Abstract
Introduction
Type 2 diabetes is an increasing problem in China, yet there is a paucity of data regarding the cost-effectiveness of pharmacological interventions in the Chinese setting.
Methods
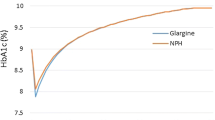
Previous data were obtained from PRESENT (Physicians’ Routine Evaluation of Safety and Efficacy of NovoMix 30 Therapy), a multicountry, single-arm, observational study where type 2 diabetes patients poorly controlled with biphasic human insulin (BHI) were converted to biphasic insulin aspart 30 (BIAsp30); the Chinese subgroup experienced an improvement in HbA1c and a reduction in hypoglycaemic events. A published and validated computer simulation model of diabetes (the CORE Diabetes Model) was used to estimate the long-term clinical and cost consequences of switching to BIAsp30 from BHI in the Chinese setting. Treatment effects and patient characteristics were derived from PRESENT and countryspecific published sources. Primary research was performed to ascertain patient management practices and diabetes-related complication costs. Risks of modelled complications were derived from landmark clinical trials and epidemiological studies. Costs and clinical projections were made over patient lifetimes from a third-party payer perspective and discounted at 3% annually. Extensive sensitivity analyses were performed.
Results
Conversion to BIAsp30 from BHI was projected to improve discounted life expectancy by 0.38 years per patient (9.91 vs 9.53 years) and quality-adjusted life expectancy by 0.91 quality-adjusted life years (QALYs) per patient (6.32 vs 5.41 QALYs). Conversion to BIAsp30 was associated with increased direct medical costs of Chinese Yuan (CNY) 1751 per patient, due to higher pharmacy and management costs (CNY +19,007), offset by reduced diabetes-related complication costs (CNY −17,254) over patient lifetimes. BIAsp30 was associated with an incremental cost-effectiveness ratio of CNY 1926 per QALY gained.
Conclusion
BIAsp30 was projected to substantially improve clinical outcomes but was associated with increased lifetime medical costs. BIAsp30 would be considered cost-effective in China given a willingness-to-pay threshold of CNY 100,000 per QALY gained in type 2 diabetes patients poorly controlled on BHI.
Similar content being viewed by others
References
Roglic G, Unwin N, Bennett PH, et al. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care. 2005;28:2130–2135.
Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053.
King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–1431.
International Diabetes Federation. Diabetes Atlas. 3rd edition. Brussels: International Diabetes Federation; 2007.
Popkin BM. Nutrition in transition: the changing global nutrition challenge. Asia Pac J Clin Nutr. 2001;10(suppl):S13–S18.
Zhao W, Chen J. Implications from and for food cultures for cardiovascular disease: diet, nutrition and cardiovascular diseases in China. Asia Pac J Clin Nutr. 2001;10:146–152.
The maladies of affluence. The Economist. 9 August 2007. Available at: www.economist.com/world/international/displaystory.cfm?story_id=9616897. Accessed 2007.
Jia WP, Pang C, Chen L, et al. Epidemiological characteristics of diabetes mellitus and impaired glucose regulation in a Chinese adult population: the Shanghai Diabetes Studies, a crosssectional 3-year follow-up study in Shanghai urban communities. Diabetologia. 2007;50:286–292.
Dong Y, Gao W, Nan H, et al. Prevalence of type 2 diabetes in urban and rural Chinese populations in Qingdao, China. Diabet Med. 2005;22:1427–1433.
World Health Organization. Diabetes is a common condition and its frequency is dramatically rising all over the world. Available at: www.who.int/diabetes/commoncondition/en. Accessed 2008.
Chan JC, Ng MC, Critchley JA, et al. Diabetes mellitus-a special medical challenge from a Chinese perspective. Diabetes Res Clin Pract. 2001;54(suppl 1):S19–S27.
Economic consequences of diabetes mellitus in the U.S. in 1997. American Diabetes Association. Diabetes Care. 1998;21:296–309.
