmilk, which is donated by lactating mothers, is intended for premature delivery and infants, vulnerable to well-known neurological toxicity of Pb, at the 1st month postpartum. Utilizing mother-infant-dyads recruit from the milk bank to estimate the health risk of the infants of dyads and the vulnerable recipients of donor milk, we can confirm that the quality of breastmilk is extremely important.
This study was several research that recently conducted a follow-up of breast milk samples and questionnaires. Thus, it provides sufficient information to investigate the trend of risk during breastfeeding. However, this study also presented several limitations. First, inevitable recall and response bias existed in the questionnaire interviews. Second, except for dietary intake (Table 4), living near any polluted areas within 1 km, clean habit, and cosmetic usage are all influencing factors in metal concentrations in the breast milk. However, these mothers may need to go out to shop without any mask or to work in a polluted area while their residential place are in rural areas. These uncontrolled environmental factors will be the confounders in this study. Third, other heavy metals besides those tested can cause joint toxic reactions. Thus, the synergistic risk can be evaluated if more toxic metals were monitored simultaneously.
Future Direction to Promote the Quality of Human Milk Bank and Maternal Children Health
Currently, the operation of human-donor milk banks in Europe (Kontopodi et al. 2021) and in North America (Brownell et al. 2014) mainly focuses on the safety of donor milk in accordance with the donors’ lifestyle criteria (smoking, alcohol, drug abuse, extreme diet, etc.), maternal infection issue (human immunodeficiency virus, hepatitis viruses, cytomegalovirus, sexually transmitted disease, etc.), and the pathological bacteriology of the collected or pasteurized milk. However, the monitoring of heavy metal contamination in human milk banking has been largely overlooked.
To our best knowledge after literature review, this study is the first cohort observation research conducted on a human milk bank for monitoring of the reported heavy metals. Monitoring heavy metal in donors’ milk may improve not only the health of donors’ offspring but also that of the recipients. Our study result helped donors of the milk bank but also the non-donor lactating women to adjust their lifestyle to avoid further intake of heavy metals from polluted sources. The offspring and recipients who depend on breast milk exclusively could be also protected from intake of heavy metals.
In summary, breast feeding exhibits numerous beneficial effects for mothers and children, including reduction of ovarian and breast cancer risk (Rea 2004; Leung and Sauve 2005), growth promotion, and modulation of immune system (Makrides et al. 1996; Laiho et al. 2003; Wijga et al. 2006; Lepage and Perre 2012; Khaldi et al. 2014; Rogier et al. 2014). Beyond improving physical health, breastfeeding can help in building a close relationship between mothers and their offspring (Guxens et al. 2011; Sabel et al. 2012). The WHO recommends that women breastfeed children for the first 6 months and continue breastfeeding while giving appropriate complementary foods until 2 years of age (WHO 2009; Schwarzenberg and Georgieff 2018). Hence, healthy diets and lifestyle for breastfeeding mothers should be advised. Prioritizing adequate nutrition and healthy dietary patterns during this time is a key factor to ensure a foundation for a child’s optimal neurodevelopment (Schwarzenberg and Georgieff 2018). Based on the results of daily life habits, dietary pattern and risk assessment, the future public policy in promoting breastfeeding should be considered to instruct healthy diets and lifestyle from exposure to heavy metals since the perinatal stage.
Strength and Limitation
Enrollment of participants from a milk bank and with relatively large milk sample size is a strength. Participants from the milk bank were all longitudinal and exclusively breastfed. A total of 26 out 39 (67%) participants continued to provide milk samples and breastfeed during the study period. Not including all participants from their partum immediately was a weakness. However, the enrollment from the partum immediately will result in high dropped out rate since 24.2–29.3% of the mothers were exclusively at 2–6 months postpartum (Taiwan-Health-Promotion-Administration 2012; Chang et al. 2019). Importantly, the study unit, TSHMB, exclusively enrolled the donors within 3 months postpartum and well presented the interesting study cohort.
