Abstract
We previously demonstrated that a CD13/CD33 ratio low (< 1) and high (≥ 2) was associated with shorter survival in patients with myelodysplastic syndromes (MDS) treated with azacitidine (AZA). Previous studies also showed the negative impact of TP53 mutations on patient outcomes. The aim of the study is to investigate the relationship between a p53 expression, CD13/CD33 ratio, and the outcomes of MDS patients treated with AZA. The relationship between the p53 expression, CD13/CD33 ratio in blast cells, and outcomes of 121 MDS patients treated with AZA was examined. In patients with CD13/CD33 ratio low and high, there was no significant difference in survival between p53-positive and p53-negative patients. However, in the patients with 1 ≤ CD13/CD33 ratio < 2, p53 positivity correlated with higher serum LDH levels. Poorer risk status according to cytogenetics was more frequently observed in p53-positive patients than in p53-negative patients. The rates of progressive disease and failure after 4 cycles of AZA were higher in p53-positive patients than in p53-negative patients. Univariate and multivariate analyses confirmed that higher serum LDH levels and p53 positivity were independent adverse prognostic factors for prognosis. A Kaplan-Meier analysis revealed the potential of p53 expression as a prognostic factor in patients with 1 ≤ CD13/CD33 ratio < 2 and that it correlated with shorter survival and acute myeloid leukemia (AML) progression. The present study showed that p53 expression is an independent risk factor for shorter overall survival and AML progression in MDS patients with 1 ≤ CD13/CD33 ratio < 2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The hypomethylating agent, azacitidine (AZA), is an effective therapy for low- and high-risk myelodysplastic syndromes (MDS) [1]. MDS are a group of clonal hematological disorders that are characterized by ineffective hematopoiesis, leading to blood cytopenias and a high risk of progression to acute myeloid leukemia (AML) [2]. Approximately 50% of patients respond to AZA, and, thus, prognostic factors for responses and survival need to be clarified in MDS patients treated with AZA. We recently reported that the CD13/CD33 ratio in blast cells from MDS patients treated with AZA was associated with patient outcomes independent of other prognostic factors and the estimated 5-year overall survival (OS) rate was significantly lower in CD13/CD33 low (< 1) or high (≥ 2) than in 1 ≤ CD13/CD33 ratio < 2 (22% vs. 58%, p = 0.015) [3].
A strong relationship has been reported between p53 expression, TP53 mutations, and adverse outcomes in various hematological malignancies including MDS [4,5,6]. TP53 mutations are mainly seen in high-risk MDS with abnormal chromosome 5 or complex karyotype [7, 8]. Previous studies also showed the negative impact of TP53 mutations on patient outcomes and a relationship between TP53 mutations and poor responses to therapies [9,10,11,12]. In this study, we investigated the relationship between p53 expression, CD13/CD33 ratio, and the outcomes of MDS patients treated with AZA.
Patients and methods
Patients
We conducted a retrospective review of data collected from 121 MDS patients treated between January 2007 and January 2019 at the Japanese Red Cross Society Wakayama Medical Center. The present study comprised of patients diagnosed with MDS who received AZA. AZA was intravenously or subcutaneously administered at a dose of 75 mg/m2 on days 1–7 every 28 days. Disease diagnoses were made according to the WHO 2017 classification [13]. Cytogenetic analyses were performed using standard G-banding with trypsin-Giemsa staining. Karyotypes were interpreted using the International System for Cytogenetic Nomenclature criteria [14]. IPSS and IPSS-R were used in risk assessments [15, 16]. From the time of diagnosis of MDS, value for hemoglobin, platelet counts, and serum lactate dehydrogenase (LDH) level was retrospectively evaluated. Responses were evaluated according to the IWG 2006 criteria [17].
Bone marrow samples were obtained from all patients before the beginning of AZA. Sections (thickness of 2 μm) on SuperFrost microscope slides were deparaffinized and pre-treated at 95 °C for 7 min in citrate buffer (pH 6). To quantify and assess the distribution of progenitor cells, samples were stained for CD34 (Cell Marque Rocklin, CA). The DO-7 antibody (Dako Cytomation, Denmark), which labels wild- and mutant-type p53 proteins, was used to detect p53 protein expression. The entire trephine section was assessed for p53 protein nuclear staining in hematopoietic progenitor cells, as previously described [18]. In order to minimize the possibility of false-positive results, p53 protein expression was only considered to be positive when strong nuclear staining (score 3+) was present in at least 5% of hematopoietic cells in the entire bone marrow. To ensure correct staining, a positive control (urothelial carcinoma) was included on each slide.
