Abstract
Pneumonia is an inflammatory disease of the lung, responsible for high morbidity and mortality worldwide. It is caused by bacteria, viruses, fungi, or other microorganisms. Streptococcus pneumoniae, a gram-positive bacterium with over 90 serotypes, is the most common causative agent. Moreover, comorbid factors including heart failure, renal disease, and pulmonary disease could increase the risk of pneumococcal pneumonia. Since the advent of the pneumococcal vaccine in the 1980s, the incidence of pneumonia has decreased significantly. However, current vaccines confer only limited protection against serotypes included in the vaccine. Thus, to overcome this limitation, new types of pneumococcal vaccines have been sought and under clinical trials. In this review, we discuss pneumonia and summarize the various types of pneumococcal vaccines in progress.
Similar content being viewed by others
Introduction
In 2015, a World Health Organization (WHO) report showed that respiratory diseases including lower respiratory infections, chronic obstructive pulmonary disease (COPD), trachea/bronchus/lung cancers, and tuberculosis, comprised 4 of the top 10 causes of death in the world. In addition, lower respiratory infections, which are the deadliest communicable diseases, are the leading cause of death in low-income economies (WHO 2017a). According to the WHO and Europe Detailed Mortality Databases, respiratory diseases were responsible for 15% of deaths in the European Union (EU), with pneumonia being the leading cause.
Pneumonia is one of the leading causes of death (Jackson et al. 2004), and a common cause of sepsis, responsible for 50% of all episodes. Most people recover from pneumonia or do not exhibit the symptoms anymore. However, it can be a life-threatening for those with weak or compromised immune systems including infants, young children, the elderly, and people suffering from other chronic diseases (Lynch and Zhanel 2009). For example, hospital- acquired pneumonia has a particularly high mortality rate (ERS 2017). Moreover, most deaths during the post-neonatal stage (1–59 months) occur because of pneumonia (WHO 2017b). To reduce mortality rates worldwide, vaccination with the pneumococcal vaccine is highly recommended because S. pneumoniae is the most common causative agent of pneumonia (Musher and Thorner 2014). Thus, many types of pneumococcal vaccines have been developed and are undergoing clinical trials. However, no studies have examined pneumococcal vaccines that have been studied or investigated at the clinical trial stage. In this review, we summarize information regarding pneumonia, its causative agent, and the preventive pneumococcal vaccine.
Pneumonia
Pneumonia is a respiratory infection that accounts for high morbidity in young and old individuals with weakened immune systems (Fry et al. 2005). In addition, the presence of chronic underlying conditions contribute to a marked increase in pneumonia risk with age (Jackson et al. 2004; Fry et al. 2005).
The most common pneumonia is community acquired pneumonia (CAP) (Musher and Thorner 2014), which is caused by bacteria, viruses, and less commonly by fungi or other microorganisms (MayoClinic 2017). Unlike hospital-acquired pneumonia, which is acquired during or after hospitalization for other diseases, CAP can also be acquired by non-hospitalized individuals. S. pneumoniae, Haemophilus influenzae, Staphylococcus aureus, influenza virus, and pulmonary diseases including lung cancer are the main causative agents of pneumonia. Pseudomonas aeruginosa, Pneumocystis jirovecii, Moraxella catarrhalis, and other gram-negative bacteria are less common causative agents (Musher and Thorner 2014). Prior to the use of antibiotics, more than 75% of pneumonia cases were caused by S. pneumoniae (Musher and Thorner 2014). However, recent studies have revealed that only 5 to 15% of pneumonia cases in the United States (US) are caused by S. pneumoniae (Restrepo et al. 2008; Jain et al. 2015), whereas, in some other countries, S. pneumoniae is responsible for a higher proportion of cases (Musher and Thorner 2014; Gadsby et al. 2016).
