Abstract
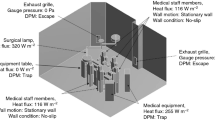
This study investigates effect of exhaust outlet location on airflow and particle distribution in an operating room with laminar ventilation system (LAF) via computational fluid dynamics (CFD). Four different exhaust opening configurations are comparatively examined: floor level, central level, ceiling level and floor & ceiling level. Three different particle diameters (5,10 and 20 μm) are considered for a constant value of the air change rate (30 ACH). Deposited particle numbers to operating table and to instrument table are given and compared for different particle diameters and exhaust outlet cases. It is shown that the exhaust configuration in which both floor & ceiling level air outlets employed together shows the best performance in terms of lowest particle deposition to the operating table. For this case, compared to original floor level exhaust outlet design, the total number of particles deposited on the operating table decreased by 64% for the smallest particle diameter (5 μm) and 26% for the largest particle diameter (20 μm).
Similar content being viewed by others
References
Aganovic A, Cao G, Stenstad LI, Skogås JG (2017). Impact of surgical lights on the velocity distribution and airborne contamination level in an operating room with laminar airflow system. Building and Environment, 126: 42–53.
Agirman A, Cetin YE, Avci M, Aydin O (2019). Influence of ceiling height on airflow and particle distribution in an operating room. E3S Web of Conferences, 111: 01032.
Ahmed AQ, Gao S, Kareem AK (2016). A numerical study on the effects of exhaust locations on energy consumption and thermal environment in an office room served by displacement ventilation. Energy Conversion and Management, 117: 74–85.
Alfonso-Sanchez JL, Martinez IM, Martin-Moreno JM, Gonzalez RS, Botia F (2017). Analyzing the risk factors influencing surgical site infections: The site of environmental factors. Canadian Journal of Surgery, 60: 155–161.
Allegranzi B, Nejad SB, Combescure C, Graafmans W, Attar H, Donaldson L, Pittet D (2011). Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. The Lancet, 377: 228–241.
ANSYS (2013). Ansys Fluent Theory Guide. Canonsburg, PA, USA: ANSYS Inc.
Balocco C, Petrone G, Cammarata G, Vitali P, Albertini R, Pasquarella C (2014). Indoor air quality in a real operating theatre under effective use conditions. Journal of Biomedical Science and Engineering, 7: 866–883.
Belani KG, Albrecht M, McGovern PD, Reed M, Nachtsheim C (2013). Patient warming excess heat. The effects on orthopedic operating room ventilation performance. Anesthesia & Analgesia, 117:406-411.
Berrios-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, et al. (2017). Centers for disease control and prevention guideline for the prevention of surgical site infection. JAMA Surgery, 152: 784.
Bouilly J, Limam K, Béghein C, Allard F (2005). Effect of ventilation strategies on particle decay rates indoors: an experimental and modelling study. Atmospheric Environment, 39: 4885–4892.
Broex ECJ, van Asselt ADI, Bruggeman CA, van Tiel FH (2009). Surgical site infections: how high are the costs? Journal of Hospital Infection, 72: 193–201.
Brown BH, Smallwood RH, Barber DC, Lawford PV, Hose DR (2017). Medical Physics and Biomedical Engineering. Boca Raton, FL, USA: CRC Press.
Cao G, Storas MCA, Aganovic A, Stenstad LI, Skogås JG (2018). Do surgeons and surgical facilities disturb the clean air distribution close to a surgical patient in an orthopedic operating room with laminar airflow? American Journal of Infection Control, 46: 1115–1122.
Chen Q, Jiang Z, Moser A (1992). Control of airborne particle concentration and draught risk in an operating room. Indoor Air, 2: 154–167.
Chow TT, Yang XY (2003). Performance of ventilation system in a non-standard operating room. Building and Environment, 38: 1401–1411.
Chow TT, Yang XY (2005). Ventilation performance in the operating theatre against airborne infection: numerical study on an ultra-clean system. Journal of Hospital Infection, 59: 138–147.
Chow TT, Lin Z, Bai W (2006). The integrated effect of medical lamp position and diffuser discharge velocity on ultra-clean ventilation performance in an operating theatre. Indoor and Built Environment, 15:315-331.
Chow TT, Wang J (2012). Dynamic simulation on impact of surgeon bending movement on bacteria-carrying particles distribution in operating theatre. Building and Environment, 57: 68–80.
Diab-Elschahawi M, Berger J, Blacky A, Kimberger O, Oguz R, Kuelpmann R, Kramer A, Assadian O (2011). Impact of different-sized laminar air flow versus no laminar air flow on bacterial counts in the operating room during orthopedic surgery. American Journal of Infection Control, 39: e25–e29.