Conclusions
The results indicated an unacceptable non-cancerous health risk (95% HI = 1.37 > 1) for Pb and Hg, for infants through the consumption of breast milk. Meanwhile, environmental conditions, including indoor air quality, residential districts, cleaning products, and maternal dietary, e.g., drinking water, viscera (organ meat), eggs, seafood and canned food and personal habits, e.g., cosmetics usage, can affect Pb and Hg concentrations under different conditions. In addition, Pb and Hg pose a potential hazard, especially for Pb exposure via breastmilk consumption. Based on the results, heavy metal in human milk, especially for Pb, should be monthly monitored not only in donor milk human milk banks but also in postpartum women who experience traditional confinement and bear children with exclusive breastfeeding. Compared to blood sampling, breast milk is much feasible to be expressed and preserved. Second, breastfeeding mothers with high levels of toxic metals in their breast milk should be given feedback to change their life or dietary style and inhibit from contacting contaminated sources. Third, the synergistic risk of other toxics should be evaluated further to ensure high-quality milk for donors’ offspring and vulnerable recipients who exclusively depend on it. Fourth, a broader public health attention should be paid if the mothers' milk obtained from the study area, irrespective to donation, have higher level of toxic metals.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Admyre C, Johansson SM, Qazi KR, Filen JJ, Lahesmaa R, Norman M et al (2007) Exosomes with immune modulatory features are present in human breast milk. J Immunol 179(3):1969–1978. https://doi.org/10.4049/jimmunol.179.3.1969
Affinito P, Tommaselli GA, di Carlo C, Guida F, Nappi C (1996) Changes in bone mineral density and calcium metabolism in breastfeeding women: a one year follow-up study. J Clin Endocrinol Metabol 81(6):2314–2318
Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T et al (2010) Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr 50(1):85–91. https://doi.org/10.1097/MPG.0b013e3181adaee0
Akan J, Abdulrahman F, Sodipo OA, Chiroma YA (2010) Distribution of heavy metals in the liver, kidney and meat of beef, mutton, caprine and chicken from Kasuwan Shanu market in Maiduguri Metropolis, Borno State, Nigeria. Res J Appl Sci Eng Technol 2(8):743–748
Al-Saleh I, Nester M, Abduljabbar M, Al-Rouqi R, Eltabache C, Al-Rajudi T (2016) Mercury (Hg) exposure and its effects on Saudi breastfed infant’s neurodevelopment. Int J Hyg Environ Health 219(1):129–141. https://doi.org/10.1016/j.ijheh.2015.10.002
Al Zabadi H, Sayeh G, Jodeh S (2018) Environmental exposure assessment of cadmium, lead, copper and zinc in different Palestinian canned foods. Agric Food Secur 7(1):50. https://doi.org/10.1186/s40066-018-0205-1
Bassil M, Daou F, Hassan H, Yamani O, Kharma JA, Attieh Z et al (2018) Lead, cadmium and arsenic in human milk and their socio-demographic and lifestyle determinants in Lebanon. Chemosphere 191:911–921. https://doi.org/10.1016/j.chemosphere.2017.10.111
Braun JM, Froehlich TE, Daniels JL, Dietrich KN, Hornung R, Auinger P et al (2008) Association of environmental toxicants and conduct disorder in U.S. children: NHANES 2001–2004. Environ Health Perspect 116(7):956–962. https://doi.org/10.1289/ehp.11177
Brownell EA, Lussier MM, Herson VC, Hagadorn JI, Marinelli KA (2014) Donor human milk bank data collection in North America: an assessment of current status and future needs. J Hum Lact 30(1):47–53. https://doi.org/10.1177/0890334413508237
Buckle A, Taylor C (2017) Cost and cost-effectiveness of donor human milk to prevent necrotizing enterocolitis: systematic review. Breastfeed Med 12(9):528–536. https://doi.org/10.1089/bfm.2017.0057
Burger J, Gochfeld M (2004) Mercury in canned tuna: white versus light and temporal variation. Environ Res 96(3):239–249. https://doi.org/10.1016/j.envres.2003.12.001