Pneumonia shows a high incidence rate in hospitalized patients, older outpatients, and men of all ages (Jackson et al. 2004). In addition, there are various risk factors for pneumonia, including smoking, diabetes, heart failure, lung cancer, renal disease, COPD, and viral infection. For example, CAP incidence rates have coincided with influenza virus epidemics (Carvalho et al. 2009; Sheng et al. 2011). National statistical data also shows that the CAP pattern closely reflected the temporal pattern of death percentages attributed to pneumonia and influenza in the US (Jackson et al. 2004).
There are many pneumonia treatments available, such as antibiotics, breathing treatments, and oxygen therapy (Korsgaard et al. 2005; van der Poll and Opal 2009). However, people with weak immune systems are likely to have complications such as respiratory failure, uncontrolled inflammation (i.e., sepsis), and lung abscesses (CDC 2017). In addition, the emergence of antibiotic resistant strains is considered a serious problem (Kaplan and Mason 1998; Picazo 2009). Thus, preventing pneumonia occurrence through vaccination is important. Indeed, the pneumococcal vaccine and seasonal flu vaccine are recommended for all children and adults (KSID 2014).
The pneumococcal vaccine has been commercially available since 1983, and its use has reduced the burden of pneumococcal disease among children and the elderly. Moreover, the decline of CAP caused by pneumococcus in the US was due to universal pneumococcal vaccination in adults and children (Musher 2016). Thus, the Advisory Committee on Immunization Practices (ACIP) recommends pneumococcal vaccination for immunocompromised adults (Kim et al. 2017; Robinson et al. 2017) as for prevention of pneumonia.
S. pneumoniae
S. pneumoniae is a gram positive bacterium with over 90 serotypes (Kalin 1998). Until recently, 92 serotypes were identified (Kapatai et al. 2016). S. pneumoniae have been known as the most common cause of CAP (Steel et al. 2013; Bewick et al. 2012) and causative agent of pneumococcal diseases such as otitis media, meningitis, and bacteremia (Bogaert et al. 2004). S. pneumoniae can colonize the nasopharynx asymptomatically, but is one of the leading causes of high mortality and morbidity in infants, the elderly, and immunocompromised people (Black et al. 2010; Wunderink and Waterer 2014).
Specific serotypes may colonize the nasopharynx and become prevalent, depending on their invasiveness, indirectly reflecting epidemiologic changes (Flasche et al. 2011). In S. pneumoniae, many virulence factors could contribute to colonization and development of pneumococcal diseases (Kadioglu et al. 2008). Bacterial and host factors contributing to colonization have been defined in animal models (Kadioglu et al. 2008). In a mouse acute pneumonia model, pneumolysin (Ply) was an essential factor for bacterial survival in the respiratory tract (Kadioglu et al. 2008). Other virulence factors such as PspA, LytA, PsaA, PiaA, and NanA also play a leading role in respiratory tract infection and pneumonia (Kadioglu et al. 2008).
Pneumolysin, a cytolytic toxin, is a well-known virulence factor of S. pneumoniae. It functions as a Toll-like receptor ligand, activates the complement pathway, and stimulates various inflammatory cytokines (Hirst et al. 2004). LytA, also known as autolysin, digests the cell wall and releases pneumolysin and other cellular contents (van der Poll and Opal 2009). Moreover, it inhibits C3 convertase formation (Andre et al. 2017). PsaA, pneumococcal surface antigen A, is involved in metal ion uptake, which leads to protection from oxidative stress (Kadioglu et al. 2008). PiaA, pneumococcal iron acquisition A, is another component of the ATP-binding cassette transport system and is involved in the acquisition of iron for bacterial growth (van der Poll and Opal 2009). Finally, NanA, a neuraminidase that is also known as sialidase, cleaves the terminal sialic acid, which promotes adhesion and colonization (Kadioglu et al. 2008). This molecule also deglycosylates complement components to evade the host complement pathway (Andre et al. 2017).
