Abstract
Background
The Covid-19 pandemic led to a complete renewal of clinical activities of Italian hospitals. During the lockdown, all hospitals in Italy had to suspend non-urgent clinical activities. The prolonged suspension of elective activities could have caused a series of problems.
Methods
A new ad hoc protocol was designed. Single-day fast-imaging protocol with regadenoson-stress 99mTc-tetrofosmin imaging was preferred. Patients were contacted by phone 4 days before the test and answered to a questionnaire which will be repeated on the day of the exam. Body temperature <37.5 degrees C and no Covid-19 symptoms were necessary to enter the unit. Patients wore surgical mask and gloves. Social distancing was maintained throughout the examination. Healthcare professionals wore a personal protective equipment.
Results
A total of 46 patients were studied from April 7 to May 15, 2020, before the publication of the recommendations from ASNC and SNMMI. None of the patients experienced complications. Follow-up of patients discharged was carried by phone. No Covid-19 infection symptoms were reported. On May 18, 2020 all the healthcare providers of nuclear cardiology department underwent serological testing IgG and IgM and none were positive.
Conclusion
Strict ad hoc hygiene protocol for Covid-19 pandemic avoids diagnostic-therapeutic delay and lengthening of waiting lists. Our experience confirms that pursuing WHO recommendations and recent indication of ASNC and SNMMI is safe for both health providers and patients. Moreover, the incidence of significant inducible ischemia rises when correct stratification of patients is performed.
Similar content being viewed by others
Background
Coronavirus 2019 disease initially identified in Wuhan (China) has rapidly evolved resulting in a public health emergency. The World Health Organization declared that Covid-19 can be characterized as a pandemic on March 11, 2020.1 Covid-19 has infected over five million individuals worldwide and killed over 325,509 people so far at the writing of this paper.2 Northern Italy was one of the pandemic’s epicenter with more than 226,000 coronavirus cases and 32,169 deaths.2 The most recognizable feature of Covid-19 is to cause severe respiratory complications, which largely depends on the overall state of wellbeing of the infected patient. Age, patient’s underlying comorbidities and the condition of the immune system also play a major role in the severity of the disease.3,4 Many signs and symptoms are associated with the infection such as fever, dyspnea, cough, headache and diarrhea.5 The Covid-19 pandemic led to a complete renewal of clinical activities of Italian hospitals following the high number of infected patients and their need for intensive care unit (ICU). Italian government took desperate strategies to counteract the spread of the virus avoiding the national health system to collapse. Lockdown measures blocked all elective medical activities. Generalized feared among population and limitation of mobility, have brought to a significant decrease in acute coronary syndrome-related hospitalization rates (-40%) across cardiovascular centers in Italy compared to the same period of 2019 as shown by De Filippo et al.6 The aim of this report is to demonstrate how strong collaboration of multidisciplinary teams is required to quickly design a new safety protocol able to ensure continuous patient care during pandemic, protecting both health care professionals and patients without lengthening the waiting lists, as well as, the necessity to better select patients to observe an increased incidence in inducible ischemia.
Methods
Pathway Toward a New COVID-19 Protocol
During the acute phase of the pandemic, from March 3, 2020, all hospitals in Italy had to suspend non-urgent clinical activities. The prolonged suspension of elective activities could have caused a series of problems such as (1) extension of the waiting lists and (2) diagnostic-therapeutic delay in high-risk patients leading to an increased risk of life-threatening events. To avoid such issues, our team designed a new ad hoc Covid-19 protocol for internal use, to continue to perform perfusion heart scans assuring the highest level of safety as possible for healthcare professionals and to patients. At that time, no official recommendation had yet been published on how the activity of nuclear cardiology department should be organized, therefore our protocol was produced based on WHO general guidelines on hand hygiene, respiratory etiquette and practice social distancing, as well as shifting non-urgent activities, use dedicated environments for Covid-19 suspected or positive patients and with the help of telemedicine.7 On April 7, 2020 our department of Nuclear Cardiology resumed elective activities, therefore during Covid-19 pandemic lockdown.