Burger J, Gochfeld M (2005) Heavy metals in commercial fish in New Jersey. Environ Res 99(3):403–412. https://doi.org/10.1016/j.envres.2005.02.001
Cardoso OO, Julião FC, Alves RIS, Baena AR, Díez IG, Suzuki MN et al (2014) Concentration profiles of metals in breast milk, drinking water, and soil: relationship between matrices. Biol Trace Element Res 160(1):116–122. https://doi.org/10.1007/s12011-014-0030-8
Caserta D, Graziano A, Lo Monte G, Bordi G, Moscarini M (2013) Heavy metals and placental fetal-maternal barrier: a mini-review on the major concerns. Eur Rev Med Pharmacol Sci 17(16):2198–2206
Chang FY, Cheng SW, Wu TZ, Fang LJ (2013) Characteristics of the first human milk bank in Taiwan. Pediatr Neonatol 54(1):28–33. https://doi.org/10.1016/j.pedneo.2012.11.004
Chang PC, Li SF, Yang HY, Wang LC, Weng CY, Chen KF et al (2019) Factors associated with cessation of exclusive breastfeeding at 1 and 2 months postpartum in Taiwan. Int Breastfeed J 14:18. https://doi.org/10.1186/s13006-019-0213-1
Chao HH, Guo CH, Huang CB, Chen PC, Li HC, Hsiung DY et al (2014) Arsenic, cadmium, lead, and aluminium concentrations in human milk at early stages of lactation. Pediatr Neonatol 55(2):127–134. https://doi.org/10.1016/j.pedneo.2013.08.005
Chen CH, Chiu HY, Lee SC, Chang HY, Chang JH, Chen YJ et al (2022) Growth of very preterm infants in a low-resourced rural setting after affiliation with a human milk bank. Children (Basel) 9(1):80. https://doi.org/10.3390/children9010080
Cherfi A, Abdoun S, Gaci O (2014) Food survey: levels and potential health risks of chromium, lead, zinc and copper content in fruits and vegetables consumed in Algeria. Food Chem Toxicol 70:48–53. https://doi.org/10.1016/j.fct.2014.04.044
Chien LC, Yeh CY, Lee HC, Jasmine Chao H, Shieh MJ, Han BC (2006) Effect of the mother’s consumption of traditional Chinese herbs on estimated infant daily intake of lead from breast milk. Sci Total Environ 354(2–3):120–126. https://doi.org/10.1016/j.scitotenv.2005.01.033
Comite de nutrition de la Societe francaise de, Turck D, Vidailhet M, Bocquet A, Bresson JL, Briend A et al (2013) Breastfeeding: health benefits for child and mother. Arch Pediatr 20(Suppl 2):S29-48. https://doi.org/10.1016/S0929-693X(13)72251-6
Cortez J, Makker K, Kraemer DF, Neu J, Sharma R, Hudak ML (2018) Maternal milk feedings reduce sepsis, necrotizing enterocolitis and improve outcomes of premature infants. J Perinatol 38(1):71–74. https://doi.org/10.1038/jp.2017.149
Crume TL, Ogden L, Maligie M, Sheffield S, Bischoff KJ, McDuffie R et al (2011) Long-term impact of neonatal breastfeeding on childhood adiposity and fat distribution among children exposed to diabetes in utero. Diabetes Care 34(3):641–645. https://doi.org/10.2337/dc10-1716
de Halleux V, Pieltain C, Senterre T, Rigo J (2017) Use of donor milk in the neonatal intensive care unit. Semin Fetal Neonatal Med 22(1):23–29. https://doi.org/10.1016/j.siny.2016.08.003
Dennis CL, Fung K, Grigoriadis S, Robinson GE, Romans S, Ross L (2007) Traditional postpartum practices and rituals: a qualitative systematic review. Womens Health (Lond) 3(4):87–502. https://doi.org/10.2217/17455057.3.4.487
Díez S (2009) Human health effects of methylmercury exposure. Rev Environ Contam Toxicol 198:111–132. https://doi.org/10.1007/978-0-387-09647-6_3
Dix-Cooper L, Kosatsky T (2018) Blood mercury, lead and cadmium levels and determinants of exposure among newcomer South and East Asian women of reproductive age living in Vancouver, Canada. Sci Total Environ 619–620:1409–1419. https://doi.org/10.1016/j.scitotenv.2017.11.126
Fathabad AE, Shariatifar N, Moazzen M, Nazmara S, Fakhri Y, Alimohammadi M et al (2018) Determination of heavy metal content of processed fruit products from Tehran’s market using ICP-OES: a risk assessment study. Food Chem Toxicol 115:436–446. https://doi.org/10.1016/j.fct.2018.03.044
FDA (2017) About dental amalgam fillings. FDA, Sliver Spring