Three-color flow cytometry was performed to evaluate the phenotypes of blast cells before the beginning of AZA therapy. Mononuclear cells were stained with the following mononuclear antibodies: a fluorescein isothiocyanate (FITC)-conjugated monoclonal antibody, CD3, CD5, CD8, CD15, CD19, CD25, CD34, HLA-DR (Becton Dickinson), phycoerythrin (PE)-conjugated antibodies, CD4, CD11b, CD13, CD14, CD33, CD45 (Becton Dickinson), a peridinin chlorophyll protein (PerCP)-conjugated antibody, CD10, CD117, and glycophorin A (Immunotech). A gate was set for identifying blast cells characterized by intermediate CD45 expression and low side scatter properties. At least 10,000 events were acquired for most samples. The expression of each antigen was considered to be positive when at least 20% of gated cells were fluorescent relative to negative controls. The phenotypes of blast cells were analyzed using a flow cytometer (FACSCalibur; Becton). A ratio of CD13+ cell percentages to CD33+ cell percentages (CD13/CD33 ratio) < 1 (low), 1 ≤ CD13/CD33 ratio < 2, and 2 ≤ CD13/CD33 (high) ratio were noted in 26, 77, and 18 patients, respectively. All patients provided their written informed consent to receive each regimen, and treatment was administered according to the principles of the Declaration of Helsinki. This study was approved by the Japanese Red Cross Society Wakayama Medical Center ethics committee.
Statistical analysis
Fisher’s exact test and the Mann-Whitney U test were used to assess the significance of differences. Overall survival (OS) was calculated as the time from the date of diagnosis to death from any cause and AML progression was calculated as the time from the date of diagnosis to leukemic transformation. OS and AML progressions were assessed using the Kaplan-Meier method and log-rank test. Factors affecting OS and AML progression were analyzed using univariate and multivariate Cox’s proportional hazard regression models. A p value less than 0.05 was considered to be significant. Statistical analyses were performed with the SPSS 11.5 system.
Results
The present study included 74 males (62%) and 47 females (38%) with a median age of 69 years (range 20–87 years). The median follow-up of the entire population was 39 months (range 4–138 months). One hundred fourteen patients (95%) received no prior therapy; three (2%) received lenalidomide before AZA, 2 (1%) vitaminic support, and 2 (2%) erythroid-stimulating agents. According to the WHO classification, 12 patients (10%) were diagnosed with MDS-SLD or MDS-RS, 10 (7%) with MDS-MLD, 46 (40%) with MDS-EB-1, 50 (41%) with MDS-EB-2, and 3 (2%) with MDS with isolated del (5q). According to IPSS-R, 14 patients (12%) were stratified as very low or low, 37 (31%) as intermediate, 45 (37%) as high, and 25 (20%) as very high risk. Cytogenetic aberrations were stratified according to the IPSS-R risk score, and 2 patients (2%) were diagnosed as very good, 49 (40%) as good, 19 (16%) as intermediate, 13 (11%) as poor, and 38 (31%) as very poor risk. According to the IWG criteria applied after the fourth cycle, 16% of patients achieved a complete response (CR), 36% partial response (PR), and 17% stable disease (SD). The median number of cycles of AZA was 9.6 (range 4–60) with a median time on treatment of 26 months (range 4–86).
In patients with CD13/CD33 low or high, twenty-five patients were positive for p53 expression, while 19 were negative (Table 1). p53 positivity correlated with higher serum LDH levels. However, no significant differences were observed in age, sex, the WHO classification, IPSS-R, risk status according to cytogenetics, response after 4 cycles of AZA, and the median number of cycles of AZA between the 2 groups. There was no significant difference in OS between p53-positive and p53-negative patients with CD13/CD33 low or high.
