Abstract
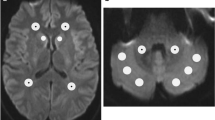
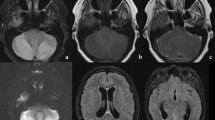
To develop a radiological score system to assess the severity of acute cerebellitis (AC) and to compare radiological severity score at the onset to cerebellar atrophy at follow-up. Clinical and MRI findings were recorded in 16 patients with AC. Radiological severity score considering topographic patterns, gray/white matter involvement, enhancement, tonsillar herniation or hydrocephalus development and clinical severity score taking into account clinical symptoms were assessed for each patient at the onset of the symptoms. Radiological and neurological sequelae were assessed at follow-up. At symptoms onset, clinical severity scale ranged from mild to severe and radiological severity score ranged from 3 to 7 with higher scores indicating a greater severity. The cut-off value of 5 for radiological score well segregated severe patients defined by clinical scale. A significant correlation between clinical scale and radiological severity scores (p < 0.001, r = 0.75) was found. At follow-up visit, all children developed cerebellar atrophy and 5 children showed neurologic sequelae while adults showed complete resolution without atrophy. Patients in whom atrophy was not observed had both older ages (p < 0.001) and a focal cerebellar involvement (p = 0.03). In patients with AC, radiological severity score may be a useful tool in evaluating clinical severity, but it is not capable to predict neither neurological sequelae nor evolution towards atrophy. Cerebellar atrophy, observed in children with AC, may be caused by several factors such as the age of patient and the extension of cerebellar involvement and it may be counterbalanced by neuronal restoring processes due to neuroplasticity.



Similar content being viewed by others
References
Emelifeonwu JA, Shetty J, Kaliaperumal C, Gallo P, Sokol D, Soleiman H, et al. Acute cerebellitis in children: a variable clinical entity. J Child Neurol. 2018;33:675–84.
De Bruecker Y, Claus F, Demaerel P, Ballaux F, Sciot R, Lagae L, et al. MRI findings in acute cerebellitis. Eur Radiol. 2004;14:1478–83.
Van Samkar A, Poulsen MNF, Bienfait HP, Van Leeuwen RB. Acute cerebellitis in adults: a case report and review of the literature. BMC Res Notes. 2017;10:610.
Bozzola E, Bozzola M, Tozzi AE, Calcaterra V, Longo D, Krzystofiak A, et al. Acute cerebellitis in varicella: a ten year case series and systematic review of the literature. Ital J Pediatr. 2014;40:57.
Tlili-Graiess K, Mhiri Souei M, Mlaiki B, Arifa N, Moulahi H, Jemni Gharbi H, et al. Imaging of acute cerebellitis in children. Report of 4 cases. J Neuroradiol. 2006;33:38–44.
Paketci C, Edem P, Okumus C, Sarioglu FC, Bayram E, Hiz S, et al. Herpes simplex virus-1 as a rare etiology of isolated acute cerebellitis: case report and literature review. J Neuro-Oncol. 2020;26:270–2.
Gruis KL, Moretti P, Gebarski SS, Mikol DD. Cerebellitis in an adult with abnormal magnetic resonance imaging findings prior to the onset of ataxia. Arch Neurol. 2003;60:877–80.
Nussinovitch M, Prais D, Volovitz B, Shapiro R, Amir J. Post-infectious acute cerebellar ataxia in children. Clin Pediatr (Phila). 2003;42:581–4.
Al-Shokri SD, Karumannil SA, Mohammed SS, Sadek MS. Post-Epstein-Barr virus acute cerebellitis in an adult. Am J Case Rep. 2020;21:e918567.
Donmez FY, Agildere AM, Tore HG, Ure S, Benli S. Abnormal diffusion-weighted imaging findings in an adult patient with acute cerebellitis presenting with a normal magnetic resonance imaging. J Comput Assist Tomogr. 2008;32:156–8.
Yildirim M, Gocmen R, Konuskan B, Parlak S, Yalnizoglu D, Anlar B. Acute cerebellitis or postinfectious cerebellar ataxia? Clinical and imaging features in acute cerebellitis. J Child Neurol. 2020;35:380–8.
Kornreich L, Shkalim-Zemer V, Levinsky Y, Abdallah W, Ganelin-Cohen E, Straussberg R. Acute cerebellitis in children: a many-faceted disease. J Child Neurol. 2016;31:991–7.
Alomani H, Arshad M, Elzonfly M, Aldakhil AA, Alharbi AH, Alasqah A, et al. Pediatric fulminant cerebellitis is still a fatal disease that we know little about! Two case reports and a literature review. Am J Case Rep. 2021;22:e928370.
Hacohen Y, Niotakis G, Aujla A, Siddiqui A, McCormick D, Bassi S, et al. Acute life threatening cerebellitis presenting with no apparent cerebellar signs. Clin Neurol Neurosurg. 2011;113:928–30.