Feizi R, Jaafarzadeh N, Akbari H, Jorfi S (2019) Evaluation of lead and cadmium concentrations in lipstick and eye pencil cosmetics. Environ Health Eng Manag 6(4):277–282. https://doi.org/10.15171/EHEM.2019.31
García-Esquinas E, Pérez-Gómez B, Fernández MA, Pérez-Meixeira AM, Gil E, de Paz C et al (2011) Mercury, lead and cadmium in human milk in relation to diet, lifestyle habits and sociodemographic variables in Madrid (Spain). Chemosphere 85(2):268–276
Gaxiola-Robles R, Labrada-Martagón V, Acosta-Vargas B, Méndez-Rodríguez LC, Zenteno-Savín T (2014) Interaction between mercury (Hg), arsenic (As) and selenium (Se) affects the activity of glutathione S-transferase in breast milk; possible relationship with fish and shellfish intake. Nutr Hosp 30(2):436–446
Grote V, Verduci E, Scaglioni S, Vecchi F, Contarini G, Giovannini M et al (2016) Breast milk composition and infant nutrient intakes during the first 12 months of life. Eur J Clin Nutr 70(2):250–256
Grzunov LetiniĿ J, Matek SariĿ M, Piasek M, JurasoviĿ J, Varnai VM, Sulimanec Grgec A et al (2016) Use of human milk in the assessment of toxic metal exposure and essential element status in breastfeeding women and their infants in coastal Croatia. J Trace Elem Med Biol 38:117–125. https://doi.org/10.1016/j.jtemb.2016.08.002
Gundacker C, Pietschnig B, Wittmann KJ, Lischka A, Salzer H, Hohenauer L et al (2002) Lead and mercury in breast milk. Pediatrics 110(5):873–878
Guxens M, Mendez MA, Moltó-Puigmartí C, Julvez J, García-Esteban R, Forns J et al (2011) Breastfeeding, long-chain polyunsaturated fatty acids in colostrum, and infant mental development. Pediatrics 128(4):e880–e889
Hon KL, Fung CK, Leung AK (2017) Childhood lead poisoning: an overview. Hong Kong Med J 23(6):616–621. https://doi.org/10.12809/hkmj176214
Iwai-Shimada M, Satoh H, Nakai K, Tatsuta N, Murata K, Akagi H (2015) Methylmercury in the breast milk of Japanese mothers and lactational exposure of their infants. Chemosphere 126:67–72. https://doi.org/10.1016/j.chemosphere.2014.12.086
Jeong KS, Ha E, Shin JY, Park H, Hong YC, Ha M et al (2017) Blood heavy metal concentrations in pregnant Korean women and their children up to age 5years: Mothers’ and Children’s Environmental Health (MOCEH) birth cohort study. Sci Total Environ 605–606:784–791. https://doi.org/10.1016/j.scitotenv.2017.06.007
Kern JK, Geier DA, Homme KG, Geier MR (2020) Examining the evidence that ethylmercury crosses the blood–brain barrier. Environ Toxicol Pharmacol. https://doi.org/10.1016/j.etap.2019.103312
Khaldi N, Vijayakumar V, Dallas DC, Guerrero A, Wickramasinghe S, Smilowitz JT et al (2014) Predicting the important enzymes in human breast milk digestion. J Agric Food Chem 62(29):7225–7232
Khanjani N, Jafari M, Mousavi EA (2018) Breast milk contamination with lead and cadmium and its related factors in Kerman, Iran. J Environ Health Sci Eng 16(2):323–335
Kontopodi E, Arslanoglu S, Bernatowicz-Lojko U, Bertino E, Bettinelli ME, Buffin R et al (2021) Donor milk banking: improving the future. “A survey on the operation of the European donor human milk banks.” PLoS ONE 16(8):e0256435. https://doi.org/10.1371/journal.pone.0256435
Kvestad I, Vabø S, Kjellevold M, Nøstbakken OJ, Midtbø LK, Hysing M et al (2018) Fatty fish, hair mercury and cognitive function in Norwegian preschool children: results from the randomized controlled trial FINS-KIDS. Environ Int 121(Pt 2):1098–1105. https://doi.org/10.1016/j.envint.2018.10.022
Laiho K, Lampi AM, Hämäläinen M, Moilanen E, Piironen V, Arvola T et al (2003) Breast milk fatty acids, eicosanoids, and cytokines in mothers with and without allergic disease. Pediatr Res 53(4):642–647
Lee C, Huang H, Wu Y, Kao Y, Chen H (2018) The health risks of lead and cadmium in foodstuffs for the general population of Taiwan. J Exp Food Chem. https://doi.org/10.4172/2472-0542.1000137
Lepage P, Van de Perre P (2012) The immune system of breast milk: antimicrobial and anti-inflammatory properties. Human Immunodeficiency Virus type 1 (HIV-1) and breastfeeding. Adv Exp Med Biol 743:121–137. https://doi.org/10.1007/978-1-4614-2251-8_9