Factors increasing pneumonia risk in pneumococcal infections
Influenza virus, respiratory syncytial virus, parainfluenza virus, adenovirus, and coronavirus are commonly detected in patients with CAP, but it may be unclear to what extent any of these organisms are causing the disease or have predisposed the patient to secondary bacterial infection (Johnstone et al. 2008; Pavia 2013).
When influenza A virus is serially infected with bacteria, its lethality is increased (Mina and Klugman 2013). For example, pneumococcal coinfection was responsible for high mortality during the 2009 H1N1 pandemic (Monsalvo et al. 2011). Moreover, it has been reported that influenza virus coinfection comprises 22% of CAP cases (Michelow et al. 2004).
Although influenza virus and pneumococcus coinfection is responsible for higher mortality and morbidity, the current pneumococcal conjugate vaccine does not provide sufficient protection in the serial coinfection model (Metzger et al. 2015). Therefore, the development of a new type of vaccine, which can protect against influenza virus and pneumococcus coinfection, is required.
Pneumococcal vaccine
The pneumococcal vaccine is divided into whole cell vaccine and subunit. Whole cell vaccine included live attenuated vaccine and inactivated vaccine, and subunit vaccine included polysaccharide vaccine, conjugate vaccine and protein based vaccine. Commercially available pneumococcal vaccines are belonging in subunit vaccine. PPV23 and PCV13 is available pneumococcal vaccine in the marker in recent. Pediatric pneumococcal disease incidence was already successfully reduced after the introduction of the conjugate pneumococcal vaccine (Vila-Corcoles and Ochoa-Gondar 2013). However, current pneumococcal vaccine usage increases prevalence of pneumococcal diseases induced by serotypes not included in the vaccine (Flannery et al. 2006; Croucher et al. 2013). In addition, pneumococcal disease in the elderly remained a considerable burden, despite PPV23 vaccination. Thus, immunization with both the PCV13 and PPV23 vaccines is recommended in the elderly (Hayward et al. 2016) to overcome the disadvantages of each vaccine (Table 1). Indeed, combination of current pneumococcal vaccines produces a superior immune response than PPV23 alone. For this reason, the ACIP has recommended serial vaccination of the elderly with PCV13 and PPV23 since 2014 (Kobayashi et al. 2015). Therefore, new potential vaccines that effectively protect against pneumonia have been investigated (Table 2) and are undergoing clinical trials (Table 3).
Whole cell vaccine
Live attenuated vaccine
An attenuated or weakened form of the pathogen is used as a vaccine. Currently available live vaccines are the most cost effective (Minor 2015). In rare cases, the live attenuated vaccine strain can revert to its virulent wild type, causing severe disease (Pliaka et al. 2012). However, whole cell vaccines are superior to provide protection against various pneumococcal serotypes, as demonstrated by live attenuated mucosal vaccine (Wu et al. 2014; Roche et al. 2007; Kim et al. 2016).
Inactivated vaccine
The inactivated vaccine is made by treating pathogens with chemicals or physical processes. Compared to live attenuated vaccines, inactivated vaccines are safer (McConnell and Pachon 2010). Inactivated whole cell vaccine could confer effective protection against lethal pneumococcal challenge demonstrated by reduced colonization or higher survival rate (Choi et al. 2013; Moffitt et al. 2012; Hvalbye et al. 1999).