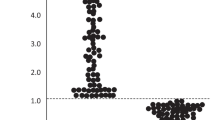
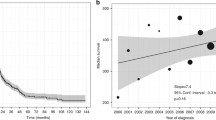
In patients with 1 ≤ CD13/CD33 ratio < 2, twenty-nine patients were positive for p53 expression, while 48 were negative (Table 2). No significant differences were observed in age, sex, hemoglobin, platelet counts, the WHO classification, and IPSS-R between the 2 groups. However, p53 positivity correlated with higher serum LDH levels. Poorer risk status according to cytogenetics was more frequently observed in p53-positive patients than in p53-negative patients. The median number of cycles of AZA was lower in p53-positive patients than in p53-negative patients. The rates of PD and failure after 4 cycles of AZA were higher in p53-positive patients than in p53-negative patients. The estimated 5-year OS rate was significantly lower in p53-positive patients than in p53-negative patients (32.4% vs. 69%, p = 0.038) (Fig. 1a). The 5-year rate to AML progression was significantly higher in p53-positive patients than in p53-negative patients (31% vs. 16%, p = 0.047) (Fig. 1b). A number of prognostic indicators for OS and AML progression were significant in univariate and multivariate analyses (Table 3). Univariate and multivariate analyses confirmed that higher serum LDH levels, poor/very poor IPSS-R cytogenetic risk groups, poor responses after 4 cycles of AZA, and p53 positivity were independent adverse prognostic factors for OS. Univariate analyses confirmed that higher serum LDH levels, poor/very poor IPSS-R cytogenetic risk groups, a poor response (PD and failure) after 4 cycles of AZA, and p53 positivity were independent adverse prognostic factors for AML progression. The multivariate analysis showed that higher serum LDH levels and p53 positivity were independent adverse prognostic factors for AML progression.
Discussion
The present study demonstrated the relationship between p53 expression and the outcomes of MDS patients treated with AZA. We previously demonstrated that a CD13/CD33 ratio low or high was associated with shorter survival in our MDS patients treated with AZA. Although there was no significant difference in survival between p53 positive and p53 negative in patients with CD13/CD33 ratio low or high, p53 positivity was correlated with shorter OS and higher AML progression in the patients with 1 ≤ CD13/CD33 ratio < 2.
Somatic gene mutations affecting patient outcomes, such as TP53, EZH2, ETV6, RUNX1, and ASXL1, have recently been identified in MDS [19,20,21]. Mutations in p53 proteins generally result in the loss of their normal functions and may also lead to the gain of another function. Previous studies demonstrated the negative impact of TP53 mutations on patient outcomes and found a relationship between TP53 mutations and poor therapy responses [9, 19, 22, 23]; however, it currently remains unclear whether p53 expression also influences responses to AZA. Muller-Thomas et al. showed that p53 expression did not have a negative impact on treatment responses in patients with higher-risk MDS and secondary AML treated with AZA [24], and the present study showed p53 expression was also not associated with treatment response in patients with CD13/CD33 low and high. On the other hand, p53 expression in the patients with 1 ≤ CD13/CD33 ratio < 2 was correlated with shorter OS and higher AML progression, and higher LDH level and poorer cytogenetic abnormalities were associated with p53 expression in these patients.
Previous studies identified an increased LDH level as a poor prognostic predictor in MDS and AML [25, 26]. Park et al. reported that an increased LDH level had a negative effect on the OS of MDS patients [26]. Other reports described the pretreatment risk group and initial LDH levels were confirmed as important prognostic factors to predict the outcomes for patients with AZA [27]. Although it is unknown the association of LDH level and p53 expression, higher LDH level was associated with p53 expression and poor prognosis in our study.
Recurrent cytogenetic abnormalities are powerful predictors of the outcomes of patients with MDS and are included in several prognostic scoring systems used in clinical practice [28]. MDS with a complex karyotype may carry a wide range of chromosomal abnormalities and somatic mutations. IPSS-R assigns a substantial risk to 10% of MDS patients with a complex karyotype, defined as three or more somatic chromosomal abnormalities in a single clone. IPSS-R considers patients with three or more abnormalities to have a poor or very poor cytogenetic risk. As defined by IPSS-R, the presence of complex karyotypes excludes MDS patients from having lower-risk MDS [16, 29]. Among MDS with complex karyotypes, the presence of TP53 mutations has been correlated with poor outcomes [30]. As shown in Table 2, poor and very poor IPSS-R cytogenetic risks were associated with p53 expression. The present study demonstrated that an increase in p53-positive cells may predict disease progression and cytogenetic evolution.
In conclusion, the present study showed that p53 expression is an independent risk factor for shorter OS and AML progression in MDS patients with 1 ≤ CD13/CD33 ratio < 2. The prognosis of patients with 1 ≤ CD13/CD33 ratio < 2 was better than that of CD13/CD33 ratio low and high; however, there are some cases that progress to AML. Although a response to AZA or achievement of a CR did delay leukemic evolution, it did not prevent progression to AML. Our study showed p53 positivity in MDS patients with 1 ≤ CD13/CD33 ratio < 2 was associated with AML progression. Thus more intensive therapy, including allogenic transplantation or early combination approaches, may improve outcomes for those patients. Further studies are warranted to clarify the roles of these markers in the pathogenesis of MDS treated with AZA.
