Abstract
Purpose of Review
To perform an extensive review of recent literature and provide an update on the current epidemiology, clinical features, and management of cryptococcal disease with a focus on the differences between patients depending on their immune status.
Recent Findings
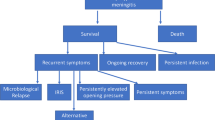
Emerging literature has highlighted the inflammatory pathophysiology and varied manifestations of cryptococcal infections in patients who are apparently healthy but paradoxically have a more critical clinical course compared with their immunosuppressed counterparts.
Summary
Non-HIV cryptococcal meningitis has greater mortality compared with that seen in HIV patients. Basic science experiments closely analyzing the underlying pathophysiological response to this infection have demonstrated the predominant role of T cell–mediated inflammatory injury in causing worse clinical outcomes. Further studies are needed to define the need for immunosuppressive agents in the treatment of this illness.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lui G, et al. Cryptococcosis in apparently immunocompetent patients. QJM. 2006;99(3):143–51. https://doi.org/10.1093/qjmed/hcl014.
Bennett JE, et al. A comparison of amphotericin B alone and combined with flucytosine in the treatment of cryptoccal meningitis. N Engl J Med. 1979;301(3):126–31. https://doi.org/10.1056/NEJM197907193010303.
Mirza SA, et al. The changing epidemiology of cryptococcosis: an update from population-based active surveillance in 2 large metropolitan areas, 1992–2000. Clin Infect Dis. 2003;36(6):789–94. https://doi.org/10.1086/368091.
Rajasingham R, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis. 2017;17(8):873–81. https://doi.org/10.1016/S1473-3099(17)30243-8.
Kwon-Chung KJ, et al. Cryptococcus neoformans and Cryptococcus gattii, the etiologic agents of cryptococcosis. Cold Spring Harb Perspect Med. 2014;4(7):a019760. https://doi.org/10.1101/cshperspect.a019760.
Gast CE, et al. Azole resistance in Cryptococcus gattii from the Pacific Northwest: investigation of the role of ERG11. Antimicrob Agents Chemother. 2013;57(11):5478–85. https://doi.org/10.1128/AAC.02287-12.
• Williamson PR, et al. Cryptococcal meningitis: epidemiology, immunology, diagnosis and therapy. Nat Rev Neurol. 2017;13(1):13–24. https://doi.org/10.1038/nrneurol.2016.167 An updated review of the epidemiology, immune pathology, and clinical management strategies for HIV-associated and HIV-seronegative cryptococcal meningitis patients.
Hagen F, et al. Importance of resolving fungal nomenclature: the case of multiple pathogenic species in the Cryptococcus genus. mSphere. 2017;2(4). https://doi.org/10.1128/mSphere.00238-17.
Kwon-Chung KJ, et al. The case for adopting the “Species Complex” nomenclature for the etiologic agents of cryptococcosis. mSphere. 2017;2(1). https://doi.org/10.1128/mSphere.00357-16.
Chen S, et al. Epidemiology and host- and variety-dependent characteristics of infection due to Cryptococcus neoformans in Australia and New Zealand. Australasian Cryptococcal Study Group. Clin Infect Dis. 2000;31(2):499–508. https://doi.org/10.1086/313992.
Vu K, Garcia JA, Gelli A. Cryptococcal meningitis and anti-virulence therapeutic strategies. Front Microbiol. 2019;10:353. https://doi.org/10.3389/fmicb.2019.00353.
Waterman SR, et al. Role of CTR4 in the virulence of Cryptococcus neoformans. MBio. 2012;3(5). https://doi.org/10.1128/mBio.00285-12e00285-12.
Chen S, Williamson P. Lessons from cryptococcal laccase: from environmental saprophyte to pathogen. Curr Fungal Infect Rep. 2011;5:233–44.
Olave MC, et al. Infective capacity of Cryptococcus neoformans and Cryptococcus gattii in a human astrocytoma cell line. Mycoses. 2017;60(7):447–53. https://doi.org/10.1111/myc.12619.
