Abstract
Purpose
The aim of this article is to report a case of uveal tuberculoma simulating an intraocular tumor in which the diagnosis was only possible by polymerase chain reaction (PCR) analysis.
Method
This is a case report.
Results
A36-year-old male presented with a progressive growing intraocular tumor and no history or positive test for other systemic disease. The eye eventually turned blind and painful and was enucleated. Histopathologic analysis revealed a granulomatous reaction and caseation necrosis but failed to identify any causative microorganisms. Final tuberculosis diagnosis was only possible by quantitative PCR.
Conclusion
Isolated uveal tuberculoma can present in an otherwise healthy patient with negative systemic tuberculosis evaluation. PCR can be used to confirm tuberculosis when other methods have failed.
Similar content being viewed by others
An isolated uveal tuberculoma in the absence of detectable systemic disease is exceedingly rare [1–8]. We present a case of an isolated uveal tuberculoma that simulated an intraocular tumor in an immunocompetent patient with no other signs of tuberculosis (TB). Final diagnosis was only possible by histopathologic study and real time quantitative polymerase chain reaction test (qPCR).
Case report
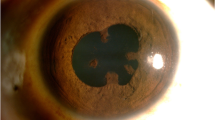
A 36-year-old male patient was referred with clinical suspicion of an intraocular tumor in the right eye (OD). He reported the use of systemic pirimetamine, sufadiazine, and prednisone, plus topical predinisolone acetate for presumed toxoplasmosis intermediate uveitis over the last 3 months with partial and transitory improvement in visual acuity (VA). Before toxoplasma treatment, a systemic investigation revealed non reagent tuberculin skin test (TST) and normal chest radiograph. VA was 0.6 in OD, anterior chamber was unremarkable, and the vitreous exhibited a mild cellular reaction. An elevated yellow mass with exudation was detected in the temporal inferior periphery. On ultrasonography the mass involved the ciliary body and choroidal periphery, exhibited medium and irregular internal reflectivity and measured 5.1-mm thick by 11.9 mm in the largest basal diameter (Fig. 1a). The patient was scheduled for cryotherapy for a presumed vasoproliferative tumor. After four cryotherapy sessions VA decreased to counting fingers, the surrounding retina was detached, there was worsening of vitreous haze and multiple hemorrhages were present over the tumor's surface. The tumor has increased to 7.7-mm thick by 13.1 mm in largest base (Fig. 1b). Unfavorable evolution prompted a differential diagnosis with a malignant uveal neoplasia and enucleation was proposed but refused by the patient. Fine-needle biopsy was out of question due to vitreous haze and retinal detachment. A sclerouveal biopsy guarded by a thick scleral flap was done with the warning of impending early enucleation if a uveal malignancy was confirmed. Histopathologic evaluation revealed only uveal tissue with fibrosis, probably due to the previous cryotherapy. The patient abandoned the follow-up for 2 months, then returned with a blind painful eye and a white subconjunctival nodule located at previous surgical site, measuring 4 mm in largest base (Fig. 1c). The eye was enucleated.
a Ultrasonography at presentation shows a 5.1-mm thick peripheral tumor (arrow); b Ultrasonography after cryotherapy reveals a detached retina (arrow) and a tumor with increased dimensions; c Clinical aspect after extraocular extension (arrow); d Gross aspect. Solid tumor with transcleral extension (arrow)
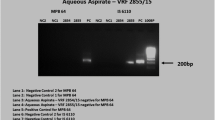
Gross examination revealed a solid white tumor located at ciliary body and peripheral choroid with surrounding retinal detachment and transcleral extraocular extension (Fig. 1d). Optical microscopy revealed chronic granulomatous inflammatory reaction with caseation necrosis and multinucleated giant cells but no acid-fast bacillus on Ziehl-Neelsen (Fig. 2a). Real time quantitative PCR on paraffin-embedded material revealed 560 Mycobacterial tuberculosis genomes in five 20-μm histologic sections (Fig. 2b and c), according to a previously described method [9].
a Quantitative real time PCR graph represents amplification curves (blue—amplification curve of standard DNA; red—amplification curve of experimental specimen). b Quantitative real time PCR graph represents melting curves (blue—melting curve of standard DNA; red—melting curve of experimental specimen). c Histopathological evaluation reveals caseating necrosis (black arrow) with multinucleated giant cells (white arrow)
A new systemic evaluation for TB that was again negative. Triple drug antitubercular therapy was started with rifampin, isoniazid, and pyrazinamide. After 3 years of follow-up, no other TB focus was detected.