Subunit vaccine
Polysaccharide vaccine
The polysaccharide capsule from encapsulated bacteria is a major virulence factor and can be used as an antigen. However, the polysaccharide antigen interacts with B cells and directly induces antibody production without a T cell response (Goldblatt 2000; Song et al. 2013). Infants have a particularly immature B cell response, and so vaccines that do not also induce a T cell response cannot provide adequate protection against pneumococcal infection (Simon et al. 2015). The pneumococcal polysaccharide vaccine (PPV23; Pneumovax 23) comprises polysaccharide from 23 serotypes (1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19F, 19A, 20, 22F, 23F, and 33F), which are responsible for 85-90% of invasive pneumococcal infections in the world (WHO 2017c). PPV23 is effective against invasive pneumococcal disease (IPD), and is recommended to individuals aged ≥50 and children aged ≥2 (Fedson and Guppy 2013). However, PPV23 does not prevent the incidence of pneumonia or morbidity (Huss et al. 2009), since it elicits serum IgG but not secretory IgA in the nasopharynx. Although no strong evidence on PPV23-induced CAP prevention is available, PPV23 seems to alleviate CAP severity (Kraicer-Melamed et al. 2016; Johnstone et al. 2007).
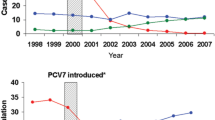
Conjugate vaccine
This vaccine uses polysaccharide antigens conjugated with carrier proteins (Goldblatt 2000). In contrast to polysaccharide vaccines, the conjugate vaccine can elicit T cell response, resulting in superior immunogenicity (Song et al. 2013) and immunity that lasts longer (Goldblatt 2000). Pneumococcal conjugate vaccine with 7 valent capsular polysaccharides (PCV7; Prevnar®) includes serotypes 4, 6B, 9V, 14, 18C, 19F and 23F, and PCV10 (Synflorix®) comprises serotypes 1, 4, 5, 6B, 7F, 9V, 14, 18C, 19F and 23F. Serotypes 3, 6A, and 19A were added to PCV13 (Prevnar 13®). PCV7 has been shown to induce protective effects against IPD, pneumonia, and otitis media (Lee et al. 2014; Pilishvili et al. 2010). Moreover, PCV7 could protect HIV-infected adults from pneumococcal infection (French et al. 2016). PCV13 markedly decreased pneumococcal pneumonia incidence in children because pneumococcal serotypes 19A and 3 are responsible for half of childhood pneumococcal pneumonia cases (Olarte et al. 2017). PCV13 vaccination is recommended for infants, children, and adults.
Protein based vaccine (Recombinant protein vaccine)
These vaccines consist of purified protein antigens that have been produced in bacteria (Nascimento and Leite 2012). The protein antigen elicits antibodies in a vaccinated person, thus protecting them from disease. Various recombinant protein vaccine was developed to elicit a sufficient protective immune response (Table 2).
Pneumococcal vaccine studies in the future
Respiratory pathogens initiate colonization in the mucosal surface to cause disease. Therefore, the mucosal immune system plays an important role as a primary physical barrier in protection against respiratory diseases (Neutra and Kozlowski 2006; Holmgren and Czerkinsky 2005). In the mucosal immune system, secretory IgA, a key factor in mucosal immunity, is induced by vaccination to entrap microbes or block microbial adherence and invasion (Lamm 1997; Hutchings et al. 2004). Local IgG is also induced (Kozlowski et al. 2002). Thus, mucosal vaccination induces both mucosal and systemic immune responses to provide effective protection against respiratory diseases such as pneumonia. Compared with mucosal vaccines, injectable vaccines are less effective at generating mucosal immune responses (Lamm 1997), and could transmit infection via the blood through contaminated needles (Levine and Dougan 1998). Despite the mucosal vaccine’s advantages, and their use against diseases such as cholera, polio and influenza, few of these vaccines are available (Holmgren and Czerkinsky 2005). This is because the mucosal immune system reacts to mucosal vaccines as they do for microorganisms, making their implementation difficult; i.e., the mucosal vaccine adheres to the mucosal surface and is subject to degradation by proteases and nucleases, triggering the same immune response as the real pathogen. Thus, to be feasible, mucosal vaccines must overcome this hurdle, and evoke secretory immune responses, such as secretory IgA.