Jonsson B. Revealing the cost of type II diabetes in Europe. Diabetologia. 2002;45:S5–S12.
Chen XB, Tang L, Chen HY. Assessing the impact of complications on the costs of type 2 diabetes in urban China. Chin J Diabetes. 2003;11:238–241.
Xie X, Vondeling H. Cost-utility analysis of intensive blood glucose control with metformin versus usual care in overweight type 2 diabetes mellitus patients in Beijing, P.R. China. Value Health. 2008;11(suppl 1):S23–S32.
American Diabetes Association. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31:596–615.
Vora JP, Ibrahim HA, Bakris GL. Responding to the challenge of diabetic nephropathy: the historic evolution of detection, prevention and management. J Hum Hypertens. 2000;14:667–685.
Ray JA, Valentine WJ, Secnik K, et al. Review of the cost of diabetes complications in Australia, Canada, France, Germany, Italy and Spain. Curr Med Res Opin. 2005;21:1617–1629.
IDF Clinical Guidelines Task Force. Global Guideline for Type 2 Diabetes. Brussels: International Diabetes Federation; 2005.
The DCCT Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–986.
The UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–853.
Nathan DM, Buse JB, Davidson MB, et al. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006;29:1963–1972.
Smith SA, Murad MH. Review: long-acting insulin analogues do not improve glycaemic control but reduce nocturnal hypoglycaemia. Evid Based Med. 2008;13:79.
Bolli GB, Di Marchi RD, Park GD, et al. Insulin analogues and their potential in the management of diabetes mellitus. Diabetologia. 1999;42:1151–1167.
Dimitriadis GD, Gerich JE. Importance of timing of preprandial subcutaneous insulin administration in the management of diabetes mellitus. Diabetes Care. 1983;6:374–377.
Siebenhofer A, Plank J, Berghold A, et al. Short acting insulin analogues versus regular human insulin in patients with diabetes mellitus. Cochrane Database Syst Rev. 2006;(19):CD003287.
Shestakova M, Sharma SK, Almustafa M, et al. Transferring type 2 diabetes patients with uncontrolled glycaemia from biphasic human insulin to biphasic insulin aspart 30: experiences from the PRESENT study. Curr Med Res Opin. 2007;23:3209–3214.
Khutsoane D, Sharma SK, Almustafa M, et al. Biphasic insulin aspart 30 treatment improves glycaemic control in patients with type 2 diabetes in a clinical practice setting: experience from the PRESENT study. Diabetes Obes Metab. 2008;10:212–222.
Sharma SK, Al-Mustafa M, Oh SJ, et al. Biphasic insulin aspart 30 treatment in patients with type 2 diabetes poorly controlled on prior diabetes treatment: results from the PRESENT study. Curr Med Res Opin. 2008;24:645–652.
Gao Y, Guo XH, Vaz JA, et al. Biphasic insulin aspart 30 treatment improves glycaemic control in patients with type 2 diabetes in a clinical practice setting: Chinese PRESENT study. Diabetes Obes Metab. 2008; May 20. In press.
Palmer AJ, Roze S, Valentine WJ, et al. The CORE Diabetes Model: projecting long-term clinical outcomes, costs and costeffectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20:S5–S26.
Palmer AJ, Roze S, Valentine W, et al. Validation of the CORE Diabetes Model against epidemiological and clinical studies. Curr Med Res Opin. 2004;20:S27–S40.
Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412.
Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703–713.
Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–419.
Stevens RJ, Kothari V, Adler AI, et al. The UKPDS risk engine: a model for the risk of coronary heart disease in type II diabetes (UKPDS 56). Clin Sci (Lond). 2001;101:671–679.
Kothari V, Stevens RJ, Adler AI, et al. UKPDS 60: risk of stroke in type 2 diabetes estimated by the UK Prospective Diabetes Study risk engine. Stroke. 2002;33:1776–1781.