DIN (2008). DIN 1946-4. Ventilation and air conditioning, Part 4: Ventilation in buildings and rooms of heatlhcare. Berlin: Deutsches Institut für Normung.
Eslami J, Abbassi A, Saidi MH, Bahrami M (2016). Effect of supply/exhaust diffuser configurations on the contaminant distribution in ultra clean environments: Eulerian and Lagrangian approaches. Energy and Buildings, 127: 648–657.
Feigley CE, Bennett JS, Khan J, Lee E (2002). Performance of deterministic workplace exposure assessment models for various contaminant source, air inlet, and exhaust locations. AIHA Journal, 63: 402–412.
Fischer S, Thieves M, Hirsch T, Fischer KD, Hubert H, Beppler S, Seipp HM (2015). Reduction of airborne bacterial burden in the OR by installation of unidirectional displacement airflow (UDF) systems. Medical Science Monitor, 21: 2367–2374.
Fry DE (2011). Fifty ways to cause surgical site infections. Surgical Infections, 12: 497–500.
Hinds WC (1999). Aerosol Technology: Properties, Behaviour, and Measurements of Airborne Particles, 2nd edn. New York: John Wiley & Sons.
Ho SH, Rosario L, Rahman MM (2009). Three-dimensional analysis for hospital operating room thermal comfort and contaminant removal. Applied Thermal Engineering, 29: 2080–2092.
Hoffman PN, Williams J, Stacey A, Bennett AM, Ridgway GL, Dobson C, Fraser I, Humphreys H (2002). Microbiological commissioning and monitoring of operating theatre suites. Journal of Hospital Infection, 52: 1–28.
Jin M, Memarzadeh F, Lee K, Chen Q (2012). Experimental study of ventilation performance in laboratories with chemical spills. Building and Environment, 57: 327–335.
Jurelionis A, Gagyte L, Prasauskas T, Ciuzas D, Krugly E, Seduikytè L, Martuzevicius D (2015). The impact of the air distribution method in ventilated rooms on the aerosol particle dispersion and removal: The experimental approach. Energy and Buildings, 86: 305–313.
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012). Economic burden of periprosthetic joint infection in the United States. The Journal of Arthroplasty, 27: 61–65.e1.
Legg AJ, Cannon T, Hamer AJ (2012). Do forced air patient-warming devices disrupt unidirectional downward airflow? The Journal of Bone and Joint Surgery British Volume, 94-B: 254–256.
Legg AJ, Hamer AJ (2013). Forced-air patient warming blankets disrupt unidirectional airflow. The Bone & Joint Journal, 95-B: 407–410.
Li X, Yan Y, Shang Y, Tu J (2015). An Eulerian-Eulerian model for particulate matter transport in indoor spaces. Building and Environment, 86: 191–202.
Lin T, Tung Y-C, Hu S-C, Lin C-Y (2010). Effects of the removal of 0.1 urn particles in industrial cleanrooms with a fan dry coil unit (FDCU) return system. Aerosol and Air Quality Research, 10: 571–580.
Ling JH (2005). Study on operating room air purification effectiveness. PhD Thesis, Tianjin University, China.
Liu DL (2010). Particle deposition onto enclosure surfaces. In: Kohli R, Mittal KL (eds), Developments in Surface Contamination and Cleaning: Particle Deposition, Control and Removal. Norwich, NY: William Andrew Publishing, pp. 1–56.
Lydon GP, Ingham DB, Mourshed MM (2014). Ultra clean ventilation system performance relating to airborne infections in operating theatres using CFD modelling. Building Simulation, 7: 277–287.
MacInnes JM, Bracco FV (1992). Stochastic particle dispersion modeling and the tracer-particle limit. Physics of Fluids A: Fluid Dynamics, 4: 2809–2824.
Mangram AJ, Horan TC, Pearson ML, Silver LC, William R (2000). Guideline for prevention of surgical site infection. Bulletin of the American College of Surgeons, 85: 23–29.
Mathijssen NMC, Hannink G, Sturm PDJ, Pilot P, Bloem RM, Buma P, Petit PLC, Schreurs BW (2016). The effect of door openings on numbers of colony forming units in the operating room during hip revision surgery. Surgical Infections, 17: 535–540.
Mears SC, Blanding R, Belkoff SM (2015). Door opening affects operating room pressure during joint arthroplasty. Orthopedics, 38: e991–e994.
Memarzadeh F, Jiang Z (2004). Effect of operation room geometry and ventilation system parameter variations on the protection of the surgical site. In: Proceedings of IAQ Conference.
