Abstract
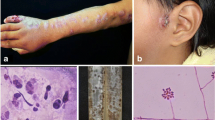
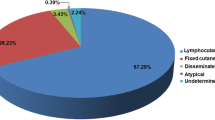
Lymphocutaneous sporotrichosis is the most common clinical form of cutaneous sporotrichosis. Caused by a complex of dimorphic fungi called Sporothrix schenckii complex, it is an occupational disease, present especially in tropical and subtropical areas, and has been reported in all continents. Diagnosis is established by isolation of the causative agent. Therapy of choice for lymphocutaneous sporotrichosis is itraconazole, and in developing countries, potassium iodide solution. In general, the lymphocutaneous form is considered a mild benign form of the disease, and the majority of cases respond well to treatment in about 3–4 months of therapy. In this paper, we have made a general review of the disease, especially of the epidemiology, clinical features and diagnosis of the lymphocutaneous form, as well as a brief analysis of the advantages and disadvantages of diverse treatments.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kauffman CA. Sporotrichosis. Clin Infect Dis. 1999;29:231–7.
•• Barros MB, de Almeida PR, Shubach AO. Sporothrix schenckii and Sporotrichosis. Clin Microbiol Rev. 2011;24:633–54. A complete review of the disease and the etiological agent.
Schechtman RC. Sporotrichosis: Part I. Skinmed. 2010;8:216–20.
• Bonifaz A, Vázquez-González D. Sporotrichosis: an update. G Ital Dermatol Venereol. 2010;145:659–73. A review of the disease, all its clinical forms, diagnosis and treatment.
da Rosa AC, Scroferneker ML, Vettorato R, et al. Epidemiology of sporotrichosis: a study of 304 cases in Brazil. J Am Acad Dermatol. 2005;52(3 pt1):451–599.
Marimon R, Cano J, Gene J, et al. Sporothrix brasiliensis, S. globosa, and S. mexicana, three new Sporothrix species of clinical interest. J Clin Microbiol. 2007;45:3198–206.
• Rodrigues AM, de Hoog S, de Camargo ZP. Emergence of pathogenicity in the Sporothrix schenckii complex. Med Mycol. 2012 Sep 19: 1–8. PMID: 22989196. This study evaluated the differences among these species found frequency in the environment and in human hosts, and discuss their diverse pathogenicity.
Hajjeh R, McDonnell S, Reef S, et al. Outbreak of sporotrichosis among tree nursery workers. J Infect Dis. 1997;176:499–504.
Hay RJ, Morris-Jones R. Outbreaks of sporotrichosis. Curr Opin Infect Dis. 2008;21:119–21.
Schubach A, Barros MB, Wanke B. Epidemic sporotrichosis. Curr Opin Infect Dis. 2008;21:129–33.
Song Y, Li SS, Zhong SX, et al. Report of 457 sporotrichosis cases from Jilin province, northeast China, a serious endemic region. J Eur Acad Dermatol Venereol. 2013;22:313–8.
Barros MB, Costa DL, Schubach TM, et al. Endemic of zoonotic sporotrichosis: profile of cases in children. Pediatr Infect Dis J. 2008;3:246–50.
Freitas DF. do Valle AC, de Almeida Paes R, et al. Zoonotic Sporotrichosis in Rio de Janeiro, Brazil: a protracted epidemic yet to be curbed. Clin Infect Dis. 2010;50:453.
Bonifaz A, Saúl A, Paredes-Solís V, et al. Sporotrichosis in childhood. Clinical and therapeutic experience in 25 cases. Pediatr Dermatol. 2007;24:369–72.
Pappas PG, Tellez I, Deep AE, et al. Sporotrichosis in Peru: description of an area of hyperendemicity. Clin Infect Dis. 2000;30:65–70.
• López-Romero E, Reyes-Montes Mdel R, Pérez-Torres A, et al. Sporothrix schenckii complex and sporotrichosis, an emerging health problem. Future Microbiol. 2011;6:85–102. A review on the increase of sporotrichosis and how it is becoming a public health problem in some areas.
Marimon R, Serena C, Gené J, et al. In vitro antifungal susceptibilities of five species of Sporothrix. Antimicrob Agents Chemother. 2008;52:732–4.