Garcia-Hermoso D, Janbon G, Dromer F. Epidemiological evidence for dormant Cryptococcus neoformans infection. J Clin Microbiol. 1999;37(10):3204–9.
Lin X. Cryptococcus neoformans: morphogenesis, infection, and evolution. Infect Genet Evol. 2009;9(4):401–16. https://doi.org/10.1016/j.meegid.2009.01.013.
Saha DC, et al. Serologic evidence for reactivation of cryptococcosis in solid-organ transplant recipients. Clin Vaccine Immunol. 2007;14(12):1550–4. https://doi.org/10.1128/CVI.00242-07.
Charlier C, et al. Evidence of a role for monocytes in dissemination and brain invasion by Cryptococcus neoformans. Infect Immun. 2009;77(1):120–7. https://doi.org/10.1128/IAI.01065-08.
Araujo Gde S, et al. Capsules from pathogenic and non-pathogenic Cryptococcus spp. manifest significant differences in structure and ability to protect against phagocytic cells. PLoS One. 2012;7(1):e29561. https://doi.org/10.1371/journal.pone.0029561.
Park Y-D, et al. A role for LHC1 in higher order structure and complement binding of the Cryptococcus neoformans Capsule. PLoS Pathog. 2014;10(5):e1004037. https://doi.org/10.1371/journal.ppat.1004037.
He X, et al. Virulence factors identified by Cryptococcus neoformans mutant screen differentially modulate lung immune responses and brain dissemination. Am J Pathol. 2012;S0002–9440(12):00487–7. https://doi.org/10.1016/j.ajpath.2012.06.012.
Panepinto J, et al. Sec6-dependent sorting of fungal extracellular exosomes and laccase of Cryptococcus neoformans. 2008.
• Almeida F, Wolf JM, Casadevall A. Virulence-associated enzymes of Cryptococcus neoformans. Eukaryot Cell. 2015;14(12):1173–85. https://doi.org/10.1128/EC.00103-15 A review of newly discovered enzymatic mechanisms through which Cryptococcus neoformans adapts to survive and infect mammalian hosts.
• Panackal AA, et al. Susceptibility to cryptococcal meningoencephalitis associated with idiopathic CD4(+) lymphopenia and secondary germline or acquired defects. Open Forum Infect Dis. 2017;4(2):ofx082. https://doi.org/10.1093/ofid/ofx082 Two case studies of patients with idiopathic CD4+ lymphopenia (ICL) and opportunistic cryptococcal meningoencephalitis infections with an immunological focus on the E57K genetic mutation and acquired granulocyte-macrophage colony-stimulating factor autoantibodies.
Zonios DI, et al. Cryptococcosis and idiopathic CD4 lymphocytopenia. Medicine (Baltimore). 2007;86(2):78–92. https://doi.org/10.1097/md.0b013e31803b52f5.
•• Elsegeiny W, Marr KA, Williamson PR. Immunology of cryptococcal infections: developing a rational approach to patient therapy. Front Immunol. 2018;9:651. https://doi.org/10.3389/fimmu.2018.00651 New insights on immune activation in HIV-positive and previously healthy patients with cryptococcal meningoencephalitis to update treatment strategies.
•• Brizendine KD, Baddley JW, Pappas PG. Predictors of mortality and differences in clinical features among patients with cryptococcosis according to immune status. PLoS One. 2013;8(3):e60431. https://doi.org/10.1371/journal.pone.0060431 A retrospective cohort study of 302 patients with cryptococcosis that identifies cryptococcemia, high intracranial pressure, and a non-HIV, non-transplant immune status as predictive markers for mortality.
•• Panackal AA, et al. Paradoxical immune responses in non-HIV cryptococcal meningitis. PLoS Pathog. 2015;11(5):e1004884. https://doi.org/10.1371/journal.ppat.1004884 This immunological study higlights unusual findings of strong intrathecal expansion and activation of T cells involved in both innate and adaptive immunity in HIV-negative patients with cryptococcal meningoencephalitis.