References
Greenberg PL, Young NS, Gattermann N (2002) Myelodysplastic syndromes. Hematol Am Soc Hematol Educ Program 2002:136–161
Tefferi A, Vardiman JW (2009) Myelodysplastic syndromes. N Engl J Med 361:1872–1885
Oka S, Ono K, Nohgawa M (2020) Clinical effects of the CD13/CD33 ratio on the prognosis of myelodysplastic syndrome treated with azacitidine. Leuk Lymphoma 61:1250–1253
Schlette EJ, Admirand J, Wierda W et al (2009) p53 expression by immunohistochemistry is an important determinant of survival in patients with chronic lymphocytic leukemia receiving frontline chemo-immunotherapy. Leuk Lymphoma 50:1597–1605
Nakano Y, Naoe T, Kiyoi H, Kitamura K, Minami S, Miyawaki S, Asou N, Kuriyama K, Kusumoto S, Shimazaki C, Akiyama H, Saito K, Nishimura M, Motoji T, Shinagawa K, Saito H, Ohno R (2000) Prognostic value of p53 gene mutations and the product expression in de novo acute myeloid leukemia. Eur J Haematol 65:23–31
Kikukawa M, Aoki N, Sakamoto Y, Mori M (1999) Study of p53 in elderly patients with myelodysplastic syndromes by immunohistochemistry and DNA analysis. Am J Pathol 155:717–721
Kita-Sasai Y, Horiike S, Misawa S, Kaneko H, Kobayashi M, Nakao M, Nakagawa H, Fujii H, Taniwaki M (2001) International prognostic scoring system and TP53 mutations are independent prognostic indicators for patients with myelodysplastic syndrome. Br J Haematol 115:309–312
Kulasekararaj AG, Smith AE, Mian SA, Mohamedali AM, Krishnamurthy P, Lea NC, Gäken J, Pennaneach C, Ireland R, Czepulkowski B, Pomplun S, Marsh JC, Mufti GJ (2013) TP53 mutations in myelodysplastic syndrome are strongly correlated with aberrations of chromosome 5, and correlate with adverse prognosis. Br J Haematol 160:660–672
Kaneko H, Misawa S, Horiike S, Nakai H, Kashima K (1995) TP53 mutations emerge at early phase of myelodysplastic syndrome and are associated with complex chromosomal abnormalities. Blood. 85:2189–2193
Padua RA, Guinn BA, Al-Sabah AI et al (1998) RAS, FMS and p53 mutations and poor clinical outcome in myelodysplasias: a 10-year follow-up. Leukemia. 12:887–892
Horiike S, Kita-Sasai Y, Nakao M, Taniwaki M (2003) Configuration of the TP53 gene as an independent prognostic parameter of myelodysplastic syndrome. Leuk Lymphoma 44:915–922
Nishiwaki S, Ito M, Watari R et al (2016) A new prognostic index to make short-term prognoses in MDS patients treated with azacitidine: a combination of p53 expression and cytogenetics. Leuk Res 41:21–26
Swerdlow SH, Campo E, Harris NL et al (2017) WHO classification of tumours of haematopoietic and lymphoid tissues, 4th edn. IARC Press, Lyon
Shaffer LG, McGowan-Jordan J, Schnid M (2013). ISCN: an international system for human cytogenetic nomencaltue. S Karger:Basel, Switzerland, 2013
Greenberg P, Cox C, LeBeau MM et al (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 89:2079–2088
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F, Bennett JM, Bowen D, Fenaux P, Dreyfus F, Kantarjian H, Kuendgen A, Levis A, Malcovati L, Cazzola M, Cermak J, Fonatsch C, le Beau MM, Slovak ML, Krieger O, Luebbert M, Maciejewski J, Magalhaes SMM, Miyazaki Y, Pfeilstöcker M, Sekeres M, Sperr WR, Stauder R, Tauro S, Valent P, Vallespi T, van de Loosdrecht AA, Germing U, Haase D (2012) Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 120:2454–2465
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 127:2391–2405
Iwasaki T, Murakami M, Sugisaki C, Sobue S, Ohashi H, Asano H, Suzuki M, Nakamura S, Ito M, Murate T (2008) Characterization of myelodysplastic syndrome and aplastic anemia by immunostaining of p53 and hemoglobin F and karyotype analysis: differential diagnosis between refractory anemia and aplastic anemia. Pathol Int 58:353–360
Bejar R, Stevenson K, Abdel-Wahab O, Galili N, Nilsson B, Garcia-Manero G, Kantarjian H, Raza A, Levine RL, Neuberg D, Ebert BL (2011) Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med 364:2496–2506
