Abstract
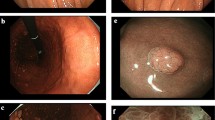
A 71-year-old woman was given a barium meal examination as part of a workup for recurring melena and iron deficiency anemia (IDA), and it revealed a large duodenal polyp measuring 60 mm in diameter. Subsequent upper gastrointestinal endoscopy showed a large pedunculated polyp in the duodenal bulb. Magnifying endoscopy with narrow-band imaging (NBI) showed that the lesion consisted of a regular enlarged intervening part between crypts of the epithelium that resembled gastric mucosa. Although the lesion was suspected of being benign, it was resected by endoscopic submucosal dissection (ESD) to prevent the progression of the IDA. The pathology examination revealed the proliferation of mildly irregular-shaped or dilated glands lined by cuboidal cells and low columnar cells in the submucosa. The gastric glands were immunohistochemically positive for MUC6, suggesting pyloric gland differentiation. The lesion was covered by a foveolar-type epithelium, and we made a diagnosis of pyloric gland adenoma (PGA). PGAs are most common in the stomach, and they are rare in the duodenum, where endoscopic treatment is technically challenging. Here we report a case of large duodenal PGA successfully resected by ESD. Since part of PGAs has been reported to be associated with adenocarcinoma, minimally invasive treatment strategies are desirable to reduce the risk of progression to carcinoma.




Similar content being viewed by others
References
Pezhouh MK, Park JY. Gastric pyloric gland adenoma. Arch Pathol Lab Med. 2015;139:823–6.
Bakotic BW, Robinson MJ, Sturm PD, et al. Pyloric gland adenoma of the main pancreatic duct. Am J Surg Pathol. 1999;23(2):227–31.
Yahagi N, Kato M, Ochiai Y, et al. Outcomes of endoscopic resection for superficial duodenal epithelial neoplasia. Gastrointest Endosc. 2018;88(4):676–82.
Chen ZM, Scudiere JR, Abraham SC, et al. Pyloric gland adenoma: An entity distinct from gastric foveolar type adenoma. Am J Surg Pathol. 2009;33(2):186–93.
Endo M, Abiko Y, Oana S, et al. Usefulness of endoscopic treatment for duodenal adenoma. Dig Endosc. 2010;22:360–5.
Tsuji S, Doyama H, Tsuji K, et al. Preoperative endoscopic diagnosis of superficial non-ampullary duodenal epithelial tumors, including magnifying endoscopy. World J Gastroenterol. 2015;21:11832–41.
Maruoka D, Arai M, Ishigami H, et al. Cold polypectomy for nonampullary duodenal adenoma. Endoscopy. 2015;47(Suppl 1):E477–8.
Mitsuishi T, Hamatani S, Hirooka S, et al. Clinicopathological characteristics of duodenal epithelial neoplasms: Focus on tumors with a gastric mucin phenotype (pyloric gland-type tumors). PLoS ONE. 2017;12(4):e0174985.
Kushima R, Mukaisho K, Vieth M, et al. Pyloric-gland-type adenomas of the stomach. Stomach Intestine. 2003;38:1377–87.
Kushima R. “Jūnishichō: Igata no sennshu gan” [Gastric-type Adenoma and Adenocarcinoma of the Duodenum]. Stomach and Intestine. 2020;55:425–8 ((in Japanese)).
Miller GC, Kumarasinghe MP, Borowsky J, et al. Clinicopathological features of pyloric gland adenomas of the duodenum: a multicentre study of 57 cases. Histopathology. 2020;76:404–10.
Kushima R, Rüthlein HJ, Stolte M, et al. “Pyloric gland-type adenoma” arising in heterotopic gastric mucosa of the duodenum, with dysplastic progression of the gastric type. Virchows Arch. 1999;435:452–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ken Ohata, Shunya Takayanagi, Eiji Sakai, Takashi Muramoto, and Hirotsugu Hashimoto declare that they have no conflict of interest.
Human rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takayanagi, S., Sakai, E., Muramoto, T. et al. Large duodenal pyloric gland adenoma successfully resected by endoscopic submucosal dissection. Clin J Gastroenterol 14, 538–541 (2021). https://doi.org/10.1007/s12328-021-01367-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-021-01367-w