Abstract
Background
The criteria for classifying hormone receptor (HR)-positive/HER2-negative breast cancers into low-risk and high-risk subgroups remain undetermined. Supportive data for optimal criteria to identify tumors in the high-risk subgroup are necessary for Japanese patients with HR-positive/HER2-negative breast cancers.
Methods
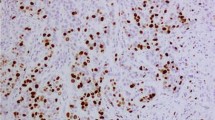
Using immunohistochemistry and fluorescence in situ hybridization, we identified 369 consecutive patients with HR-positive/HER2-negative, node-negative invasive breast cancers. We examined the prognostic impact of the Ki-67 labeling index (LI) based on 3 cutoff values, 10, 14, and 20 %, along with that of histological grade (HG) and nuclear grade (NG) by Cox’s univariate and multivariate analyses.
Results
The univariate analyses clearly showed that Ki-67 LI with any cutoff value divided the patients into distinct high-risk and low-risk groups, and that HG and NG were also powerful prognostic indicators. High Ki-67 LI with any cutoff value was strongly correlated with HG and NG, and when these parameters were included in the multivariate analyses, the impact of HG/NG was stronger than Ki-67 LIs. When the 10 % cutoff value was adopted, discordance between Ki-67 LI and grades was frequent in papillotubular-type invasive ductal carcinoma, predominantly intraductal carcinoma, and mucinous carcinoma.
Conclusions
Any of the Ki-67 LI values, regardless of cutoff value, could be applicable for the classification of high-risk and low-risk HR-positive/HER2-negative, node-negative invasive breast cancers. Luminal A/B subtyping according to Ki-67 LI, or HG/NG, in combination with histological type, appeared to be able to create an optimum risk estimation system for patients with HR-positive/HER2-negative, node-negative invasive breast cancers in Japan.




Similar content being viewed by others
References
Center for Cancer Control and Information Services, National Cancer Center J. Vital Statistics Japan (Ministry of Health, Labour and Welfare). 2009.
Kurebayashi J, Kanomata N, Shimo T, et al. Marked lymphovascular invasion, progesterone receptor negativity, and high Ki67 labeling index predict poor outcome in breast cancer patients treated with endocrine therapy alone. Breast Cancer. (in press).
Watanabe T, Sano M, Takashima S, et al. Oral uracil and tegafur compared with classic cyclophosphamide, methotrexate, fluorouracil as postoperative chemotherapy in patients with node-negative, high-risk breast cancer: National Surgical Adjuvant Study for Breast Cancer 01 Trial. J Clin Oncol. 2009;27:1368–74.
Tsuda H, Akiyama F, Kurosumi M, et al. Establishment of histological criteria for high-risk node-negative breast carcinoma for a multi-institutional randomized clinical trial of adjuvant therapy. Japan National Surgical Adjuvant Study of Breast Cancer (NSAS-BC) Pathology Section. Jpn J Clin Oncol. 1998;28:486–91.
Carey LA, Perou CM, Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295:2492–502.
Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature. 2000;406:747–52.
Sorlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A. 2001;98:10869–74.
Desmedt C, Haibe-Kains B, Wirapati P, et al. Biological processes associated with breast cancer clinical outcome depend on the molecular subtypes. Clin Cancer Res. 2008;14:5158–65.
Rouzier R, Perou CM, Symmans WF, et al. Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res. 2005;11:5678–85.
Goldhirsch A, Wood WC, Coates AS, et al. Strategies for subtypes-dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–47.
Cheang MC, Chia SK, Voduc D, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101:736–50.
de Azambuja E, Cardoso F, de Castro G Jr, et al. Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12,155 patients. Br J Cancer 2007;96:1504–13.
Dowsett M, Nielsen TO, A’Hern R, et al. Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer working group. J Natl Cancer Inst. 2011;103:1656–64.
Viale G, Giobbie-Hurder A, Regan MM, et al. Prognostic and predictive value of centrally reviewed Ki-67 labeling index in postmenopausal women with endocrine-responsive breast cancer: results from Breast International Group Trial 1–98 comparing adjuvant tamoxifen with letrozole. J Clin Oncol. 2008;26:5569–75.
Viale G, Regan MM, Mastropasqua MG, et al. Predictive value of tumor Ki-67 expression in two randomized trials of adjuvant chemoendocrine therapy for node-negative breast cancer. J Natl Cancer Inst. 2008;100:207–12.
Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology. 1991;19:403–10.
Japanese Breast Cancer Society. General rules for clinical and pathological recording of breast cancer. 16th ed. Tokyo: Kanehara Shuppan; 2008. p. 18–28 (in Japanese).
Harvey JM, Clark GM, Osborne CK, Allred DC. Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol. 1999;17:1474–81.
Wolff AC, Hammond ME, Schwartz JN, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–45.
Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351:2817–26.
Toi M, Iwata H, Yamanaka T, et al. Clinical significance of the 21-gene signature (Oncotype DX) in hormone receptor-positive early stage primary breast cancer in the Japanese population. Cancer. 2010;116:3112–8.
Longacre TA, Ennis M, Quenneville LA, et al. Interobserver agreement and reproducibility in classification of invasive breast carcinoma: an NCI breast cancer family registry study. Mod Pathol. 2006;19:195–207.
Tsuda H, Akiyama F, Kurosumi M, et al. The efficacy and limitations of repeated slide conferences for improving interobserver agreement when judging nuclear atypia of breast cancer. The Japan National Surgical Adjuvant Study of Breast Cancer (NSAS-BC) Pathology Section. Jpn J Clin Oncol. 1999;29:68–73.
Tsuda H, Akiyama F, Kurosumi M, et al. Evaluation of the interobserver agreement in the number of mitotic figures of breast carcinoma as simulation of quality monitoring in the Japan National Surgical Adjuvant Study of Breast Cancer (NSAS-BC) protocol. Jpn J Cancer Res. 2000;91:451–7.
Rakha E, Pinder S, Shin D, Tsuda H. Tubular carcinoma and cribriform carcinoma. In: Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van der Vijver MJ, editors. WHO classification of tumours of the breast. Lyon: International Agency for Research on Cancer; 2012. p. 43–45.
Carlson RW, Allred DC, Anderson BO, et al. Breast cancer. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2009;7:122–92.
WHO. International histological classification of tumours no. 2. Histological typing of breast tumours. 2nd ed. Geneva: World Health Organization; 1981. p. 19.
Enjoji M, Matsukuma A, Sakamoto G, et al. Invasive ductal carcinoma of the breast with a predominant intraductal component: cooperative clinicopathologic study in seven Japanese centers. Jpn J Clin Oncol. 1992;22:84–91.
Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24:3726–34.
Acknowledgments
This work was supported in part by the National Cancer Center Research and Development Fund (22-5), the Grant-in-Aid for Scientific Research (C) from Japan Society for the Promotion of Science (22501039), and Grant-in-Aid for the Third-Term Comprehensive 10-Year Strategy for Cancer Control from the Ministry of Health, Labor, and Welfare, Japan (H22-023). We thank Sachiko Miura, M.T., Chizu Kina, M.T., Ms. Chinami Onuma (National Cancer Center Hospital), and Ms. Kozue Suzuki (National Defense Medical College) for technical support.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ono, M., Tsuda, H., Yunokawa, M. et al. Prognostic impact of Ki-67 labeling indices with 3 different cutoff values, histological grade, and nuclear grade in hormone-receptor-positive, HER2-negative, node-negative invasive breast cancers. Breast Cancer 22, 141–152 (2015). https://doi.org/10.1007/s12282-013-0464-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-013-0464-4