Optimization of Stress Myocardial Perfusion Scan
A new ad hoc protocol was designed to allow the unit to perform stress myocardial perfusion scintigraphy respecting the virus containment measures and ensuring safety of patients and health personnel. The solution to ensure least contact between patient and healthcare professionals for the shortest time was to convert the standard exercise-induced stress test with the pharmacological test using regadenoson. Therefore, single-day fast-imaging protocol with regadenoson-stress imaging was preferred to all patients using 99mTc-1,2-bis[bis(2-ethoxyethyl)phosphino]ethane (tetrofosmin) with a dose of 370 MBq + 1100 MBq. Regadenoson rapid protocol consists in a bolus over 10 seconds followed by a 10 seconds flush of 5 to 10 ml physiological solution (NaCl 0.9%), 10-20 seconds later the radiopharmaceutical is injected. Regadenoson is administered independent of patient weight in a dose of 0.4 mg in 5 ml.8 Within 15-20 minutes, the patient underwent gated myocardial perfusion SPECT. If further images are required, the re-acquisition is performed 2-3 hours after the first injection.
Images Acquisition Times
Early images were acquired 15 minutes after 99mTc-injection at the end of the pharmacological test. Second administration of the radiopharmaceutical occurred after 120 minutes from the first 99mTc-injection at rest. Between the second injection and the late images (around 30 minutes), patients were asked to eat a small fatty meal. Acquisition with SPECT / TC tomography gamma-camera (GE) equipped with parallel holes collimators low-energy high-resolution (LEHR); Matrix at least 64 × 64; Zoom 1-1.3; Angular sampling 3°-4°; 180° rotation from 45° OAD to 135° OPS; 20”/ frame; 16 frames / cycle Gated-SPECT with tolerance window for R-R range of ± 20%. Our TC module was used as a non-diagnostic unit with the purpose of anatomical localization and to perform the correction for attenuation.
Selection of Patients
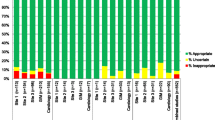
Every patient’s medical record was registered electronically on our system and everyone was assigned to four categories based on the urgency to perform the test.
The Italian health system provides the classification priority of medical services dividing in U, B, D and P-label. Patients with U-label (urgent) needed to undergo stress test within 3 days; B-label (short urgent) test to be performed within 10 days, D-label (deferred) test can be postponed up to 30 days and P-label were patients without any priority. Our team adopted such classification and stratification was performed based on clinical and diagnostic data: (1) symptoms, (2) history of stress test, (3) diabetes, (4) chronic coronary occlusion (5) symptomatic borderline coronary lesions, (6) oncological follow-up (7) reduced ejection fraction and (8) multidisciplinary discussion with hemodynamic unit.
During the pandemic period there were no U-label requests. B- and D-label patients were contacted by phone 4 days before the test. During the call patients answered to a questionnaire which will be repeated on the day of the exam before entering the unit. Figure 1 represents the simplified version of the submitted questionnaire. Patients with suspicious symptoms for Covid-19 were postponed. 12 patients refused to perform the examination asking to be called back only when Italian health authorities would have declared the end of the restrictions on hospital admissions. Among the 12 patients, 2 had mild symptoms such as catarrhal cough but not fever.
Access Rules on Test Day
The department of Nuclear Medicine of our facility has a dedicated entry and does not require main hospital access. Therefore, bypassing the emergency room avoiding potentially risky route.
The unit is equipped with an autonomous ventilation system independent from the remaining hospital structure. Before entering the ward, the body temperature of patients was measured with an infrared thermometer avoiding any contact, moreover the same questionnaire in Figure 1 was delivered. If the patient had a body temperature below 37.5 degrees Celsius (99.5 Fahrenheit) and no suspicion of Covid-19 was suspected based on the answer given to the questionnaire, the patient was allowed to enter the ward after positioning a surgical mask and wearing gloves. Only the patient was allowed to enter in the unit without any other relatives. Social distancing was maintained throughout the rooms and a maximum of 4 patients were allowed to stay maintaining at least 2 meters of distance by each other. While waiting between the rest and stress image acquisition, no patient was invited to leave the nuclear medicine department, but they were invited to stay in the waiting room equipped with bathroom. Our waiting room for radio-injected patients complies with the legal regulations as well as the bathroom which is equipped with protected drains. In case of test requests from other hospital units of positive Covid-19 patient, this would have been performed in our ward only in the absence of other patients and subsequently a complete disinfection would have been performed.