Conclusion
The most common pneumonia, CAP, is mainly caused by S. pneumoniae. Although antibiotics have been used to treat pneumonia, the incidence of antibiotic resistance has increased and the risk of pneumonia in children and the elderly with weak immune responses is high. Thus, to prevent pneumonia or IPD, including sepsis, the WHO and ACIP recommend vaccination. Moreover, influenza virus, a critical factor in increased pneumococcal pneumonia risk, has been linked to higher mortality. After the introduction of PCV vaccination, the incidence of pneumonia and IPD greatly decreased. However, the current vaccine cannot prevent emergence of pneumococcal diseases caused by serotypes not included in the vaccine. Thus, development of new mucosal vaccine types is needed to protect against a broader range of serotypes.
References
Andre G, Converso TR, Politano WR, Ferraz LF, Ribeiro ML, Leite LC, Darrieux M (2017) Role of Streptococcus pneumoniae proteins in evasion of complement-mediated immunity. Front Microbiol 8:224
Bewick T, Sheppard C, Greenwood S, Slack M, Trotter C, George R, Lim WS (2012) Serotype prevalence in adults hospitalised with pneumococcal non-invasive community-acquired pneumonia. Thorax 67:540–545
Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Jha P, Campbell H, Walker CF, Cibulskis R, Eisele T, Liu L, Mathers C (2010) Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375:1969–1987
Bogaert D, De Groot R, Hermans PW (2004) Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis 4:144–154
Briles DE, King JD, Gray MA, Mcdaniel LS, Swiatlo E, Benton KA (1996) PspA, a protection-eliciting pneumococcal protein: immunogenicity of isolated native PspA in mice. Vaccine 14:858–867
Briles DE, Hollingshead SK, King J, Swift A, Braun PA, Park MK, Ferguson LM, Nahm MH, Nabors GS (2000) Immunization of humans with recombinant pneumococcal surface protein A (rPspA) elicits antibodies that passively protect mice from fatal infection with Streptococcus pneumoniae bearing heterologous PspA. J Infect Dis 182:1694–1701
Briles DE, Hollingshead SK, Paton JC, Ades EW, Novak L, Van Ginkel FW, Benjamin WH Jr (2003) Immunizations with pneumococcal surface protein A and pneumolysin are protective against pneumonia in a murine model of pulmonary infection with Streptococcus pneumoniae. J Infect Dis 188:339–348
Carvalho RP, Mesquita JS, Bonomo A, Elsas PX, Colombo AP (2009) Relationship of neutrophil phagocytosis and oxidative burst with the subgingival microbiota of generalized aggressive periodontitis. Oral Microbiol Immunol 24:124–132
CDC Symptoms and Complications (2017) Centers for Disease Control and Prevetion https://www.cdc.gov/pneumococcal/about/symptoms-complications.html. Accessed 10 Mar 2017
Choi SY, Tran TD, Briles DE, Rhee DK (2013) Inactivated pep27 mutant as an effective mucosal vaccine against a secondary lethal pneumococcal challenge in mice. Clin Exp Vaccine Res 2:58–65
Croucher NJ, Finkelstein JA, Pelton SI, Mitchell PK, Lee GM, Parkhill J, Bentley SD, Hanage WP, Lipsitch M (2013) Population genomics of post-vaccine changes in pneumococcal epidemiology. Nat Genet 45:656–663
Daniels CC, Coan P, King J, Hale J, Benton KA, Briles DE, Hollingshead SK (2010) The proline-rich region of pneumococcal surface proteins A and C contains surface-accessible epitopes common to all pneumococci and elicits antibody-mediated protection against sepsis. Infect Immun 78:2163–2172
