Abstract
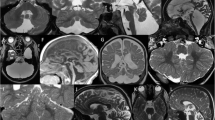
Cerebellar cysts may be seen in selected genetic disorders and acquired anomalies. Here, we review our experience, excluding cystic tumors and parasitic cysts. The pathogenesis is heterogeneous: Cysts may involve/represent normal structures (e.g., Virchow-Robin spaces), be “destructive” (such as in some types of pontocerebellar hypoplasias), “malformative” (such as in some forms of congenital muscular dystrophies and GPR56-related migration disorders), or “disruptive” (such as in some cerebellar dysplasias). The provided checklist may be useful in deciding targeted diagnostic workup.








Similar content being viewed by others
References
Poretti A, Boltshauser E. Cerebellar cysts and neuroimaging in congenital muscular dystrophies. In: Boltshauser E, Schmahmann JD, editors. Cerebellar disorders in children. London: MacKeith Press; 2012. p. 177–83.
Barkovich AJ, Raybaud C. Pediatric neuroimaging. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2012.
Osborn AG. Osborn’s brain: imaging, pathology, and anatomy. Philadelphia: Lippincott Williams & Wilkins; 2012.
Nickerson JP, Richner B, Santy K, et al. Neuroimaging of pediatric intracranial infection-part 2: TORCH, viral, fungal, and parasitic infections. J Neuroimaging. 2012;22:e52–63.
Poretti A, Meoded A, Huisman TA. Neuroimaging of pediatric posterior fossa tumors including review of the literature. J Magn Reson Imaging. 2012;35:32–47.
Reardon W, Donnai D. Dysmorphology demystified. Arch Dis Child Fetal Neonatal Ed. 2007;92:F225–9.
Hennekam RC, Biesecker LG, Allanson JE, et al. Elements of morphology: general terms for congenital anomalies. Am J Med Genet A. 2013;161A:2726–33.
Zafeiriou DI, Batzios SP. Brain and spinal MR imaging findings in mucopolysaccharidoses: a review. AJNR Am J Neuroradiol. 2013;34:5–13.
Alqahtani E, Huisman TA, Boltshauser E, et al. Mucopolysaccharidoses type I and II: new neuroimaging findings in the cerebellum. Eur J Paediatr Neurol. 2014;18:211–7.
Goh RH, Maguire J. Neuroepithelial cyst of the posterior fossa: two case reports with radiologic-pathologic correlation. Can Assoc Radiol J. 1996;47:126–31.
Marsh SE, Grattan-Smith P, Pereira J, Barkovich AJ, Gleeson JG. Neuroepithelial cysts in a patient with Joubert syndrome plus renal cysts. J Child Neurol. 2004;19:227–31.
Poretti A, Huisman TA, Scheer I, Boltshauser E. Joubert syndrome and related disorders: spectrum of neuroimaging findings in 75 patients. AJNR Am J Neuroradiol. 2011;32:1459–63.
Rudnik-Schoneborn S, Barth PG, Zerres K. Pontocerebellar hypoplasia. Am J Med Genet C: Semin Med Genet. 2014;166C:173–83.
Barth PG. Pontocerebellar hypoplasias. An overview of a group of inherited neurodegenerative disorders with fetal onset. Brain Dev. 1993;15:411–22.
Barth PG, Aronica E, de Vries L, et al. Pontocerebellar hypoplasia type 2: a neuropathological update. Acta Neuropathol. 2007;114:373–86.
Namavar Y, Barth PG, Kasher PR, et al. Clinical, neuroradiological and genetic findings in pontocerebellar hypoplasia. Brain. 2011;134:143–56.
Eggens VR, Barth PG, Niermeijer JM, et al. EXOSC3 mutations in pontocerebellar hypoplasia type 1: novel mutations and genotype-phenotype correlations. Orphanet J Rare Dis. 2014;9:23.