Personal Protective Equipment for Healthcare Professionals
All the healthcare professionals wore a personal protective equipment composed of an FFP2 mask plus a surgical mask, class III biohazard suit, face visor, disposable shoe covers and double gloves. The second gloves were changed for each patient. Hand sanitizer was used between each maneuver. The patient signed the informed consent using a pen that was disinfected after use as well as the support surface. In a separated room, the nurse isolates the venous access and places the disposable ECG electrodes.
Imaging Acquisition and Stress Test
Pharmacological stress test with regadenoson was performed to all patients in the presence of the nurse and the nuclear cardiologist. This ensured minimum contact between patient and healthcare professional for the shortest time in the unit. Average execution time 4.30 minutes. At the end of the stress test, the patients followed the radiology technician maintaining 2 meters distance. Acquisition of images with single-day fast-imaging protocol with regadenoson-stress 99mTc-tetrofosmin imaging was achieved. Successively, the nuclear doctor processed the images in a separate area from the room in which the test has been performed. If the examination turned negative, the patient was discharged. If further images were required, the re-acquisition would have been performed 2-3 hours after the first injection. Full sanitization of all equipments used for the test was performed after each patient. At the end of the day the unit was completely sanitized.
Results
A total of 46 patients with a median age of 66 years (49-85 years) were studied from April 7 to May 15, 2020, before the publication of the recommendations from American Society of Nuclear Cardiology (ASNC) and Society of Nuclear Medicine and Molecular Imaging (SNMMI)9,10. 33 were males (71.7%) and 13 were females (28.3%). 29 out of 46 patients were already diagnosed with chronic ischemic cardiopathy and the remainder underwent to stress myocardial perfusion scintigraphy to further study their underlying conditions.
18 patients (39%) were labeled with priority B and 28 (61%) with priority D. Overall, 9 male patients out of 46 (19.6%) had moderate inducible ischemia. The presence of symptoms (undefined dyspnea and/or precordial pain) associated with one or more clinical parameters mentioned above, especially if associated with diabetes and reduced ejection fraction let the patients to be labeled in B category. Among such patients, 5 had significant ischemia. D-labeled patients were asymptomatic but had at least 2 positive clinical parameters and 4 patients had significant ischemia, 3 of them had diabetes. Table 1 summarizes the results.
Our data seem to indicate that the presence of symptoms, diabetes and reduced ejection fraction are the most useful stratification parameters. Using the stratification methodology, the incidence of significant inducible ischemia rose up to 19.4% with respect to 7.69% of the same period of 2019 when no stratification was used. These data highlighted the reliability of the categorization in four groups of patients based on the urgency to assign test-priorities. None of the patients experienced complications. Short follow-up of patients discharged was carried by phone and no complaints were registered as well as absence of Covid-19 infection symptoms. On May 18, 2020 all the health personnels of nuclear cardiology department underwent serological tests testing IgG and IgM and none were positive.
Conclusion
The Nuclear Cardiology Team of Moncalieri Hospital is composed of a nuclear cardiologist, a nuclear doctor, a dedicated nurse and a nuclear technician. Strong collaboration of multidisciplinary teams is required to quickly design and apply a new safety protocol able to ensure continuous patient care during pandemic, protecting both health care professionals and patients without lengthening the waiting lists. Following strict hygiene rules protocol during Covid-19 pandemic allowed our team to continue study all patients with necessity of performing stress tests avoiding diagnostic-therapeutic delay leading to an increased risk of life-threatening events. In fact, using the new stratification methodology, the incidence of significant inducible ischemia rose almost by 300% with respect to non-stratification period in 2019. Despite the difference in number of patients studied by Bourque et al., their incidence of significant ischemia shown with stress myocardial perfusion scintigraphy in diabetic patients, which are at high risk of cardiovascular events was of 5.7%, with respect to 19.6% when patients were stratified with our method.11 Also waiting list did not lengthen. Our experience in nuclear cardiology unit during active Covid-19 pandemic when no official recommendation had yet been published confirms that pursuing WHO recommendations and recent indication of ASNC and SNMMI is safe for both health providers and patients.
