Abstract
Introduction
To investigate the efficacy of retinal electromagnetic stimulation and sub-tenon autologous platelet-rich plasma in the treatment of deep retinal capillary ischemia.
Methods
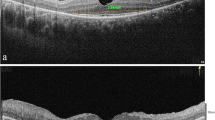
The study included 28 eyes of 17 patients aged 15–76 years (mean 37.9 years) who had deep retinal capillary ischemia. Patients who had acute-onset paracentral scotoma in the last 1 month were included in the study between January 2018 and January 2019. The diagnosis of deep retinal capillary ischemia was based on clinical history and typical findings of optical coherence tomography angiography. The eyes were divided into three groups: group 1 (n = 7 eyes) received electromagnetic stimulation alone; group 2 (n = 7 eyes) received electromagnetic stimulation and sub-tenon autologous platelet-rich plasma injection; group 3 had no intervention and served as a control group (n = 14 eyes). The patients underwent ten sessions of electromagnetic stimulation in groups 1 and 2. Sub-tenon autologous platelet-rich plasma injection was performed immediately after the first, fifth, and tenth sessions of electromagnetic stimulation in group 2. The deep retinal capillary density and best corrected visual acuity changes were investigated before and after treatment at the first month.
Results
The mean deep retinal capillary density was 52.0% before electromagnetic stimulation and 56.1% after ten sessions of application in group 1; this improvement was statistically significant (p = 0.01). In the combined treatment group (group 2), the mean deep retinal capillary density was 46.9% before the treatment and 56.5% after the treatment; this increase was also statistically significant (p = 0.01). Statistically significant best corrected visual acuity improvement (p = 0.01) could be achieved only in group 2. The combined treatment was significantly superior (p < 0.01) to treatment with only electromagnetic stimulation regarding best corrected visual acuity and deep retinal capillary density. In the control group (group 3), there was no statistically significant change (p = 0.09) in the mean deep retinal capillary density and best corrected visual acuity.
Conclusion
Treatment of the underlying cause is a priority in the treatment of deep retinal capillary ischemia. However, in the acute period, local ischemia treatment is necessary to prevent permanent retinal damage and scotomas. In mild cases, only electromagnetic stimulation, which is non-invasive and easy to use, might have a beneficial effect on deep retinal capillary density. In more severe cases, sub-tenon fresh autologous platelet-rich plasma injection together with electromagnetic stimulation may be more effective in the treatment of local ischemia of the retina in order to augment the response.
Funding
The Rapid Service Fees were funded by the Ankara University Tecnopolis Institute.
Clinical Trial Registration
titck.gov.tr identifier, 2018-136.



Similar content being viewed by others
References
Campbell JP, Zhang M, Hwang TS, et al. Detailed vascular anatomy of the human retina by projection-resolved optical coherence tomography angiography. Scientific Rep. 2017. https://doi.org/10.1038/srep42201.
Tan PEZ, Yu PK, Balaratnasingam C, et al. Quantitative confocal imaging of the retinal microvasculature in the human retina. Investig Opthalmol Vis Sci. 2012;53(9):5728. https://doi.org/10.1167/iovs.12-10017.
Park JJ, Soetikno BT, Fawzi AA. Characterization of the middle capillary plexus using optical coherence tomography angiography in healthy and diabetic eyes. Retina. 2016;36:2039–50.
Linsenmeier RA, Zhang HF. Retinal oxygen: from animals to humans. Prog Retin Eye Res. 2017;58:115–51.
Rahimy E, Sarraf D. Paracentral acute middle maculopathy: spectral domain optical coherence tomography feature of deep capillary ischemia. Curr Opin Ophthalmol. 2014;25:207.
Sarraf D, Rahimy E, Fawzi AA, et al. Paracentral acute middle maculopathy. JAMA Ophthalmol. 2013;131(10):1275. https://doi.org/10.1001/jamaophthalmol.2013.4056.