Memarzadeh F, Xu W (2012). Role of air changes per hour (ACH) in possible transmission of airborne infections. Building Simulation, 5: 15–28.
Noble WC (1975). Dispersal of skin microorganisms. British Journal of Dermatology, 93: 477–485.
Noble WC (1976). Dispersal of bacteria from human skin. In: Proceedings of the International Symposium on Contamination Control.
Richmond-Bryant J, Eisner AD, Brixey LA, Wiener RW (2006). Transport of airborne particles within a room. Indoor Air, 16: 48–55.
Romano F, Marocco L, Gustén I, Joppolo CM (2015). Numerical and experimental analysis of airborne particles control in an operating theater. Building and Environment, 89: 369–379.
Sadrizadeh S, Holmberg S, Tammelin A (2014a). A numerical investigation of vertical and horizontal laminar airflow ventilation in an operating room. Building and Environment, 82: 517–525.
Sadrizadeh S, Tammelin A, Ekolind P, Holmberg S (2014b). Influence of staff number and internal constellation on surgical site infection in an operating room. Particuology, 13: 42–51.
Sadrizadeh S, Holmberg S (2015). How safe is it to neglect thermal radiation in indoor environment modeling with high ventilation rates? In: Proceedings of the 36th AIVC, 5th TightVent & 3rd venticool Conference.
Santa Cruz A, Coste N, Makhloufi R, Guillou S, Delboulbé E, Tiffonnet A-L, Marion M (2011). Airflow inside an open ventilated system: Influence of operator's arms or moving conveyor. Journal of Food Engineering, 105: 197–209.
Shih T-H, Liou WW, Shabbir A, Yang Z, Zhu J (1995). A new k-e eddy viscosity model for high Reynolds number turbulent flows. Computers & Fluids, 24: 227–238.
Smith EB, Raphael IJ, Maltenfort MG, Honsawek S, Dolan K, Younkins EA (2013). The effect of laminar air flow and door openings on operating room contamination. The Journal of Arthroplasty, 28: 1482–1485.
Srebric J, Vukovic V, He G, Yang X (2008). CFD boundary conditions for contaminant dispersion, heat transfer and airflow simulations around human occupants in indoor environments. Building and Environment, 43: 294–303.
Stacey A, Humphreys H (2002). A UK historical perspective on operating theatre ventilation. Journal of Hospital Infection, 52: 77–80.
Teter J, Guajardo I, Al-Rammah T, Rosson G, Perl TM, Manahan M (2017). Assessment of operating room airflow using air particle counts and direct observation of door openings. American Journal of Infection Control, 45: 477–482.
WHO (2016). Global Guidelines for the Prevention of Surgical Site Infection. Geneva: World Health Organization.
Whyte W, Hodgson R, Tinkler J (1982). The importance of airborne bacterial contamination of wounds. Journal of Hospital Infection, 3: 123–135.
Whyte W, Shaw BH (1974). The effect of obstructions and thermals in laminar-flow systems. Journal of Hygiene, 72: 415–423.
Yin Y, Xu W, Gupta J, Guity A, Marmion P, Manning A, Gulick B, Zhang X, Chen Q (2009). Experimental study on displacement and mixing ventilation systems for a patient ward. HVAC&R Research, 15: 1175–1191.
Zamuner N (1986). Operating room environment with turbulent airflow. ASHRAE Transactions, 92: 343–349.
Zhai ZJ, Osborne AL (2013). Simulation-based feasibility study of improved air conditioning systems for hospital operating room. Frontiers of Architectural Research, 2: 468–475.
Zhang Z, Chen Q (2006). Experimental measurements and numerical simulations of particle transport and distribution in ventilated rooms. Atmospheric Environment, 40: 3396–3408.
Zhang Z, Chen Q (2007). Comparison of the Eulerian and Lagrangian methods for predicting particle transport in enclosed spaces. Atmospheric Environment, 41: 5236–5248.
Zhang R, Tu G, Ling J (2008). Study on biological contaminant control strategies under different ventilation models in hospital operating room. Building and Environment, 43: 793–803.
Zhao B, Yang C, Yang X, Liu S (2008). Particle dispersion and deposition in ventilated rooms: Testing and evaluation of different Eulerian and Lagrangian models. Building and Environment, 43: 388–397.
Zoon WAC, van der Heijden MGM, Loomans MGLC, Hensen JLM (2010). On the applicability of the laminar flow index when selecting surgical lighting. Building and Environment, 45: 1976–1983.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agirman, A., Cetin, Y.E., Avci, M. et al. Effect of air exhaust location on surgical site particle distribution in an operating room. Build. Simul. 13, 979–988 (2020). https://doi.org/10.1007/s12273-020-0642-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12273-020-0642-1