Abstract
Background
Invasive lobular carcinoma (ILC) is known to be the second most common histological type following invasive ductal carcinoma (IDC). Definitive clinical features of ILC are controversial.
Methods
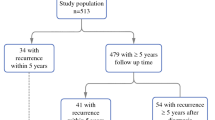
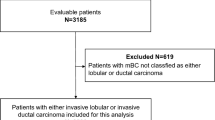
We retrospectively analyzed a cohort of 330 patients with metastatic breast cancer, 303 of IDC, 19 of ILC, and 8 of others. We compared the patient age and tumor–node–metastasis factors, disease-free survival (DFS), estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor 2 (HER2) expression at the primary site between ILC and IDC. We then selected the patients in the ER+ or PR+/HER2− subtype specifically and compared sites of recurrence, and the survival curve starting from the point of development of metastatic disease.
Results
The clinical stage was significantly higher in the ILC patients than in the IDC (p = 0.001). The mean (±SD) of DFS for the ILC and IDC patients was 2.6 ± 0.6 and 2.4 ± 0.3 years, respectively, with no significant difference (p = 0.18). However, the hormone receptor status was same between both groups; the rate of HER2 positivity was significantly lower in the ILC group (0%) than in the IDC group (16.2%) (p = 0.05). In ER+ or PR+/HER2− subtype, the mean DFS for the ILC and IDC was 2.9 ± 0.6 and 3.1 ± 0.3 years, and the median survival time after the recurrence for ILC and IDC patients was 4.2 ± 0.7 and 5.6 ± 0.7 years, respectively, with no significant difference (p = 0.77). The frequency of lung metastases was significantly lower in the ILC group (6.3%) than in the IDC group (53.7%) (p < 0.01), while the frequency of peritoneal metastases was significantly higher in the ILC group (68.8%) than in the IDC group (1%) (p = 0.00). Of note, the prognosis after the diagnosis of peritoneal metastases was poor, with a median survival time of 19 ± 9 months and resistance to hormone therapy.
Conclusions
The extremely high rate (68.8%) of peritoneal metastases was observed in long-term follow-up for the metastatic breast cancer patients with ILC. We need to reveal the definitive feature of ILC and develop new therapeutic strategies to prevent the dissemination of ILCs.

Similar content being viewed by others
References
Ashikari R, Huvos AG, Urban JA, Robbins GF. Infiltrating lobular carcinoma of the breast. Cancer. 1973;31:110–6.
Sastre-Garau X, Jouve M, Asselain B, Vincent-Salomon A, Beuzeboc P, Dorval T, et al. Infiltrating lobular carcinoma of the breast. Clinicopathologic analysis of 975 cases with reference to data on conservative therapy and metastatic patterns. Cancer. 1996;77:113–20.
Martinez V, Azzopardi JG. Invasive lobular carcinoma of the breast: incidence and variants. Histopathology. 1979;3:467–88.
Fu L, Tsuchiya S, Matsuyama I, Ishii K. Clinicopathologic features and incidence of invasive lobular carcinoma in Japanese women. Pathol Int. 1998;48:348–54.
Jung SY, Jeong J, Shin SH, Kwon Y, Kim EA, Ko KL, et al. The invasive lobular carcinoma as a prototype luminal A breast cancer: a retrospective cohort study. BMC Cancer. 2010;10:664.
Li CI, Anderson BO, Porter P, Holt SK, Daling JR, Moe RE. Changing incidence rate of invasive lobular breast carcinoma among older women. Cancer. 2000;88:2561–9.
Chen CL, Weiss NS, Newcomb P, Barlow W, White E. Hormone replacement therapy in relation to breast cancer. JAMA. 2002;287:734–41.
Arpino G, Bardou VJ, Clark GM, Elledge RM. Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res. 2004;6:R149–56.
Horsfall DJ, Tilley WD, Orell SR, Marshall VR, Cant EL. Relationship between ploidy and steroid hormone receptors in primary invasive breast cancer. Br J Cancer. 1986;53:23–8.
Garcia-Fernandez A, Lain JM, Chabrera C, Garcia Font M, Fraile M, Barco I, et al. Comparative long-term study of a large series of patients with invasive ductal carcinoma and invasive lobular carcinoma. Loco-regional recurrence, metastasis, and survival. Breast J. 2015;21:533–7.