ERS The burden of lung disease. European respiratory society (2017) http://www.erswhitebook.org/chapters/the-burden-of-lung-disease/. Accessed 12 Mar 2017
Fedson DS, Guppy MJ (2013) Pneumococcal vaccination of older adults: conjugate or polysaccharide? Hum Vaccin Immunother 9:1382–1384
Flannery B, Heffernan RT, Harrison LH, Ray SM, Reingold AL, Hadler J, Schaffner W, Lynfield R, Thomas AR, Li J, Campsmith M, Whitney CG, Schuchat A (2006) Changes in invasive Pneumococcal disease among HIV-infected adults living in the era of childhood pneumococcal immunization. Ann Intern Med 144:1–9
Flasche S, Van Hoek AJ, Sheasby E, Waight P, Andrews N, Sheppard C, George R, Miller E (2011) Effect of pneumococcal conjugate vaccination on serotype-specific carriage and invasive disease in England: a cross-sectional study. PLoS Med 8:e1001017
French N, Gordon SB, Mwalukomo T, White SA, Mwafulirwa G, Longwe H, Mwaiponya M, Zijlstra EE, Molyneux ME, Gilks CF (2016) A trial of a 7-valent pneumococcal conjugate vaccine in HIV-infected adults. Malawi Med J 28:115–122
Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ (2005) Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA 294:2712–2719
Gadsby NJ, Russell CD, Mchugh MP, Mark H, Conway Morris A, Laurenson IF, Hill AT, Templeton KE (2016) Comprehensive molecular testing for respiratory pathogens in community-acquired pneumonia. Clin Infect Dis 62:817–823
Giefing C, Meinke AL, Hanner M, Henics T, Bui MD, Gelbmann D, Lundberg U, Senn BM, Schunn M, Habel A, Henriques-Normark B, Ortqvist A, Kalin M, Von Gabain A, Nagy E (2008) Discovery of a novel class of highly conserved vaccine antigens using genomic scale antigenic fingerprinting of pneumococcus with human antibodies. J Exp Med 205:117–131
Glover DT, Hollingshead SK, Briles DE (2008) Streptococcus pneumoniae surface protein PcpA elicits protection against lung infection and fatal sepsis. Infect Immun 76:2767–2776
Goldblatt D (2000) Conjugate vaccines. Clin Exp Immunol 119:1–3
Hayward S, Thompson LA, Mceachern A (2016) Is 13-valent pneumococcal conjugate vaccine (PCV13) combined with 23-valent pneumococcal polysaccharide vaccine (PPSV23) superior to PPSV23 alone for reducing incidence or severity of pneumonia in older adults? A Clin-IQ. J Patient Cent Res Rev 3:111–115
Hirst RA, Kadioglu A, O’Callaghan C, Andrew PW (2004) The role of pneumolysin in pneumococcal pneumonia and meningitis. Clin Exp Immunol 138:195–201
Holmgren J, Czerkinsky C (2005) Mucosal immunity and vaccines. Nat Med 11:S45–S53
Huss A, Scott P, Stuck AE, Trotter C, Egger M (2009) Efficacy of pneumococcal vaccination in adults: a meta-analysis. CMAJ 180:48–58
Hutchings AB, Helander A, Silvey KJ, Chandran K, Lucas WT, Nibert ML, Neutra MR (2004) Secretory immunoglobulin A antibodies against the sigma1 outer capsid protein of reovirus type 1 Lang prevent infection of mouse Peyer’s patches. J Virol 78:947–957
Hvalbye BK, Aaberge IS, Lovik M, Haneberg B (1999) Intranasal immunization with heat-inactivated Streptococcus pneumoniae protects mice against systemic pneumococcal infection. Infect Immun 67:4320–4325
Jackson ML, Neuzil KM, Thompson WW, Shay DK, Yu O, Hanson CA, Jackson LA (2004) The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis 39:1642–1650