• Zhang X, Huang H, Feng P, et al. In vitro activity of itraconazole in combination with terbinafine against clinical strains of itraconazole-insensitive Sporothrix schenckii. Eur J Dermatol. 2011;21:573–36. This in- vitro study proves synergism of itraconazole and terbinafine.
Vásquez-del-Mercado E, Arenas R, Padilla-Desgarennes C. Sporotrichosis. Clin Dermatol. 2012;30:437–43.
Takenaka M, Sato S, Nishimoto K. Survey of 155 sporotrichosis cases examined in Nagasaki Prefecture from 1951 to 2007. Nihon Ishinkin Gakkai Zasshi. 2009;50:101–8.
Bustamante B, Campos PE. Endemic sporotrichosis. Curr Opin Infect Dis. 2001;14:145–9.
Madrid IM, Mattei A, Martins A, et al. Feline sporotrichosis in the southern region of rio grande do sul, Brazil: clinical, zoonotic and therapeutic aspects. Zoonoses Public Health. 2010;57:151–4.
Orofino-Costa R, Bóia MN, Magalhães GA, et al. Arthritis as a hypersensitivity reaction in a case of sporotrichosis transmitted by a sick cat: clinical and serological follow up of 13 months. Mycoses. 2010;53:81–3.
Liu X, Zhang Z, Hou B, et al. Rapid identification of Sporothrix schenckii in biopsy tissue by PCR. J Eur Acad Dermatol Venereol. 2012. doi:10.1111/jdv.12030.
Hu S, Chung WH, Hung SI. Detection of Sporothrix schenckii in clinical samples by a nested PCR assay. J Clin Microbiol. 2003;41:1414–8.
Kawasaki M, Anzawa K, Mochizuki T, Ishizaki H. New strain typing method with Sporothrix schenckii using mitochondrial DNA and polymerase chain reaction restriction fragment length polymorphism (PCR-RFLP) technique. J Dermatol. 2012;39:362–5.
Zhang YQ, Xu XG, Zhang M, et al. Sporotrichosis: clinical and histopathological manifestations. Am J Dermatopathol. 2011;33:296–302.
Novales SJ, Navarrete FG, Ramos GA. Esporotricosis. Aspectos histológicos de 50 casos. Rev Centr Dermatol Pascua. 1995;4:149–52.
• Quintella LP, Passos SR, do Vale AC, et al. Histopathology of cutaneous sporotrichosis in Rio de Janeiro: a series of 119 consecutive cases. J Cutan Pathol. 2011;38:25–32. A large series of sporotrichosis and histopathological behavior.
Bustamante B, Campos PE. Sporotrichosis: a forgotten disease in the drug research agenda. Expert Rev Anti Infect Ther. 2004;2:85–94.
Schechtman RC. Sporotrichosis: Part II. Skinmed. 2010;8:275–80.
Cabezas C, Bustamante B, Holgado W, Begue RE. Treatment of cutaneous sporotrichosis with one daily dose of potassium iodide. Pediatr Infect Dis J. 1996;15:352–4.
Xue SL, Li L. Oral potassium iodide for the treatment of sporotrichosis. Mycopathologia. 2009;167:355–6.
• Yamada K, Zaitz C, Framil VM, Muramatu LH. Cutaneous sporotrichosis treatment with potassium iodide: a 24 year experience in São Paulo State, Brazil. Rev Inst Med Trop Sao Paulo. 93;53:89. A large experience of the potassium iodide treatment.
Kauffman CA, Bustamante B, Chapman SW, et al. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45:1255–65.
Xiao T, Lin J, Chen HD. Prominent facial edema caused by potassium iodide solution in a patient with sporotrichosis. J Dermatol. 2009;36:111–3.
Conti-Díaz IA, Civila E, Gezuele E, et al. Treatment of human cutaneous sporotrichosis with itraconazole. Mycoses. 1992;35:153–6.
Sharkey-Mahis PK, Kauffman CA, Grabyl JR, et al. Treatment of sporotrichosis with itraconazole. Am J Med. 1993;95:279–85.