•• Pirofski LA, Casadevall A. The damage-response framework of microbial pathogenesis and infectious diseases. Adv Exp Med Biol. 2008;635:135–46. https://doi.org/10.1007/978-0-387-09550-9_11 An overview of the damage-response framework explains how an imbalance in the host-microbe interaction can determine variable outcomes in different patients.
Shelburne SA 3rd, Hamill RJ. The immune reconstitution inflammatory syndrome. AIDS Rev. 2003;5(2):67–79.
Tugume L, et al. HIV-associated cryptococcal meningitis occurring at relatively higher CD4 counts. J Infect Dis. 2019;219(6):877–83. https://doi.org/10.1093/infdis/jiy602.
Legris T, et al. Immune reconstitution inflammatory syndrome mimicking relapsing cryptococcal meningitis in a renal transplant recipient. Transpl Infect Dis. 2011;13(3):303–8. https://doi.org/10.1111/j.1399-3062.2010.00592.x.
Neal LM, et al. CD4(+) T cells orchestrate lethal immune pathology despite fungal clearance during Cryptococcus neoformans meningoencephalitis. MBio. 2017;8(6). https://doi.org/10.1128/mBio.01415-17.
• Panackal AA, et al. Fighting the monster: applying the host damage framework to human central nervous system infections. MBio. 2016;7(1). https://doi.org/10.1128/mBio.01906-15 This review applies the host damage-response framework to nonviral generalized CNS infections, including cryptococcal meningitis in non-HIV-infected patients.
•• Balasko A, Keynan Y. Shedding light on IRIS: from pathophysiology to treatment of cryptococcal meningitis and immune reconstitution inflammatory syndrome in HIV-infected individuals. HIV Med. 2019;20(1):1–10. https://doi.org/10.1111/hiv.12676 A review of the pathophysiology of HIV-associated cryptococcal immune reconstitution inflammatory syndrome with the consideration of thalidomide as a targeted alternative for type 1 T helper (Th1) cell overcompensation.
• Liao CH, et al. Different presentations and outcomes between HIV-infected and HIV-uninfected patients with cryptococcal meningitis. J Microbiol Immunol Infect. 2012;45(4):296–304. https://doi.org/10.1016/j.jmii.2011.12.005 A retrospective study describing potential predictors of outcomes with findings of lower mortality rates in HIV-infected CM compared with non-HIV patients with CM.
• Bratton EW, et al. Comparison and temporal trends of three groups with cryptococcosis: HIV-infected, solid organ transplant, and HIV-negative/non-transplant. PLoS One. 2012;7(8):e43582. https://doi.org/10.1371/journal.pone.0043582 This study compares trends for cryptococcosis in patients with varying immune status with the main finding of an increased prevalence in HIV-uninfected cases.
• Nguyen MH, et al. Outcomes of central nervous system cryptococcosis vary with host immune function: results from a multi-center, prospective study. J Infect. 2010;61(5):419–26. https://doi.org/10.1016/j.jinf.2010.08.004 This observational study demonstrated significant differences in outcomes for CNS cryptococcosis in relation to host immune status with the main finding of a higher mortality rate in non-immunocompromised patients.
Pappas PG. Cryptococcal infections in non-HIV-infected patients. Trans Am Clin Climatol Assoc. 2013;124:61–79.
•• Marr KA, et al. A multicenter, longitudinal cohort study of cryptococcosis in HIV-negative people in the United States. Clin Infect Dis. 2019. https://doi.org/10.1093/cid/ciz193 This prospective cohort study identified declining Montreal Cognitive Assessment (MoCA) scores and subsequent long-term neurological sequelae in HIV-uninfected patients despite the use of antifungal therapy.
Spec A, et al. Cryptococcus Infection Network in Non-Human Immunodeficiency Virus Cohort (CINCH) study: initial report of treatment and outcomes. Open Forum Infect Dis. 2016;3(Suppl 1):122. https://doi.org/10.1093/ofid/ofw194.35.
Traino K. HIV-negative cryptococcal meningoencephalitis results in a persistent frontal-subcortical syndrome. Nat Sci Rep. 2019; (in press).
