Abstract
Background
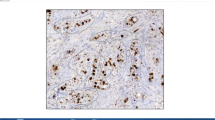
In recent papers, Ki67 labeling index (LI) has been used to classify breast cancer patients into the low and high Ki67LI groups for comparison studies, which showed significant differences in many prognostic factors. It has not been clarified whether image analysis software can be used for calculating LI in breast cancer. In our study, we examined whether Ki67LI in breast cancer calculated using image analysis software correlates with that measured on the basis of visual.
Methods
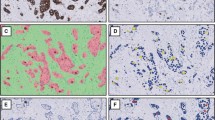
Fifty patients were randomly selected among breast cancer patients who underwent surgical operation from March, 2010 to May, 2010 in our hospital without preoperative chemotherapy. In this study, for the virtual slide system (VSS: VS120-L100, Olympus, Tokyo, Japan), the high-resolution VSs of all the 50 patients were prepared as samples. The image analysis software use for calculating LI was Tissuemorph Digital Pathology (Tissuemorph DP: Visiopharm, Hoersholm, Denmark). The calculated LI was extracted from 3 to 5 views containing hot spots. The LI calculated using Tissuemorph DP was designed as LI/image/T. The digital image of 3 to 5 LI/image/T views was printed out, and on the digital photograph, we counted visually the number of Ki67-immunopositive cells in exactly the same area, and the percentage of Ki67-immunopositive cells was designed as LI/direct. Moreover, a pathologist’s assistant (PA) determined the tumor area in the same specimen using VSS and calculated LI using Tissuemorph DP, which was designed as LI/image/PA. The chief pathologist (CP) similarly calculated LI which was designed as LI/image/CP. We evaluated the degree of agreement between different data sets “LI/image/T and LI/direct” and “LI/image/T, LI/image/CP, and LI/image/PA” by using interclass correlation coefficient (ICC).
Results
The average counts of cells were as follows: LI/direct, 3209.7 ± 1970.4 (SD); LI/image/T, 2601.6 ± 1697.1; LI/image/PA, 2886.5 ± 2027.5; LI/image/CP, 18805.5 ± 22293.4. The values of LI/direct and LI/image/T showed almost perfect agreement as showed by an ICC of 0.885 (95 % CI, 0.806–0.933; p < 0.001). The agreement among three investigators was almost perfect. The obtained ICC was 0.825 (95 % CI, 0.739–0.890; p < 0.001) among the data of LI/image/T, LI/image/CP and LI/image/PA. There were five cases that immunopositivity for Ki67 showed a more than 10 % disagreement between LI/direct and LI/image/T.
Conclusion
The merits of calculating Ki67 LI using Tissuemorph DP are as follows. First, the staining intensity of the cells to be counted can be adjusted. Second, the portion of a tumor including “hot spots” for counting can be chosen. Third, many cancer cells can be counted more rapidly using Tissuemorph DP than by visual observation. However, it is important that pathologist should check and carry out the final decision of the data, when Ki67 LI using Tissuemorph DP is calculated.






Similar content being viewed by others
References
Bago-Horvath Z, Rudas M, Dubsky P, Jakesz R, Singer CF, Kemmerling R, Greil R, Jelen A, Bohm G, Jasarevic Z, et al. Adjuvant sequencing of tamoxifen and anastrozole is superior to tamoxifen alone in postmenopausal women with low proliferating breast cancer. Clin Cancer Res. 2011;17(24):7828–34.
Millar EK, Graham PH, McNeil CM, Browne L, O’Toole SA, Boulghourjian A, Kearsley JH, Papadatos G, Delaney G, Fox C, et al. Prediction of outcome of early ER+ breast cancer is improved using a biomarker panel, which includes Ki-67 and p53. Br J Cancer. 2011;105(2):272–80.
Viale G, Giobbie-Hurder A, Regan MM, Coates AS, Mastropasqua MG, Dell’Orto P, Maiorano E, MacGrogan G, Braye SG, Ohlschlegel C, et al. Prognostic and predictive value of centrally reviewed Ki-67 labeling index in postmenopausal women with endocrine-responsive breast cancer: results from Breast International Group Trial 1-98 comparing adjuvant tamoxifen with letrozole. J Clin Oncol. 2008;26(34):5569–75.
Reyal F, Hajage D, Savignoni A, Feron JG, Bollet MA, Kirova Y, Fourquet A, Pierga JY, Cottu P, Dieras V, et al. Long-term prognostic performance of Ki67 rate in early stage, pT1-pT2, pN0, invasive breast carcinoma. PLoS ONE. 2013;8(3):e55901.
Cheang MC, Chia SK, Voduc D, Gao D, Leung S, Snider J, Watson M, Davies S, Bernard PS, Parker JS, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101(10):736–50.
Kobayashi T, Iwaya K, Moriya T, Yamasaki T, Tsuda H, Yamamoto J, Matsubara O. A simple immunohistochemical panel comprising 2 conventional markers, Ki67 and p53, is a powerful tool for predicting patient outcome in luminal-type breast cancer. BMC Clin Pathol. 2013;13:5.
Gudlaugsson E, Skaland I, Janssen EA, Smaaland R, Shao Z, Malpica A, Voorhorst F, Baak JP. Comparison of the effect of different techniques for measurement of Ki67 proliferation on reproducibility and prognosis prediction accuracy in breast cancer. Histopathology. 2012;61(6):1134–44.
Haglund F, Ma R, Huss M, Sulaiman L, Lu M, Nilsson IL, Hoog A, Juhlin CC, Hartman J, Larsson C. Evidence of a functional estrogen receptor in parathyroid adenomas. J Clin Endocrinol Metab. 2012;97(12):4631–9.
Skaland I, Janssen EA, Gudlaugsson E, Klos J, Kjellevold KH, Soiland H, Baak JP. Phosphohistone H3 expression has much stronger prognostic value than classical prognosticators in invasive lymph node-negative breast cancer patients less than 55 years of age. Mod Pathol. 2007;20(12):1307–15.
Janssen EA, Slewa A, Gudlaugsson E, Jonsdottir K, Skaland I, Soiland H, Baak JP. Biologic profiling of lymph node negative breast cancers by means of microRNA expression. Mod Pathol. 2010;23(12):1567–76.
Mikami Y, Ueno T, Yoshimura K, Tsuda H, Kurosumi M, Masuda S, Horii R, Toi M, Sasano H. Interobserver concordance of Ki67 labeling index in breast cancer: Japan Breast Cancer Research Group Ki67 Ring Study. Cancer Sci. 2013;104:1539–43.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Niikura N, Sakatani T, Arima N, Ohi Y, Honma N, Kanomata N, Yoshida K, Kadoya T, Tamaki K, Kumaki N et al. Assessment of the Ki67 labeling index: a Japanese validation ring study. Breast Cancer (Tokyo, Japan) 2014.
Knutsvik G, Stefansson IM, Aziz S, Arnes J, Eide J, Collett K, Akslen LA. Evaluation of Ki67 expression across distinct categories of breast cancer specimens: a population-based study of matched surgical specimens, core needle biopsies and tissue microarrays. PLoS ONE. 2014;9(11):e112121.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Maeda, I., Abe, K., Koizumi, H. et al. Comparison between Ki67 labeling index determined using image analysis software with virtual slide system and that determined visually in breast cancer. Breast Cancer 23, 745–751 (2016). https://doi.org/10.1007/s12282-015-0634-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-015-0634-7