Glamuzina E, Brown R, Hogarth K, et al. Further delineation of pontocerebellar hypoplasia type 6 due to mutations in the gene encoding mitochondrial arginyl-tRNA synthetase, RARS2. J Inherit Metab Dis. 2012;35:459–67.
Cassandrini D, Cilio MR, Bianchi M, et al. Pontocerebellar hypoplasia type 6 caused by mutations in RARS2: definition of the clinical spectrum and molecular findings in five patients. J Inherit Metab Dis. 2013;36:43–53.
Kastrissianakis K, Anand G, Quaghebeur G, et al. Subdural effusions and lack of early pontocerebellar hypoplasia in siblings with RARS2 mutations. Arch Dis Child. 2013;98:1004–7.
Hopkins B, Sutton VR, Lewis RA, Van den Veyver I, Clark G. Neuroimaging aspects of Aicardi syndrome. Am J Med Genet A. 2008;146A:2871–8.
Bahi-Buisson N, Poirier K, Boddaert N, et al. GPR56-related bilateral frontoparietal polymicrogyria: further evidence for an overlap with the cobblestone complex. Brain. 2010;133:3194–209.
Barkovich AJ. Current concepts of polymicrogyria. Neuroradiology. 2010;52:479–87.
Quattrocchi CC, Zanni G, Napolitano A, et al. Conventional magnetic resonance imaging and diffusion tensor imaging studies in children with novel GPR56 mutations: further delineation of a cobblestone-like phenotype. Neurogenetics. 2013;14:77–83.
Fujii Y, Ishikawa N, Kobayashi Y, Kobayashi M, Kato M. Compound heterozygosity in GPR56 with bilateral frontoparietal polymicrogyria. Brain Dev. 2013;36:528–31.
Luo R, Yang HM, Jin Z, et al. A novel GPR56 mutation causes bilateral frontoparietal polymicrogyria. Pediatr Neurol. 2011;45:49–53.
Li S, Jin Z, Koirala S, et al. GPR56 regulates pial basement membrane integrity and cortical lamination. J Neurosci. 2008;28:5817–26.
Clement E, Mercuri E, Godfrey C, et al. Brain involvement in muscular dystrophies with defective dystroglycan glycosylation. Ann Neurol. 2008;64:573–82.
Aida N, Yagishita A, Takada K, Katsumata Y. Cerebellar MR in Fukuyama congenital muscular dystrophy: polymicrogyria with cystic lesions. AJNR Am J Neuroradiol. 1994;15:1755–9.
Bonnemann CG, Wang CH, Quijano-Roy S, et al. Diagnostic approach to the congenital muscular dystrophies. Neuromuscul Disord. 2014;24:289–311.
Freeze HH, Chong JX, Bamshad MJ, Ng BG. Solving glycosylation disorders: fundamental approaches reveal complicated pathways. Am J Hum Genet. 2014;94:161–75.
Talim B, Ferreiro A, Cormand B, et al. Merosin-deficient congenital muscular dystrophy with mental retardation and cerebellar cysts unlinked to the LAMA2, FCMD and MEB loci. Neuromuscul Disord. 2000;10:548–52.
Triki C, Louhichi N, Meziou M, et al. Merosin-deficient congenital muscular dystrophy with mental retardation and cerebellar cysts, unlinked to the LAMA2, FCMD, MEB and CMD1B loci, in three Tunisian patients. Neuromuscul Disord. 2003;13:4–12.
Rathod SB, Baheti AD, Dabhade PT, Sankhe SS. Walker-Warburg syndrome: demonstration of cerebellar cysts with CISS sequence. Magn Reson Med Sci. 2012;11:137–40.
Cirak S, Foley AR, Herrmann R, et al. ISPD gene mutations are a common cause of congenital and limb-girdle muscular dystrophies. Brain. 2013;136:269–81.
Hedberg C, Oldfors A, Darin N. B3GALNT2 is a gene associated with congenital muscular dystrophy with brain malformations. Eur J Hum Genet. 2014;22:707–10.