Niyousha MR, Hassanpoor N, Eftekhari A, Mousvi F. Simultaneous paracentral acute middle maculopathy and Purtscher-like retinopathy after acute febrile illness. Can J Ophthalmol. 2018;53(5):e184–6. https://doi.org/10.1016/j.jcjo.2017.11.020.
Nemiroff J, Phasukkijwatana N, Sarraf D. Optical coherence tomography angiography of deep capillary ischemia. Dev Ophthalmol. 2016;56:139–45.
Kulikov AN, Maltsev DS, Leongardt TA. Retinal microvasculature alteration in paracentral acute middle maculopathy and acute macular neuroretinopathy. Retin Cases Br Rep. 2018. https://doi.org/10.1097/icb.0000000000000709.
Nakashima H, Iwama Y, Tanioka K, Emi K. Paracentral acute middle maculopathy following vitrectomy for proliferative diabetic retinopathy. Ophthalmology. 2018. https://doi.org/10.1016/j.ophtha.2018.07.006.
McLeod D. En face optical coherence tomography analysis to assess the spectrum of perivenular ischemia and paracentral acute middle maculopathy in retinal vein occlusion. Am J Ophthalmol. 2017;182:203–4.
Rahimy E, Kuehlewein L, Sadda SR, Sarraf D. Paracentral acute middle maculopathy. Retina. 2015;35:1921–30.
Nemiroff J, Kuehlewein L, Rahimy E, et al. Assessing deep retinal capillary ischemia in paracentral acute middle maculopathy by optical coherence tomography angiography. Am J Ophthalmol. 2016;162:121–32.
Bhavsar KV, Lin S, Rahimy E, et al. Acute macular neuroretinopathy: a comprehensive review of the literature. Surv Ophthalmol. 2016;61(5):538–65. https://doi.org/10.1016/j.survophthal.2016.03.003.
Introini U, Casalino G, Querques G, Bagini M, Bandello F. Acute macular neuroretinopathy following intranasal use of cocaine. Acta Ophthalmol. 2015;93(3):e239–40.
Munk MR, Jampol LM, Cunha Souza E, et al. New associations of classic acute macular neuroretinopathy. Br J Ophthalmol. 2015;100(3):389–94. https://doi.org/10.1136/bjophthalmol-2015-306845.
Li M, Zhang X, Ji Y, Ye B, Wen F. Acute macular neuroretinopathy in dengue fever: short-term prospectively followed up case series. JAMA Ophthalmol. 2015;133(11):1329–33.
Koenekoop RK. Why some photoreceptors die while others remain dormant: lessons from RPE65 and LRAT associated retinal dystrophies. Ophthalmic Genet. 2011;32(2):126–8.
Wang W, Lee SJ, Scott PA, et al. Two-step reactivation of dormant cones in retinitis pigmentosa. Cell Rep. 2016;15(2):372–85.
Sabharwala J, Seilheimera RL, Taoc X, Cowanc CS, Frankfortb BJ, Wub SM. Elevated IOP alters the space/time profiles in the center and surround of both ON and OFF RGCs in mouse. PNAS. 2017;114(33):8859–64.
Lavia C, Bonnin S, Maule M, Erginay A, Tadayoni R, Gaudric A. Vessel density of superficial, intermediate, and deep capillary plexuses using optical coherence tomography angiography. Retina. 2019;39(2):247–58. https://doi.org/10.1097/iae.000000000000241.
Notodihardjo SC, Morimoto N, Kakudo N, et al. Comparison of the efficacy of cryopreserved human platelet lysate and refrigerated lyophilized human platelet lysate for wound healing. Regen Ther. 2019;10:1–9. https://doi.org/10.1016/j.reth.2018.10.003.
Zahn J, Loibl M, Sprecher C, et al. Platelet-rich plasma as an autologous and proangiogenic cell delivery system. Mediat Inflamm. 2017;2017:1–14. https://doi.org/10.1155/2017/1075975.
Armulik A. Endothelial/pericyte interactions. Circ Res. 2005;97(6):512–23. https://doi.org/10.1161/01.res.0000182903.16652.d7.
