Abstract
Introduction
Currently, there is no clinical prediction model for young patients (≤ 45 years old) with epithelial ovarian cancer (EOC) based on large samples of clinical data. The purpose of this study was to construct nomograms using data extracted from the Surveillance, Epidemiology, and End Results (SEER) Program to predict the overall survival (OS) and cancer-specific survival (CSS) of patients and to further guide the choice of clinical treatment options.
Methods
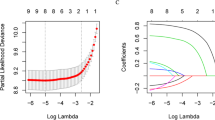
Data from a total of 6376 young patients with EOC collected from 1998 to 2016 were selected from the SEER database. These patients were randomly divided (7:3) into a training cohort (n = 4465) and a validation cohort (n = 1911). Cox and least absolute shrinkage and selection operator (LASSO) analyses were used to select the prognostic factors affecting OS and CSS, and the nomograms of OS and CSS were established. The performance of the nomogram models was assessed by C-index, area under the curve (AUC), calibration curves, and decision curve analysis (DCA). Sample were chosen from patients who underwent surgery in Shengjing Hospital to set external validation. Kaplan–Meier curves were plotted to compare survival outcomes between subgroups.
Results
Nomograms showed good predictive power and clinical practicality. The internal and external validation indicated better performance of the nomograms than the American Joint Committee on Cancer (AJCC) staging system and tumor grade system. Significant differences were observed in the survival curves of different risk subgroups.
Conclusions
We constructed predictive nomograms to evaluate the OS and CSS of young patients with EOC. The nomograms will provide an individualized evaluation of OS and CSS for suitable treatment of young patients with EOC.










Similar content being viewed by others
References
Webb PM, Jordan SJ. Epidemiology of epithelial ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2017;41:3–14.
Torre LA, Trabert B, DeSantis CE, et al. Ovarian cancer statistics, 2018. CA Cancer J Clin. 2018;68(4):284–96.
Prat J. Ovarian carcinomas: five distinct diseases with different origins, genetic alterations, and clinicopathological features. Virchows Arch. 2012;460(3):237–49.
National Cancer Institute. Cancer Stat Facts: Ovarian Cancer. https://seer.cancer.gov/statfacts/html/ovary.html. Accessed February 20, 2019.
Taylan E, Oktay K. Fertility preservation in gynecologic cancers. Gynecol Oncol. 2019;155(3):522–9.
Carter J, Chi DS, Brown CL, et al. Cancer-related infertility in survivorship. Int J Gynecol Cancer. 2010;20(1):2–8.
Fritz R, Jindal S. Reproductive aging and elective fertility preservation. J Ovarian Res. 2018;11(1):66.
Hu J-Q, Yu P-C, Shi X, et al. Prognostic nomograms for predicting overall survival and cancer-specific survival of patients with major salivary gland mucoepidermoid carcinoma. J Cancer. 2019;10(18):4380–8.
Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 2004;10(21):7252–9.
Vickers AJ, Van Calster B, Steyerberg EW. Net benefit approaches to the evaluation of prediction models, molecular markers, and diagnostic tests. BMJ. 2016;352:i6.
Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26(6):565–74.
Heintz APM, Odicino F, Maisonneuve P, et al. Carcinoma of the ovary. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006;95(Suppl 1):S161–92.
Makar AP, Baekelandt M, Tropé CG, Kristensen GB. The prognostic significance of residual disease, FIGO substage, tumor histology, and grade in patients with FIGO stage III ovarian cancer. Gynecol Oncol. 1995;56(2):175–80.
Makar AP, Kisic J, Tropé CG. Controversies in surgical management of advanced ovarian cancer (stage III–IV). Eur J Gynaecol Oncol. 2000;21(5):449–60.
van Meurs HS, Tajik P, Hof MHP, et al. Which patients benefit most from primary surgery or neoadjuvant chemotherapy in stage IIIC or IV ovarian cancer? An exploratory analysis of the European Organisation for Research and Treatment of Cancer 55971 randomised trial. Eur J Cancer. 2013;49(15):3191–3201.
Silverberg SG. Histopathologic grading of ovarian carcinoma: a review and proposal. Int J Gynecol Pathol. 2000;19(1):7–15.
Chan JFK, Shin J, Cheung M, et al. The treatment and outcomes of early-stage epithelial ovarian cancer: have we made any progress? Br J Cancer. 2008;98(7):1191–6.