Pestalozzi BC, Zahrieh D, Mallon E, Gusterson BA, Price KN, Gelber RD, et al. Distinct clinical and prognostic features of infiltrating lobular carcinoma of the breast: combined results of 15 International Breast Cancer Study Group clinical trials. J Clin Oncol. 2008;26:3006–14.
Mersin H, Yildirim E, Gulben K, Berberoglu U. Is invasive lobular carcinoma different from invasive ductal carcinoma? Eur J Surg Oncol. 2003;29:390–5.
Yagi Y, Sasaki S, Yoshikawa A, Tsukioka Y, Fukushima W, Fujimura T, et al. Metastatic gastric carcinoma from breast cancer mimicking primary linitis plastica: a case report. Oncol Lett. 2015;10:3483–7.
Jones GE, Strauss DC, Forshaw MJ, Deere H, Mahedeva U, Mason RC. Breast cancer metastasis to the stomach may mimic primary gastric cancer: report of two cases and review of literature. World J Surg Oncol. 2007;5:75.
Harris M, Howell A, Chrissohou M, Swindell RI, Hudson M, Sellwood RA. A comparison of the metastatic pattern of infiltrating lobular carcinoma and infiltrating duct carcinoma of the breast. Br J Cancer. 1984;50:23–30.
Lamovec J, Bracko M. Metastatic pattern of infiltrating lobular carcinoma of the breast: an autopsy study. J Surg Oncol. 1991;48:28–33.
Veronesi U, Viale G, Rotmensz N, Goldhirsch A. Rethinking TNM: breast cancer TNM classification for treatment decision-making and research. Breast. 2006;15:3–8.
Harvey JM, Clark GM, Osborne CK, Allred DC. Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol. 1999;17:1474–81.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31:3997–4013.
Fisher ER, Gregorio RM, Fisher B, Redmond C, Vellios F, Sommers SC. The pathology of invasive breast cancer. A syllabus derived from findings of the National Surgical Adjuvant Breast Project (protocol no. 4). Cancer. 1975;36:1–85.
Krecke KN, Gisvold JJ. Invasive lobular carcinoma of the breast: mammographic findings and extent of disease at diagnosis in 184 patients. AJR Am J Roentgenol. 1993;161:957–60.
Molland JG, Donnellan M, Janu NC, Carmalt HL, Kennedy CW, Gillett DJ. Infiltrating lobular carcinoma—a comparison of diagnosis, management and outcome with infiltrating duct carcinoma. Breast. 2004;13:389–96.
Berx G, Cleton-Jansen AM, Strumane K, de Leeuw WJ, Nollet F, van Roy F, et al. E-cadherin is inactivated in a majority of invasive human lobular breast cancers by truncation mutations throughout its extracellular domain. Oncogene. 1996;13:1919–25.
De Leeuw WJ, Berx G, Vos CB, Peterse JL, Van de Vijver MJ, Litvinov S, et al. Simultaneous loss of E-cadherin and catenins in invasive lobular breast cancer and lobular carcinoma in situ. J Pathol. 1997;183:404–11.
Gruel N, Lucchesi C, Raynal V, Rodrigues MJ, Pierron G, Goudefroye R, et al. Lobular invasive carcinoma of the breast is a molecular entity distinct from luminal invasive ductal carcinoma. Eur J Cancer. 2010;46:2399–407.
Keller G, Vogelsang H, Becker I, Hutter J, Ott K, Candidus S, et al. Diffuse type gastric and lobular breast carcinoma in a familial gastric cancer patient with an E-cadherin germline mutation. Am J Pathol. 1999;155:337–42.
Pharoah PD, Guilford P, Caldas C, International Gastric Cancer Linkage Consortium. Incidence of gastric cancer and breast cancer in CDH1 (E-cadherin) mutation carriers from hereditary diffuse gastric cancer families. Gastroenterology. 2001;121:1348–53.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
About this article
Cite this article
Inoue, M., Nakagomi, H., Nakada, H. et al. Specific sites of metastases in invasive lobular carcinoma: a retrospective cohort study of metastatic breast cancer. Breast Cancer 24, 667–672 (2017). https://doi.org/10.1007/s12282-017-0753-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-017-0753-4