Jain S, Self WH, Wunderink RG, Fakhran S, Balk R, Bramley AM, Reed C, Grijalva CG, Anderson EJ, Courtney DM, Chappell JD, Qi C, Hart EM, Carroll F, Trabue C, Donnelly HK, Williams DJ, Zhu Y, Arnold SR, Ampofo K, Waterer GW, Levine M, Lindstrom S, Winchell JM, Katz JM, Erdman D, Schneider E, Hicks LA, Mccullers JA, Pavia AT, Edwards KM, Finelli L (2015) Community-acquired pneumonia requiring hospitalization among U.S. Adults N Engl J Med 373:415–427
Johnstone J, Marrie TJ, Eurich DT, Majumdar SR (2007) Effect of pneumococcal vaccination in hospitalized adults with community-acquired pneumonia. Arch Intern Med 167:1938–1943
Johnstone J, Majumdar SR, Fox JD, Marrie TJ (2008) Viral infection in adults hospitalized with community-acquired pneumonia: prevalence, pathogens, and presentation. Chest 134:1141–1148
Kadioglu A, Weiser JN, Paton JC, Andrew PW (2008) The role of Streptococcus pneumoniae virulence factors in host respiratory colonization and disease. Nat Rev Microbiol 6:288–301
Kalin M (1998) Pneumococcal serotypes and their clinical relevance. Thorax 53:159–162
Kapatai G, Sheppard CL, Al-Shahib A, Litt DJ, Underwood AP, Harrison TG, Fry NK (2016) Whole genome sequencing of Streptococcus pneumoniae: development, evaluation and verification of targets for serogroup and serotype prediction using an automated pipeline. PeerJ 4:e2477
Kaplan SL, Mason EO Jr (1998) Management of infections due to antibiotic-resistant Streptococcus pneumoniae. Clin Microbiol Rev 11:628–644
Kim EH, Choi SY, Kwon MK, Tran TD, Park SS, Lee KJ, Bae SM, Briles DE, Rhee DK (2012) Streptococcus pneumoniae pep27 mutant as a live vaccine for serotype-independent protection in mice. Vaccine 30:2008–2019
Kim GL, Choi SY, Seon SH, Lee S, Park SS, Song JY, Briles DE, Rhee DK (2016) Pneumococcal pep27 mutant immunization stimulates cytokine secretion and confers long-term immunity with a wide range of protection, including against non-typeable strains. Vaccine 34:6481–6492
Kim DK, Riley LE, Harriman KH, Hunter P, Bridges CB (2017) Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older—United States, 2017. MMWR Morb Mortal Wkly Rep 66:136–138
Kobayashi M, Bennett NM, Gierke R, Almendares O, Moore MR, Whitney CG, Pilishvili T (2015) Intervals Between PCV13 and PPSV23 Vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 64:944–947
Kong IG, Sato A, Yuki Y, Nochi T, Takahashi H, Sawada S, Mejima M, Kurokawa S, Okada K, Sato S, Briles DE, Kunisawa J, Inoue Y, Yamamoto M, Akiyoshi K, Kiyono H (2013) Nanogel-based PspA intranasal vaccine prevents invasive disease and nasal colonization by Streptococcus pneumoniae. Infect Immun 81:1625–1634
Korsgaard J, Moller JK, Kilian M (2005) Antibiotic treatment and the diagnosis of Streptococcus pneumoniae in lower respiratory tract infections in adults. Int J Infect Dis 9:274–279
Kozlowski PA, Williams SB, Lynch RM, Flanigan TP, Patterson RR, Cu-Uvin S, Neutra MR (2002) Differential induction of mucosal and systemic antibody responses in women after nasal, rectal, or vaginal immunization: influence of the menstrual cycle. J Immunol 169:566–574
Kraicer-Melamed H, O’donnell S, Quach C (2016) The effectiveness of pneumococcal polysaccharide vaccine 23 (PPV23) in the general population of 50 years of age and older: a systematic review and meta-analysis. Vaccine 34:1540–1550
KSID (2014) Recommended immunization schedule for adults in Korea, by the Korean Society of Infectious Diseases, 2012. Clin Exp Vaccine Res 3:110–112