Trimbos JB, Vergote I, Bolis G, et al. Impact of adjuvant chemotherapy and surgical staging in early-stage ovarian carcinoma: European Organisation for Research and Treatment of Cancer-Adjuvant ChemoTherapy in Ovarian Neoplasm trial. J Natl Cancer Inst. 2003;95(2):113–25.
Wagner U, Harter P, Hilpert F, et al. S3-Guideline on Diagnostics, Therapy and Follow-up of Malignant Ovarian Tumours: Short version 1.0 - AWMF registration number: 032/035OL, June 2013. Geburtshilfe Frauenheilkd. 2013;73(9):874–889.
González Martín A, Redondo A, Jurado M, et al. GEICO (Spanish Group for Investigation on Ovarian Cancer) treatment guidelines in ovarian cancer 2012. Clin Transl Oncol. 2013;15(7):509–25.
du Bois A, Reuss A, Harter P, Pujade-Lauraine E, Ray-Coquard I, Pfisterer J. Potential role of lymphadenectomy in advanced ovarian cancer: a combined exploratory analysis of three prospectively randomized phase III multicenter trials. J Clin Oncol. 2010;28(10):1733–9.
Harter P, Heitz F, Ataseven B, et al. How to manage lymph nodes in ovarian cancer. Cancer. 2019;125(Suppl 24):4573–7.
Chang S-J, Hodeib M, Chang J, Bristow RE. Survival impact of complete cytoreduction to no gross residual disease for advanced-stage ovarian cancer: a meta-analysis. Gynecol Oncol. 2013;130(3):493–8.
Sørensen SM, Schnack TH, Høgdall C. Impact of residual disease on overall survival in women with Federation of Gynecology and Obstetrics stage IIIB-IIIC vs stage IV epithelial ovarian cancer after primary surgery. Acta Obstet Gynecol Scand. 2019;98(1):34–43.
du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer. 2009;115(6):1234–44.
Polterauer S, Vergote I, Concin N, et al. Prognostic value of residual tumor size in patients with epithelial ovarian cancer FIGO stages IIA-IV: analysis of the OVCAD data. Int J Gynecol Cancer. 2012;22(3):380–5.
Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(19):2500–10.
Crafton SM, Cohn DE, Llamocca EN, Louden E, Rhoades J, Felix AS. Fertility-sparing surgery and survival among reproductive-age women with epithelial ovarian cancer in 2 cancer registries. Cancer. 2020;126(6):1217–24.
Wright JD, Shah M, Mathew L, et al. Fertility preservation in young women with epithelial ovarian cancer. Cancer. 2009;115(18):4118–26.
Melamed A, Rizzo AE, Nitecki R, et al. All-cause mortality after fertility-sparing surgery for stage I epithelial ovarian cancer. Obstet Gynecol. 2017;130(1):71–9.
Acknowledgements
Funding
The present study was supported by 345 Talent Project of Shengjing Hospital. The Journal’s Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Liancheng Zhu, Jian Gao and Haoya Xu designed research. Jian Gao and Xianli Li wrote manuscript. Jian Gao, Haoya Xu, Xianli Li, Shengtan Wang, Limei Yan, Feifei Li and Liancheng Zhu involved in data collection and data statistical analysis. Liancheng Zhu provided fund support and critically reviewed the manuscript. All authors read and approved the final manuscript.
Compliance with Ethics Guidelines
The studies involving human participants were reviewed and approved by Shengjing Hospital of China Medical University and were conducted in accordance with the Declaration of Helsinki.
Disclosures
Jian Gao, Shengtan Wang, Feifei Li, Haoya Xu, Xianli Li, Limei Yan, and Liancheng Zhu confirm that they have no conflicts of interest to declare.
Data Availability
All of the material is owned by the corresponding authors. The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request (Liancheng Zhu, email: medecin@126.com).
Consent for Publication
The results/data/figures in this manuscript have not been published elsewhere, nor are they under consideration by another publisher.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gao, J., Wang, S., Li, F. et al. Nomograms for Predicting Overall Survival and Cancer-Specific Survival of Young Patients with Epithelial Ovarian Cancer: Analysis Based on SEER Program. Adv Ther 39, 257–285 (2022). https://doi.org/10.1007/s12325-021-01955-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01955-9