New Knowledge Gained
The presence of symptoms such as undefined dyspnea and/or precordial pain in patients with diabetes and reduced ejection fraction can be the most useful stratification parameters to select effectively patients to observe an increased incidence in inducible ischemia. Moreover, strict ad hoc hygiene protocol for Covid-19 pandemic avoids diagnostic-therapeutic delay and lengthening of waiting lists.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- ICU:
-
Intensive care unit
- ACS:
-
Acute coronary syndrome
References
WHO - coronavirus disease (COVID-19) Pandemic Accessed May 20, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
Coronavirus Cases: Worldometer. (n.d.). (accessed May 20, 2020). https://www.worldometers.info/coronavirus/.
Wang W, Tang J, Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan. China. J Med Virol 2020. https://doi.org/10.1002/jmv.25689.
Ruirui Wang, Min Pan, Xiumei Zhang, Xiaoyun Fan, Mingfeng Han, Fengde Zhao, Manli Miao, Jing Xu, Minglong Guan, Xia Deng, Xu Chen LS. Epidemiological and clinical features of 125 Hospitalized Patients with COVID-19 in Fuyang, Anhui, China. 2020;(January):19-20.
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2019. https://doi.org/10.1016/S0140-6736(20)30183-5.
De Filippo O, D’Ascenzo F, Angelini F, et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med 2020. https://doi.org/10.1056/NEJMc2009166.
World Health Organization. Critical preparedness , readiness and response actions for COVID-19 . 2020;(March):1-3.
Verberne HJ, Acampa W, Anagnostopoulos C, et al. EANM Procedural Guidelines for Radionuclide Myocardial Perfusion Imaging with SPECT and SPECT / CT Chair of Writing Committee ( Responsible for the Coordination of the Overall Process): Hein J . Verberne and Birger Hesse Authors: Correspondence to: H.; 2015.
Skali H, Murthy VL, Al-Mallah MH, et al. Guidance and best practices for nuclear cardiology laboratories during the coronavirus disease 2019 (COVID-19) pandemic: An Information Statement from ASNC and SNMMI. J Nucl Cardiol. 2020 https://doi.org/10.1007/s12350-020-02123-2.
Skali Hicham, Murthy Venkatesh L., Paez Diana, Choi Elisa M., Keng Felix Y. J., McGhie A. Lain, Al-Mallah Mouaz, Campisi Roxana, Bateman Timothy M., Carrio Ignasi, Beanlands Rob, Calnon Dennis A, Dilsizian Vasken, Dondi Maurizio, Gimelli Alessia, Pagnanel TRC. Guidance and Best Practices for Reestablishment of Non-Emergent Care in Nuclear Cardiology Laboratories during the Coronavirus Disease 2019 (COVID-19) Pandemic: An Information Statement from ASNC, IAEA, and SNMMI. 2019;2019:1-12. doi:http://doi.org/10.5281/zenodo.3827461
Bourque JM, Patel CA, Ali MM, Perez M, Watson DD, Beller GA. Prevalence and predictors of ischemia and outcomes in outpatients with diabetes mellitus referred for single-photon emission computed tomography myocardial perfusion imaging. Circ Cardiovasc Imaging 2013;6(3):466-77. https://doi.org/10.1161/CIRCIMAGING.112.000259.
Acknowledgment
Thanks to Nurse Cristina Napione who first planned the strategy to continue to assist patients and designed the questionnaires to be submitted. In this period of great uncertainty courage and determination are our strongest weapons.
Disclosures
The authors have nothing to disclose.
Author information
Authors and Affiliations
Contributions
GS conceptualized the manuscript and prepared the first draft. MD and GB finalized all drafts of the manuscript. GC provided data. GS, MD, GB, GC and PDS provided guidance on structure, reviewed the manuscript, and approved the final version of the manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Funding
No funding.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Scrima, G., D’Amico, M., Bertuccio, G. et al. Safety measures and clinical outcome of Nuclear Cardiology Department during Covid-19 lockdown pandemic: Northern Italy experience. J. Nucl. Cardiol. 28, 331–335 (2021). https://doi.org/10.1007/s12350-020-02286-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02286-y