Haferlach T, Nagata Y, Grossmann V, Okuno Y, Bacher U, Nagae G, Schnittger S, Sanada M, Kon A, Alpermann T, Yoshida K, Roller A, Nadarajah N, Shiraishi Y, Shiozawa Y, Chiba K, Tanaka H, Koeffler HP, Klein HU, Dugas M, Aburatani H, Kohlmann A, Miyano S, Haferlach C, Kern W, Ogawa S (2014) Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia. 28:241–247
Papaemmanuil E, Gerstung M, Malcovati L, Tauro S, Gundem G, van Loo P, Yoon CJ, Ellis P, Wedge DC, Pellagatti A, Shlien A, Groves MJ, Forbes SA, Raine K, Hinton J, Mudie LJ, McLaren S, Hardy C, Latimer C, Della Porta MG, O’Meara S, Ambaglio I, Galli A, Butler AP, Walldin G, Teague JW, Quek L, Sternberg A, Gambacorti-Passerini C, Cross NC, Green AR, Boultwood J, Vyas P, Hellstrom-Lindberg E, Bowen D, Cazzola M, Stratton MR, Campbell PJ, Chronic Myeloid Disorders Working Group of the International Cancer Genome Consortium (2013) Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood. 122:3616–3627
Christiansen DH, Andersen MK, Pedersen-Bjergaard J (2001) Mutations with loss of heterozygosity of p53 are common in therapy-related myelodysplasia and acute myeloid leukemia after exposure to alkylating agents and significantly associated with deletion or loss of 5q, a complex karyotype, and a poor prognosis. J Clin Oncol 19:1405–1413
Sugimoto K, Hirano N, Toyoshima H, Chiba S, Mano H, Takaku F, Yazaki Y, Hirai H (1993) Mutations of the p53 gene in myelodysplastic syndrome (MDS) and MDS-derived leukemia. Blood. 81:3022–3026
Müller-Thomas C, Rudelius M, Rondak IC et al (2014) Response to azacitidine is independent of p53 expression in higher-risk myelodysplastic syndromes and secondary acute myeloid leukemia. Haematologica. 99:e179–e181
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, Schoch R, Gattermann N, Sanz G, List A, Gore SD, Seymour JF, Bennett JM, Byrd J, Backstrom J, Zimmerman L, McKenzie D, Beach C, Silverman LR, International Vidaza High-Risk MDS Survival Study Group (2009) Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol 10:223–232
Park MJ, Kim HJ, Kim SH et al (2008) Is International Prognostic Scoring System (IPSS) still standard in predicting prognosis in patients with myelodysplastic syndrome? External validation of the WHO Classification-Based Prognostic Scoring System (WPSS) and comparison with IPSS. Eur J Haematol 81:364–367
Moon JH, Kim SN, Kang BW, Chae YS, Kim JG, Baek JH, Park JH, Song MK, Chung JS, Won JH, Lee SM, Joo YD, Kim YK, Kim HJ, Jo DY, Sohn SK (2010) Predictive value of pretreatment risk group and baseline LDH levels in MDS patients receiving azacitidine treatment. Ann Hematol 89:681–689
Bejar R (2014) Clinical and genetic predictors of prognosis in myelodysplastic syndromes. Haematologica. 99:956–964
Schanz J, Tüchler H, Solé F, Mallo M, Luño E, Cervera J, Granada I, Hildebrandt B, Slovak ML, Ohyashiki K, Steidl C, Fonatsch C, Pfeilstöcker M, Nösslinger T, Valent P, Giagounidis A, Aul C, Lübbert M, Stauder R, Krieger O, Garcia-Manero G, Faderl S, Pierce S, le Beau MM, Bennett JM, Greenberg P, Germing U, Haase D (2012) New comprehensive cytogenetic scoring system for primary myelodysplastic syndromes (MDS) and oligoblastic acute myeloid leukemia after MDS derived from an international database merge. J Clin Oncol 30:820–829
Haase D, Stevenson KE, Neuberg D et al (2019) TP53 mutation status divides myelodysplastic syndromes with complex karyotypes into distinct prognostic subgroups. Leukemia. 33:1747–1758
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Statement of ethics
All patients provided their written informed consent to receive each regimen, and treatment was administered according to the principles of the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Oka, S., Ono, K. & Nohgawa, M. Relationship between p53 expression and prognosis of myelodysplastic syndrome treated with azacitidine. J Hematopathol 13, 213–219 (2020). https://doi.org/10.1007/s12308-020-00412-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12308-020-00412-w