UK Prospective Diabetes Study Group. U.K. Prospective Diabetes Study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes. 1995;44:1249–1258.
D’Agostino RB, Russell MW, Huse DM, et al. Primary and subsequent coronary risk appraisal: new results from the Framingham study. Am Heart J. 2000;139:272–281.
World Health Organization. Life tables for 191 countries. World mortality in 2005. Available at: www3.who.int/whosis/life_tables/life_tables.cfm 2007. Accessed 2008.
World Health Organization. Global burden of disease estimates. 2004. Available at: www. who.int/healthinfo/bodestimates/en/index.html. Accessed 2008.
Annemans L, Demarteau N, Hu S, et al. An Asian regional analysis of costeffectiveness of early irbesartan treatment versus conventional antihypertensive, late amlodipine, and late irbesartan treatments in patients with type 2 diabetes, hypertension, and nephropathy. Value Health. 2008;3:354–364.
Lin S. Nephrology in China: a great mission and momentous challenge. Kidney Int Suppl. 2003;(83):S108–S110.
Thomas GN, Critchley JA, Tomlinson B, et al. Peripheral vascular disease in type 2 diabetic Chinese patients: associations with metabolic indices, concomitant vascular disease and genetic factors. Diabet Med. 2003;20:988–995.
Xu L, Xie X, Wang S, et al. Prevalence of diabetes mellitus in China. Exp Clin Endocrinol Diabetes. 2008;116:69–70.
Valentine WJ, Palmer AJ, Nicklasson L, et al. Improving life expectancy and decreasing the incidence of complications associated with type 2 diabetes: a modelling study of HbA1c targets. Int J Clin Pract. 2006;60:1138–1145.
Hsiao WC. The Chinese health care system: lessons for other nations. Soc Sci Med. 1995;41:1047–1055.
Currie CJ, Morgan CL, Poole CD, et al. Multivariate models of health-related utility and the fear of hypoglycaemia in people with diabetes. Curr Med Res Opin. 2006;22:1523–1534.
International Society for Pharmacoeconomics and Outcomes Research. Chinese Medical Doctor Association Pharmacoeconomics Chapter. Pharmacoeconomic Guidelines. ISPOR 2005. Available at: www.pe-cn.org/en/pe_guidelines/index.asp. Accessed 2008.
World Health Organization. Making Choices in Health: WHO Guide to Cost-Effectiveness Analysis. Geneva: World Health Organization; 2003.
Barzi F, Patel A, Gu D, et al. Cardiovascular risk prediction tools for populations in Asia. J Epidemiol Community Health. 2007;61:115–121.
Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ. 1997;6:327–340.
World Health Organization. Report on Macroeconomics and Health: Investing in Health for Economic Development. Geneva: World Health Organization; 2001.
Central Intelligence Agency. The 2008 World Factbook. Washington: Central Intelligence Agency; 2008.
Yuan Y, Iloeje U, Li H, et al. Economic implications of entecavir treatment in suppressing viral replication in chronic hepatitis B (CHB) patients in China from a perspective of the Chinese Social Security program. Value Health. 2008;11(suppl 1):S11–S22.
Xue JL, Ma JZ, Louis TA, Collins AJ. Forecast of the number of patients with end-stage renal disease in the United States to the year 2010. J Am Soc Nephrol. 2001;12:2753–2758.
Chirakup S, Chaiyakunapruk N, Chaikledkeaw U, et al. Cost-effectiveness analysis of thiazolidinediones in uncontrolled type 2 diabetic patients receiving sulfonylureas and metformin in Thailand. Value Health. 2008;11(suppl 1):S43–S51.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Palmer, J.L., Gibbs, M., Scheijbeler, H.W. et al. Cost-effectiveness of switching to biphasic insulin aspart in poorly-controlled type 2 diabetes patients in China. Adv Therapy 25, 752–774 (2008). https://doi.org/10.1007/s12325-008-0080-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-008-0080-4