Leung AK, Sauve RS (2005) Breast is best for babies. J Natl Med Assoc 97(7):1010
Lucas A, Morley RT, Cole J, Lister G, Leeson-Payne C (1992) Breast milk and subsequent intelligence quotient in children born preterm. Lancet 339(8788):261–264. https://doi.org/10.1016/0140-6736(92)91329-7
Makrides M, Neumann M, Gibsona RA (1996) Effect of maternal docosahexaenoic acid (DHA) supplementation on breast milk composition. Eur J Clin Nut 50(6):352–357
Marangoni F, Cetin I, Verduci E, Canzone G, Giovannini M, Scollo P et al (2016) Maternal diet and nutrient requirements in pregnancy and breastfeeding. An Italian consensus document. Nutrients 8(10):629
MOHW-HPA (2019) Breast feeding in Taiwan (Traditional Chinese). https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=506&pid=463
Moro GE, Billeaud C, Rachel B, Calvo J, Cavallarin L, Christen L et al (2019) Processing of donor human milk: update and recommendations from the European Milk Bank Association (EMBA). Front Pediatr 7:49. https://doi.org/10.3389/fped.2019.00049
Needleman HL (2004) Low level lead exposure and the development of children. Southeast Asian J Trop Med Public Health 35(2):252–254
Newburg DS, Woo JG, Morrow AL (2010) Characteristics and potential functions of human milk adiponectin. J Pediatr 156(2 Suppl):S41-46. https://doi.org/10.1016/j.jpeds.2009.11.020
Niemi A, Venäläinen ER, Hirvi T, Hirn J, Karppanen E (1991) The lead, cadmium and mercury concentrations in muscle, liver and kidney from Finnish pigs and cattle during 1987–1988. Z Lebensm Unters Forsch 192(5):427–429. https://doi.org/10.1007/bf01193141
Norouzi E, Bahramifar N, Ghasempouri SM (2012) Effect of teeth amalgam on mercury levels in the colostrums human milk in Lenjan. Environ Monit Assess 184(1):375–380
Nriagu JO, Blankson ML, Ocran K (1996) Childhood lead poisoning in Africa: a growing public health problem. Sci Total Environ 181(2):93–100. https://doi.org/10.1016/0048-9697(95)04954-1
Pammi M, Suresh G (2017) Enteral lactoferrin supplementation for prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database Syst Rev 6:CD007137. https://doi.org/10.1002/14651858.CD007137.pub5
Park Y, Lee A, Choi K, Kim HJ, Lee JJ, Choi G et al (2018) Exposure to lead and mercury through breastfeeding during the first month of life: a CHECK cohort study. Sci Total Environ 612:876–883. https://doi.org/10.1016/j.scitotenv.2017.08.079
Piomelli S (2002) Childhood lead poisoning. Pediatr Clin North Am. https://doi.org/10.1016/s0031-3955(02)00097-4
Rea MF (2004) Benefits of breastfeeding and women’s health. J Pediatr (Rio J) 80(5 Suppl):S142–S146
Rebelo FM, Cunha LRD, Andrade PD, Costa Junior WAD, Bastos WR, Caldas ED (2017) Mercury in breast milk from women in the Federal District, Brazil and dietary risk assessment for breastfed infants. J Trace Elem Med Biol 44:99–103. https://doi.org/10.1016/j.jtemb.2017.06.009
Rogier EW, Frantz AL, Bruno ME, Wedlund L, Cohen DA, Stromberg AJ et al (2014) Secretory antibodies in breast milk promote long-term intestinal homeostasis by regulating the gut microbiota and host gene expression. Proc Natl Acad Sci USA 111(8):3074–3079. https://doi.org/10.1073/pnas.1315792111
Sabel KG, Strandvik B, Petzold M, Lundqvist-Persson C (2012) Motor, mental and behavioral developments in infancy are associated with fatty acid pattern in breast milk and plasma of premature infants. Prostaglandins Leukot Essent Fat Acids 86(4–5):183–188
Samiee F, Vahidinia A, Taravati Javad M, Leili M (2019) Exposure to heavy metals released to the environment through breastfeeding: a probabilistic risk estimation. Sci Total Environ 650(Pt 2):3075–3083. https://doi.org/10.1016/j.scitotenv.2018.10.059
Schwarzenberg SJ, Georgieff MK (2018) Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics. https://doi.org/10.1542/peds.2017-3716
Sedki A, Lekouch N, Gamon S, Pineau A (2003) Toxic and essential trace metals in muscle, liver and kidney of bovines from a polluted area of Morocco. Sci Total Environ 317(1–3):201–205. https://doi.org/10.1016/s0048-9697(03)00050-0