King KA, GA AAP, Zalewski C, Anjum S, Bennett JE, Beri A, et al. Audiologic and otologic complications of cryptococcal meningoencephalitis in non-HIV previously healthy patients. Otol Neurotol. 2019; (in press).
Panackal AA, et al. Spinal arachnoiditis as a complication of cryptococcal meningoencephalitis in non-HIV previously healthy adults. Clin Infect Dis. 2017;64(3):275–83. https://doi.org/10.1093/cid/ciw739.
O'Halloran JA, Powderly WG, Spec A. Cryptococcosis today: it is not all about HIV infection. Curr Clin Microbiol Rep. 2017;4(2):88–95. https://doi.org/10.1007/s40588-017-0064-8.
Pasquier E, et al. Long-term mortality and fisability in cryptococcal meningitis: a systematic literature review. Clin Infect Dis. 2018;66(7):1122–32. https://doi.org/10.1093/cid/cix870.
Chow E, Troy SB. The differential diagnosis of hypoglycorrhachia in adult patients. Am J Med Sci. 2014;348(3):186–90. https://doi.org/10.1097/MAJ.0000000000000217.
Komori M, et al. Cerebrospinal fluid markers reveal intrathecal inflammation in progressive multiple sclerosis. Ann Neurol. 2015;78(1):3–20. https://doi.org/10.1002/ana.24408.
Nalintya E, Kiggundu R, Meya D. Evolution of cryptococcal antigen testing: what is new? Curr Fungal Infect Rep. 2016;10(2):62–7. https://doi.org/10.1007/s12281-016-0256-3.
Jitmuang A, et al. Performance of the cryptococcal antigen lateral flow assay in non-HIV-related cryptococcosis. J Clin Microbiol. 2016;54(2):460–3. https://doi.org/10.1128/JCM.02223-15.
Liesman RM, et al. Evaluation of a commercial multiplex molecular panel for diagnosis of infectious meningitis and encephalitis. J Clin Microbiol. 2018;56(4). https://doi.org/10.1128/JCM.01927-17.
Hospenthal DR, Bennett JE. Persistence of cryptococcomas on neuroimaging. Clin Infect Dis. 2000;31(5):1303–6. https://doi.org/10.1086/317434.
Ellis JP, et al. Ischemic stroke as a complication of cryptococcal meningitis and immune reconstitution inflammatory syndrome: a case report. BMC Infect Dis. 2018;18(1):520. https://doi.org/10.1186/s12879-018-3386-0.
Hammoud DA, et al. Choroid plexitis and ependymitis by magnetic resonance imaging are biomarkers of neuronal damage and inflammation in HIV-negative cryptococcal meningoencephalitis. Sci Rep. 2017;7(1):9184. https://doi.org/10.1038/s41598-017-09694-0.
Takayanagui OM, Odashima NS. Clinical aspects of neurocysticercosis. Parasitol Int. 2006;55(Suppl):S111–5. https://doi.org/10.1016/j.parint.2005.11.016.
Schwarz P, et al. Efficacy of amphotericin B in combination with flucytosine against flucytosine-susceptible or flucytosine-resistant isolates of Cryptococcus neoformans during disseminated murine cryptococcosis. Antimicrob Agents Chemother. 2006;50(1):113–20. https://doi.org/10.1128/AAC.50.1.113-120.2006.
Diamond RD, Bennett JE. Prognostic factors in cryptococcal meningitis. A study in 111 cases. Ann Intern Med. 1974;80(2):176–81.
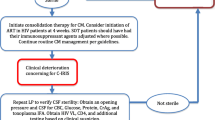
• Perfect JR, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(3):291–322. https://doi.org/10.1086/649858 IDSA clinical practice guidelines for cryptococcosis in HIV-infected individuals, organ transplant recipients, and non-HIV-infected (non-transplant) patients.