Patel P, Rayamajhi S, Tokala H, Laird-Fick H. An unusual cause of altered mental status in elderly-acute cerebellitis: a case report and review. Case Rep Med. 2013;2013:653925.
Carceller Lechón F, Duat Rodríguez A, Sirvent Cerdá SI, Khabra K, de Prada I, García-Peñas JJ, et al. Hemicerebellitis: report of three paediatric cases and review of the literature. Eur J Paediatr Neurol EJPN Off J Eur Paediatr Neurol Soc. 2014;18:273–81.
Bakshi R, Bates VE, Kinkel PR, Mechtler LL, Kinkel WR. Magnetic resonance imaging findings in acute cerebellitis. Clin Imaging. 1998;22:79–85.
Adachi M, Kawanami T, Ohshima H, Hosoya T. Cerebellar atrophy attributed to cerebellitis in two patients. Magn Reson Med Sci MRMS Off J Jpn Soc Magn Reson Med. 2005;4:103–7.
Venkatesh M, Chakkalakkoombil SV, Duraipandi MB, Gulati R. Complicated acute cerebellitis with obstructive hydrocephalus and tonsillar herniation in a child. BMJ Case Rep. 2017;2017:bcr-2017-219337.
Cohen JE, Gomori M, Benifla M, Itshayek E, Shoshan Y. Acute pseudotumoral hemicerebellitis: diagnosis and neurosurgical considerations of a rare entity. J Clin Neurosci Off J Neurosurg Soc Australas. 2014;21:337–9.
Van Lierde A, Righini A, Tremolati E. Acute cerebellitis with tonsillar herniation and hydrocephalus in Epstein-Barr virus infection. Eur J Pediatr. 2004;163:689–91.
Lancella L, Esposito S, Galli ML, Bozzola E, Labalestra V, Boccuzzi E, et al. Acute cerebellitis in children: an eleven year retrospective multicentric study in Italy. Ital J Pediatr. 2017;43:54.
Hirayama K, Sakazaki H, Murakami S, Yonezawa S, Fujimoto K, Seto T, et al. Sequential MRI, SPECT and PET in respiratory syncytial virus encephalitis. Pediatr Radiol. 1999;29:282–6.
Kubota T, Suzuki T, Kitase Y, Kidokoro H, Miyajima Y, Ogawa A, et al. Chronological diffusion-weighted imaging changes and mutism in the course of rotavirus-associated acute cerebellitis/cerebellopathy concurrent with encephalitis/encephalopathy. Brain and Development. 2011;33:21–7.
Tang Y, Suddarth B, Du X, Matsumoto JA. Reversible diffusion restriction of the middle cerebellar peduncles and dentate nucleus in acute respiratory syncytial virus cerebellitis: a case report. Emerg Radiol. 2014;21:89–92.
Kizilkilic O, Karaca S. Influenza-associated encephalitis-encephalopathy with a reversible lesion in the splenium of the corpus callosum: case report and literature review. AJNR Am J Neuroradiol. 2004;25:1863–4.
Mori T, Morii M, Kuroiwa Y, Hotsubo T, Fuse S, Tsustumi H. Rotavirus encephalitis and cerebellitis with reversible magnetic resonance signal changes. Pediatr Int Off J Jpn Pediatr Soc. 2011;53:252–5.
Hayakawa H, Katoh T. Severe cerebellar atrophy following acute cerebellitis. Pediatr Neurol. 1995;12:159–61.
Karmon Y, Inbar E, Cordoba M, Gadoth N. Paraneoplastic cerebellar degeneration mimicking acute post-infectious cerebellitis. Cerebellum Lond Engl. 2009;8:441–4.
Hennes E, Zotter S, Dorninger L, Hartmann H, Häusler M, Huppke P, et al. Long-term outcome of children with acute cerebellitis. Neuropediatrics. 2012;43:240–8.
Pilato F, Dileone M, Capone F, Profice P, Caulo M, Battaglia D, et al. Unaffected motor cortex remodeling after hemispherectomy in an epileptic cerebral palsy patient. A TMS and fMRI study. Epilepsy Res. 2009;85:243–51.
Bonaventura E, Purpura G, Pasquariello R, Da Prato S, Di Lieto MC, Barsotti J, et al. Complex neurodevelopmental disorder in a preterm child with unilateral cerebellar hemorrhage. Appl Neuropsychol. Child. 2021;1–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
We declare that all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
Rosalinda Calandrelli declares that she has no conflict of interest. Marco Panfili declares that he has no conflict of interest. Huong Elena Tran declares that she has no conflict of interest. Cesare Colosimo declares that he is a scientific consultant for Bracco Diagnostics Inc. and Bayer HealthCare. Fabio Pilato declares that he has no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calandrelli, R., Marco, P., Tran, H.E. et al. A Novel Radiological Score System to Assess the Clinical Severity in Patients with Acute Cerebellitis. Cerebellum 22, 173–182 (2023). https://doi.org/10.1007/s12311-022-01377-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-022-01377-5