Sherry CL, Oliver JS, Marriage BJ (2015) Docosahexaenoic acid supplementation in lactating women increases breast milk and plasma docosahexaenoic acid concentrations and alters infant omega 6:3 fatty acid ratio. Prostaglandins Leukot Essent Fat Acids 95:63–69. https://doi.org/10.1016/j.plefa.2015.01.005
Sowers MR, Scholl TO, Hall GM, Jannausch L, Kemp FW, Li X et al (2002) Lead in breast milk and maternal bone turnover. Am J Obstet Gynecol 187(3):770–776. https://doi.org/10.1067/mob.2002.125736
Stefanescu BM, Gillam-Krakauer M, Stefanescu AR, Markham M, Kosinski JL (2016) Very low birth weight infant care: adherence to a new nutrition protocol improves growth outcomes and reduces infectious risk. Early Hum Dev 94:25–30. https://doi.org/10.1016/j.earlhumdev.2016.01.011
Taiwan-Health-Promotion-Administration (2012) Feeding with breast milk in Taiwan: the past and the future. https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=1132&pid=2455. Accessed 1 Mar 2021
Taiwan-Health-Promotion-Administration (2015) Exclusive breastfeeding for six months: the gold standard for infant feeding. https://www.hpa.gov.tw/EngPages/Detail.aspx?nodeid=1052&pid=5962. Accessed 1 Mar 2021
TFDA (2020) Method of test for heavy metals in beverages and milk products. https://gazette.nat.gov.tw/egFront/detail.do?metaid=113612&log=detailLog. Accessed 15 May 2021
Tudehope DI (2013) Human milk and the nutritional needs of preterm infants. J Pediatr 162(3 Suppl):S17-25. https://doi.org/10.1016/j.jpeds.2012.11.049
Vahidinia A, Samiee F, Faradmal J, Rahmani A, Javad MT, Leili M (2019) Mercury, lead, cadmium, and barium levels in human breast milk and factors affecting their concentrations in Hamadan, Iran. Biol Trace Elem Res 187(1):32–40
Villamor-Martinez E, Pierro M, Cavallaro G, Mosca F, Kramer BW, Villamor E (2018) Donor human milk protects against bronchopulmonary dysplasia: a systematic review and meta-analysis. Nutrients. https://doi.org/10.3390/nu10020238
Vollset M, Iszatt N, Enger Ø, Gjengedal ELF, Eggesbø M (2019) Concentration of mercury, cadmium, and lead in breast milk from Norwegian mothers: association with dietary habits, amalgam and other factors. Sci Total Environ 677:466–473. https://doi.org/10.1016/j.scitotenv.2019.04.252
Wijga AH, van Houwelingen AC, Kerkhof M, Tabak C, de Jongste J, Gerritsen CJ et al (2006) Breast milk fatty acids and allergic disease in preschool children: the prevention and incidence of asthma and mite allergy birth cohort study. J Allergy Clin Immunol 117(2):440–447
World Health Organization (WHO) (2009) Infant and young child feeding: model chapter for textbooks for medical students and allied health professionals. World Health Organization (WHO), Geneva
Zhou P, Li Y, Ma LY, Lin HC (2015) The role of immunonutrients in the prevention of necrotizing enterocolitis in preterm very low birth weight infants. Nutrients 7(9):7256–7270. https://doi.org/10.3390/nu7095334
Acknowledgements
We are grateful for the support from the staff of Taiwan Southern Human Milk Bank of National Cheng Kung University Hospital.
Funding
This work was supported by the National Cheng Kung University Hospital (Grant Nos. NCKUH-11001002; NCKUH-11101001; NCKUH-11106013).
Author information
Authors and Affiliations
Contributions
Y-CL: methodology, data curation, writing—original draft, visualization; W-HC: methodology, data validation, writing—review & editing; T-CL: methodology, data curation, chemical analysis; OI: writing—review & editing; H-LC: conceptualization, data curation, supervision, writing—original draft, writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lin, YC., Chang, WH., Li, TC. et al. Health Risk of Infants Exposed to Lead and Mercury Through Breastfeeding. Expo Health 15, 255–267 (2023). https://doi.org/10.1007/s12403-022-00485-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12403-022-00485-1