• Beardsley J, et al. Adjunctive dexamethasone in HIV-associated cryptococcal meningitis. N Engl J Med. 2016;374(6):542–54. https://doi.org/10.1056/NEJMoa1509024 This is a double-blind, randomized, placebo-controlled landmark trial of dexamethasone use in HIV-infected patients with cryptococcal meningitis that demonstrated no improvement in outcomes for the experimental group.
Liu J, et al. Ventriculoperitoneal shunts in non-HIV cryptococcal meningitis. BMC Neurol. 2018;18(1):58. https://doi.org/10.1186/s12883-018-1053-0.
Tellez RM, et al. Cerebral cryptococcosis and immune reconstitution inflammatory syndrome. Case report. Rev Med Chil. 2018;146(12):1481–5. https://doi.org/10.4067/s0034-98872018001201481.
• Mehta GU, et al. Corticosteroids for shunted previously healthy patients with non-HIV cryptococcal meningoencephalitis. J Neurol Neurosurg Psychiatry. 2018;89(2):219–20. https://doi.org/10.1136/jnnp-2017-315830 This letter details the successful use of corticosteroids as well as antifungal therapy to control post-infectious inflammatory response syndrome (PIIRS) and prevent long-term neurological complications in cryptococcal meningitis (CM) patients.
Lane M, McBride J, Archer J. Steroid responsive late deterioration in Cryptococcus neoformans variety gattii meningitis. Neurology. 2004;63(4):713–4.
Chen SC, et al. Antifungal therapy and management of complications of cryptococcosis due to Cryptococcus gattii. Clin Infect Dis. 2013;57(4):543–51. https://doi.org/10.1093/cid/cit341.
Kwon-Chung KJ, Bennett JE. Epidemiologic differences between the two varieties of Cryptococcus neoformans. Am J Epidemiol. 1984;120(1):123–30.
Pyrgos V, et al. Epidemiology of cryptococcal meningitis in the US: 1997–2009. PLoS One. 2013;8(2):e56269. https://doi.org/10.1371/journal.pone.0056269.
Loyse A, et al. Histopathology of the arachnoid granulations and brain in HIV-associated cryptococcal meningitis: correlation with cerebrospinal fluid pressure. AIDS. 2010;24(3):405–10. https://doi.org/10.1097/QAD.0b013e328333c005.
Graybill JR, et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. The NIAID Mycoses Study Group and AIDS Cooperative Treatment Groups. Clin Infect Dis. 2000;30(1):47–54. https://doi.org/10.1086/313603.
Park MK, Hospenthal DR, Bennett JE. Treatment of hydrocephalus secondary to cryptococcal meningitis by use of shunting. Clin Infect Dis. 1999;28(3):629–33. https://doi.org/10.1086/515161.
Calligaro G, Meintjes G, Mendelson M. Pulmonary manifestations of the immune reconstitution inflammatory syndrome. Curr Opin Pulm Med. 2011;17(3):180–8. https://doi.org/10.1097/MCP.0b013e328344f692.
Hu Z, et al. Radiological characteristics of pulmonary cryptococcosis in HIV-infected patients. PLoS One. 2017;12(3):e0173858. https://doi.org/10.1371/journal.pone.0173858.
Jenny-Avital ER, Abadi M. Immune reconstitution cryptococcosis after initiation of successful highly active antiretroviral therapy. Clin Infect Dis. 2002;35(12):e128–33. https://doi.org/10.1086/344467.
Gates-Hollingsworth MA, Kozel TR. Serotype sensitivity of a lateral flow immunoassay for cryptococcal antigen. Clin Vaccine Immunol. 2013;20(4):634–5. https://doi.org/10.1128/CVI.00732-12.
Funding
This research was supported in part by the Intramural Research Program of the NIH, grant funding numbers AI001123 and AI00112.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Fungal Genomics and Pathogenesis
Rights and permissions
About this article
Cite this article
Anjum, S., Williamson, P.R. Clinical Aspects of Immune Damage in Cryptococcosis. Curr Fungal Infect Rep 13, 99–108 (2019). https://doi.org/10.1007/s12281-019-00345-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-019-00345-7