Geis T, Marquard K, Rodl T, et al. Homozygous dystroglycan mutation associated with a novel muscle-eye-brain disease-like phenotype with multicystic leucodystrophy. Neurogenetics. 2013;14:205–13.
Poretti A, Häusler M, Von Moers A, et al. Ataxia, intellectual disability, and ocular apraxia with cerebellar cysts: a new disease? Cerebellum. 2014;13:79–88.
Aldinger KA, Mosca SJ, Tetreault M, et al. Mutations in LAMA1 cause cerebellar dysplasia and cysts with and without retinal dystrophy. Am J Hum Genet. 2014;95:227–34.
Domogatskaya A, Rodin S, Tryggvason K. Functional diversity of laminins. Annu Rev Cell Dev Biol. 2012;28:523–53.
Poretti A, Boltshauser E. Cerebellar dysplasia. In: Boltshauser E, Schmahmann JD, editors. Cerebellar disorders in children. London: MacKeith Press; 2012. p. 172–6.
Doherty D, Chudley AE, Coghlan G, et al. GPSM2 mutations cause the brain malformations and hearing loss in Chudley-McCullough syndrome. Am J Hum Genet. 2012;90:1088–93.
Kau T, Veraguth D, Schiegl H, Scheer I, Boltshauser E. Chudley-McCullough syndrome: case report and review of the neuroimaging spectrum. Neuropediatrics. 2012;43:44–7.
Kivitie-Kallio S, Autti T, Salonen O, Norio R. MRI of the brain in the Cohen syndrome: a relatively large corpus callosum in patients with mental retardation and microcephaly. Neuropediatrics. 1998;29:298–301.
Poretti A, Leventer RJ, Cowan FM, et al. Cerebellar cleft: a form of prenatal cerebellar disruption. Neuropediatrics. 2008;39:106–12.
Poretti A, Huisman TA, Cowan FM, et al. Cerebellar cleft: confirmation of the neuroimaging pattern. Neuropediatrics. 2009;40:228–33.
Poretti A, Prayer D, Boltshauser E. Morphological spectrum of prenatal cerebellar disruptions. Eur J Paediatr Neurol. 2009;13:397–407.
Poretti A, Limperopoulos C, Roulet-Perez E, et al. Outcome of severe unilateral cerebellar hypoplasia. Dev Med Child Neurol. 2010;52:718–24.
Demaerel P, Lagae L, Casaer P, Baert AL. MR of cerebellar cortical dysplasia. AJNR Am J Neuroradiol. 1998;19:984–6.
Demaerel P, Wilms G, Marchal G. Rostral vermian cortical dysplasia: MRI. Neuroradiology. 1999;41:190–4.
Demaerel P. Abnormalities of cerebellar foliation and fissuration: classification, neurogenetics and clinicoradiological correlations. Neuroradiology. 2002;44:639–46.
Livingston JH, Mayer J, Jenkinson E, et al. Leukoencephalopathy with calcifications and cysts: a purely neurological disorder distinct from coats plus. Neuropediatrics. 2014;45:175–82.
Tsutsumi Y, Oka A, Itoh Y, et al. Cerebellar cysts associated with multiple carboxylase deficiency: a case report. Ultrasound Obstet Gynecol. 2010;35:634.
Acknowledgments
We thank Asim F. Choudhri, MD, Department of Radiology, Le Bonheur Children’s Hospital, Memphis, TN, USA, for sharing neuroimaging data of one patient.
Conflict of Interest
All coauthors do not report conflicts of interest.
Funding
This work was not supported by grants.
Author Contribution
EB and AP conceptualized the article, and EB drafted the manuscript. All the coauthors critically revised the manuscript for intellectual content and read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boltshauser, E., Scheer, I., Huisman, T.A.G.M. et al. Cerebellar Cysts in Children: a Pattern Recognition Approach. Cerebellum 14, 308–316 (2015). https://doi.org/10.1007/s12311-014-0633-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-014-0633-9