Benjamin LE, Hemo I, Keshet E. A plasticity window for blood vessel remodelling is defined by pericyte coverage of the preformed endothelial network and is regulated by PDGF-B and VEGF. Development. 1998;125:1591–8.
Arslan U, Özmert E, Demirel S, Örnek F, Şermet F. Effects of subtenon-injected autologous platelet-rich plasma on visual functions in eyes with retinitis pigmentosa: preliminary clinical results. Graefes Arch Clin Exp Ophthalmol. 2018;256(5):893–908. https://doi.org/10.1007/s00417-018-3953-5.
Klomjai W, Katz R, Lackmy-Vallée A. Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS). Ann Phys Rehabil Med. 2015;58(4):208–13. https://doi.org/10.1016/j.rehab.2015.05.005.
Zhang N, Xing M, Wang Y, Tao H, Cheng Y. Repetitive transcranial magnetic stimulation enhances spatial learning and synaptic plasticity via the VEGF and BDNF–NMDAR pathways in a rat model of vascular dementia. Neuroscience. 2015;311:284–91. https://doi.org/10.1016/j.neuroscience.2015.10.038.
Luo J, Zheng H, Zhang L, et al. High-frequency repetitive transcranial magnetic stimulation (rTMS) improves functional recovery by enhancing neurogenesis and activating BDNF/TrkB signaling in ischemic rats. Int J Mol Sci. 2017;18(2):455. https://doi.org/10.3390/ijms18020455.
Wang F, Zhang C, Hou S, Geng X. Synergistic effects of mesenchymal stem cell transplantation and repetitive transcranial magnetic stimulation on promoting autophagy and synaptic plasticity in vascular dementia. J Gerontol Ser A. 2018. https://doi.org/10.1093/gerona/gly221.
Webster K, Ro T. Retinal and visual cortex distance from transcranial magnetic stimulation of the vertex affects phosphene perception. Exp Brain Res. 2017;235(9):2857–66. https://doi.org/10.1007/s00221-017-5022-4.
Nikolaeva NV, Bolotova NV, Kamenskikh TG, Raĭgorodskiĭ IuM, Kolbenev IO, Luk’ianov VF. Transcranial magnetotherapy for the correction of initial manifestations of diabetic retinopathy in children. Vopr Kurortol Fizioter Lech Fiz Kult. 2009;3:25–8.
Chandra T, Chavhan GB, Sze RW, et al. Practical considerations for establishing and maintaining a magnetic resonance imaging safety program in a pediatric practice. Pediatr Radiol. 2019;49(4):458–68. https://doi.org/10.1007/s00247-019-04359-8.
Heintz PH, Sandoval DJ, Chambers GD, Adolphi NL. Biological effects of magnetic resonance imaging. In: Kelsey CA, Heintz PH, Sandoval MS, et al., editors. Radiation biology of medical imaging. Hoboken: Wiley; 2018. p. 281–95.
Sridhar J, Shahlaee A, Rahimy E, et al. Optical coherence tomography angiography and en face optical coherence tomography features of paracentral acute middle maculopathy. Am J Ophthalmol. 2015;160(6):1259–1268.e2. https://doi.org/10.1016/j.ajo.2015.09.016.
Colafrancesco V, Coassin M, Rossi S, Aloe L. Effect of eye NGF administration on two animal models of retinal ganglion cells degeneration. Ann 1st Super Sanita. 2011;47:284–9.
Lambiase A, Aloe L, Centofanti M, et al. Experimental and clinical evidence of neuroprotection by nerve growth factor eye drops: implications for glaucoma. Proc Natl Acad Sci USA. 2009;106:13469–74.
Lambiase A, Mantelli F, Sacchetti M, Rossi S, Aloe L, Bonini S. Clinical applications of NGF in ocular diseases. Arch Ital Biol. 2011;149:283–92.
Mysona BA, Zhao J, Bollinger KE. Role of BDNF/TrkB pathway in the visual system: therapeutic implications for glaucoma. Expert Rev Ophthalmol. 2017;12(1):69–81.