Baroni A, Palla M, Iovene MR, et al. Sporotrichosis: success of itraconazole treatment. Skinmed. 2007;6:41–4.
•• de Lima Barros MB, Schubach AO, de Vasconcellos Carvalhaes de Oliveira R, et al. Treatment of cutaneous sporotrichosis with itraconazole--study of 645 patients. Clin Infect Dis. 2011;52:200–6. The largest series reported on the experience of itraconazole in skin sporotrichosis.
Bonifaz A, Fierro L, Saúl A, Ponce RM. Cutaneous sporotrichosis. Intermittent treatment (pulses) with itraconazole. Eur J Dermatol. 2007;18:61–4.
• Song Y, Zhong SX, Yao L, et al. Efficacy and safety of itraconazole pulses vs. continuous regimen in cutaneous sporotrichosis. J Eur Acad Dermatol Venereol. 2011;25:302–5. The only study comparing itraconazole continuous therapy and intermittent or pulse treatment.
Kauffman CA, Pappas PG, McKinsey DS, et al. Treatment of lymphocutaneous and visceral sporotrichosis with fluconazole. Clin Infect Dis. 1996;22:46–50.
Castro LG, Belda W, Cucé LC, et al. Successful treatment of sporotrichosis with oral fluconazole: a report of three cases. Br J Dermatol. 1993;128:352–6.
Chapman SW, Pappas P, Kauffman C, et al. Comparative evaluation of the efficacy and safety of two doses of terbinafine (500 and 1000 mg/day) in the treatment of cutaneous or lymphocutaneous sporotrichosis. Mycoses. 2004;47:62–8.
Francesconi G, Valle AC, Passos S, Reis R, Galhardo MC. Terbinafine (250 mg/day): an effective and safe treatment of cutaneous sporotrichosis. J Eur Acad Dermatol Venereol. 2009;23:1273–6.
Antunes Tde A, Nobre Mde O, Faria RO, et al. Experimental cutaneous sporotrichosis: in vivo evaluation of itraconazole and terbinafine. Rev Soc Bras Med Trop. 2009;42:706–10.
Heidrich D, Stopiglia CD, Senter L, et al. Successful treatment of terbinafine in a case of sporotrichosis. An Bras Dermatol. 2011;86(4 Suppl 1):S182–185.
•• Francesconi G, Francesconi do Valle AC, Passos SL, et al. Comparative study of 250 mg/day terbinafine and 100 mg/day itraconazole for the treatment of cutaneous sporotrichosis. Mycopathologia. 2011;171:349–54. The only comparative study between itraconazole and terbinafine in the management of sporotrichosis.
Cullen S, Maucer AA, Warner N. Successful treatment of disseminated cutaneous sporotrichosis with ketoconazole. J Am Acad Dermatol. 1992;27:463–4.
Fernández-Silva F, Capilla J, Mayayo E, Guarro J. Efficacy of posaconazole in murine experimental sporotrichosis. Antimicrob Agents Chemother. 2012;56:2273–7.
Bunce PE, Yang L, Chun S, et al. Disseminated sporotrichosis in a patient with hairy cell leukemia treated with amphotericin B and posaconazole. Med Mycol. 2012;50:197–201.
Pavón N, Bonifaz A, Ponce RM. Termoterapia en esporotricosis cutánea infantil. Comunicación de dos cases. Dermatología Rev Mex. 2007;51:68–72.
Badgwell Doherty C, Doherty SD, Rosen T. Thermotherapy in dermatologic infections. J Am Acad Dermatol. 2010;62:909–27.
Ferreira CP, Galhardo MC, Valle AC. Cryosurgery as adjuvant therapy in cutaneous sporotrichosis. Braz J Infect Dis. 2011;15:181–3.
Conflict of Interest
Alexandro Bonifaz declares that he has no conflict of interest.
Denisse Vázquez-González declares that she has no conflict of interest.
Financial support
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonifaz, A., Vázquez-González, D. Diagnosis and Treatment of Lymphocutaneous Sporotrichosis: What Are the Options?. Curr Fungal Infect Rep 7, 252–259 (2013). https://doi.org/10.1007/s12281-013-0140-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-013-0140-3