Discussion
Although rare, isolated uveal tuberculoma masquerading as intraocular tumors are a well-know situation [1–8]. In almost all reported cases, TB could be suspected based on a history of previous infection, presence of other clinical active focus of TB or strong TST reaction [1, 2]. We found another nine cases of ocular TB with no systemic detectable disease and normal chest radiograph, but in three of them strong TST reaction was noted and in a fourth patient non-reacting TST was attributed to pregnancy [1–8]. Other causes of non-reacting TST in TB cases are terminal diseases, AIDS, other infections, or post immunization status and steroids [1, 2]. Our patient, like five other previously reported, did not fit in any of these [1–8]. In such cases, TB diagnosis relies on bacillus identification, culture of tissue specimens, and samples from intraocular fluids, posterior development of other TB foci or improvement on therapeutic test [1, 2]. On clinical practice the feasibility of all these possibilities can be questioned. TB cultures have an 8 weeks delay and false negative results are frequent when the samples are so reduced as those from intraocular fluids [1]. Although the finding of granulomatous reaction with caseation necrosis is suggestive of TB, in some cases no bacillus can be found on specific stains [1, 8]. Therapeutic test is also difficult to perform since it involves the use of several drugs with potential side effects for 4 to 6 weeks [1, 8]. An interesting alternative, considered adequate for small samples like vitreous or aqueous taps and for use on fixated tissue, is the PCR study [1, 8].
In the present case, uveal tuberculoma was not suspected because the patient was apparently in good health with no systemic complaints, did not exhibit clinical antecedents of TB, and had normal chest radiograph with non-reacting TST before initiating the toxoplasmosis treatment.
Another issue is whether to treat such patients after enucleation, in the absence of systemic detectable disease. Since this represents extrapulmonary TB a complete regimen of antitubercular therapy is mandatory. A well-illustrated consequence of missing such treatment is seen in the case reported by Demirci et al., in which the patient was not treated and developed TB peritonitis 6 months after enucleation [2].
In conclusion we presented a case of isolated uveal tuberculoma masquerading as an intraocular tumor in an immunocompetent patient with repeated negative TST and chest radiograph. The eye was enucleated and although typical findings were seen on microscopic examination, no bacillus could be identified on acid-fast stain and final etiologic diagnosis was only possible by qPCR study.
References
Gupta V, Gupta A, Rao NA (2007) Intraocular tuberculosis—an update. Surv Ophthalmol 52(6):561–587
Demirci H, Shields CL, Shields JA, Eagle RC Jr (2004) Ocular tuberculosis masquerading as ocular tumors. Surv Ophthalmol 49:78–89
Levecq LY, De Potter P (2005) Solitary choroidal tuberculoma in an immunocompetent patient. Arch Ophthalmol 123:864–866
Mansour AM, Haymond R (1990) Choroidal tuberculomas without evidence of extraocular tuberculosis. Graefes Arch Clin Exp Ophthalmol 228:382–383
Berinstein DM, Gentile RC, McCormick SA, Walsh JB (1997) Primary choroidal tuberculoma. Arch Ophthalmol 115:430–431
Sarvananthan N, Wiselka M, Bibby K (1998) Intraocular tuberculosis without detectable systemic infection. Arch Ophthalmol 116:1386–1388
Shen J, Han W, To CH, Wang J (2007) Choroidal tuberculoma in pregnancy. Retina 27(1):106–109
Bowyer JD, Gormley PD, Seth R, Downes RN, Lowe J (1999) Choroidal tuberculosis diagnosed by polymerase chain reaction: a clinicopathologic case report. Ophthalmology 106:290–294
Rao NA, Saraswathy S, Smith RE (2006) Tuberculous uveitis: distribution of Mycobacterium tuberculosis in retinal pigment epithelium. Arch Ophthalmol 124(12):1777–1779
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Marback, E.F., de Souza Mendes, E., Chagas Oliveira, R.D. et al. Isolated uveal tuberculoma masquerading as an intraocular tumor in an immunocompetent patient—a clinical-pathologic study with diagnosis by PCR. J Ophthal Inflamm Infect 1, 81–84 (2011). https://doi.org/10.1007/s12348-010-0010-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12348-010-0010-x