Giannos SA, Kraft ER, Zhao ZY, Merkley KH, Cai J. Photokinetic drug delivery: near infrared (NIR) induced permeation enhancement of bevacizumab, ranibizumab and aflibercept through human sclera. Pharm Res. 2018;35(6):1. https://doi.org/10.1007/s11095-018-2392-7.
Demetriades AM, Deering T, Liu H, et al. Trans-scleral delivery of antiangiogenic proteins. J Ocul Pharmacol Ther. 2008;24(1):70–9. https://doi.org/10.1089/jop.2007.0061.
Meng T, Kulkarni V, Simmers R, Brar V, Xu Q. Therapeutic implications of nanomedicine for ocular drug delivery. Drug Discov Today. 2019. https://doi.org/10.1016/j.drudis.2019.05.00.
Li SK, Hao J. Transscleral passive and iontophoretic transport: theory and analysis. Expert Opin Drug Deliv. 2017;15(3):283–99. https://doi.org/10.1080/17425247.2018.1406918.
Joseph RR, Tan DWN, Ramon MRM, et al. Characterization of liposomal carriers for the trans-scleral transport of ranibizumab. Scientific Rep. 2017;7(1):1. https://doi.org/10.1038/s41598-017-16791-7.
Marg E. Magnetostimulation of vision: direct noninvasive stimulation of the retina and the visual brain. Optom Vis Sci. 1991;68(6):427–40.
Bagattini C, Mazzi C, Savazzi S. Waves of awareness for occipital and parietal phosphenes perception. Neuropsychologia. 2015;70:114–25. https://doi.org/10.1016/j.neuropsychologia.2015.02.
Kammer T, Beck S. Phosphene thresholds evoked by transcranial magnetic stimulation are insensitive to short-lasting variations in ambient light. Exp Brain Res. 2002;145(3):407–10. https://doi.org/10.1007/s00221-002-1160-3.
Marzi CA, Mancini F, Savazzi S. Interhemispheric transfer of phosphenes generated by occipital versus parietal transcranial magnetic stimulation. Exp Brain Res. 2008;192(3):431–41. https://doi.org/10.1007/s00221-008-1496-4.
Drakon AK, Elfimov MA, Illarionov VE, Ivanova II, Portnov VV. Contemporary potential of nonmedical treatment in ophthalmology. Med Tr Prom Ekol. 2016;2:6–11.
Lim LA, Frost NA, Powell RJ, Hewson P. Comparison of the ETDRS logMAR, “compact reduced logMAR” and Snellen charts in routine clinical practice. Eye (Lond). 2010;24(4):673–7.
Acknowledgements
We thank the participants of the study.
Funding
No funding or sponsorship was received for this study and the Rapid Service Fees were funded by the Ankara University Tecnopolis Institute. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Medical Writing Assistance
Medical writing and editorial assistance was provided by Ali Hariri from the American Manuscript Editors Company, which was funded by the authors.
Compliance with Ethics Guidelines
Ethics committee approval for the transcranial electromagnetic stimulation study was obtained from the Ankara University Faculty of Medicine Clinical Research Ethics Committee (17-1177-18) as well as and Review Board of the Drug and Medical Device Department within the Turkish Ministry of Health (2018-136). These committees had already approved the aPRP work (12-595-16 and 16-AKD-30). The study was performed in accordance with the tenets of the 1964 Declaration of Helsinki. Written informed consent was obtained from the patients prior to enrollment.
Disclosures
Emin Özmert and Umut Arslan have nothing to declare.
Data Availability
The datasets generated during and/or analysed during the study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.8964386.
Rights and permissions
About this article
Cite this article
Özmert, E., Arslan, U. Management of Deep Retinal Capillary Ischemia by Electromagnetic Stimulation and Platelet-Rich Plasma: Preliminary Clinical Results. Adv Ther 36, 2273–2286 (2019). https://doi.org/10.1007/s12325-019-01040-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-019-01040-2