Lamm ME (1997) Interaction of antigens and antibodies at mucosal surfaces. Annu Rev Microbiol 51:311–340
Lee H, Choi EH, Lee HJ (2014) Efficacy and effectiveness of extended-valency pneumococcal conjugate vaccines. Korean J Pediatr 57:55–66
Levine MM, Dougan G (1998) Optimism over vaccines administered via mucosal surfaces. Lancet 351:1375–1376
Lu YJ, Forte S, Thompson CM, Anderson PW, Malley R (2009) Protection against Pneumococcal colonization and fatal pneumonia by a trivalent conjugate of a fusion protein with the cell wall polysaccharide. Infect Immun 77:2076–2083
Lu YJ, Leite L, Goncalves VM, Dias Wde O, Liberman C, Fratelli F, Alderson M, Tate A, Maisonneuve JF, Robertson G, Graca R, Sayeed S, Thompson CM, Anderson P, Malley R (2010) GMP-grade pneumococcal whole-cell vaccine injected subcutaneously protects mice from nasopharyngeal colonization and fatal aspiration-sepsis. Vaccine 28:7468–7475
Lynch JP, Zhanel GG (2009) Streptococcus pneumoniae: epidemiology, risk factors, and strategies for prevention. Semin Respir Crit Care Med 30:189–209
Mayoclinic Symptoms and causes, Pneumonia. Mayo Clinic (2017) http://www.mayoclinic.org/diseases-conditions/pneumonia/symptoms-causes/dxc-20204678. Accessed 21 June 2017
Mcconnell MJ, Pachon J (2010) Active and passive immunization against Acinetobacter baumannii using an inactivated whole cell vaccine. Vaccine 29:1–5
Metzger DW, Furuya Y, Salmon SL, Roberts S, Sun K (2015) Limited efficacy of antibacterial vaccination against secondary serotype 3 pneumococcal pneumonia following influenza infection. J Infect Dis 212:445–452
Michelow IC, Olsen K, Lozano J, Rollins NK, Duffy LB, Ziegler T, Kauppila J, Leinonen M, Mccracken GH (2004) Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children. Pediatrics 113:701–707
Mina MJ, Klugman KP (2013) Pathogen replication, host inflammation, and disease in the upper respiratory tract. Infect Immun 81:625–628
Minor PD (2015) Live attenuated vaccines: historical successes and current challenges. Virology 479–480:379–392
Moffitt KL, Yadav P, Weinberger DM, Anderson PW, Malley R (2012) Broad antibody and T cell reactivity induced by a pneumococcal whole-cell vaccine. Vaccine 30:4316–4322
Monsalvo AC, Batalle JP, Lopez MF, Krause JC, Klemenc J, Hernandez JZ, Maskin B, Bugna J, Rubinstein C, Aguilar L, Dalurzo L, Libster R, Savy V, Baumeister E, Aguilar L, Cabral G, Font J, Solari L, Weller KP, Johnson J, Echavarria M, Edwards KM, Chappell JD, Crowe JE, Williams JV, Melendi GA, Polack FP (2011) Severe pandemic 2009 H1N1 influenza disease due to pathogenic immune complexes. Nat Med 17:U195–U225
Musher DM (2016) Editorial commentary: quantitative molecular approach to diagnosing pneumonia. Clin Infect Dis 62:824–825
Musher DM, Thorner AR (2014) Community-acquired pneumonia. N Engl J Med 371:1619–1628
Nascimento IP, Leite LC (2012) Recombinant vaccines and the development of new vaccine strategies. Braz J Med Biol Res 45:1102–1111
Neutra MR, Kozlowski PA (2006) Mucosal vaccines: the promise and the challenge. Nat Rev Immunol 6:148–158
Nguyen CT, Kim SY, Kim MS, Lee SE, Rhee JH (2011) Intranasal immunization with recombinant PspA fused with a flagellin enhances cross-protective immunity against Streptococcus pneumoniae infection in mice. Vaccine 29:5731–5739
Ogunniyi AD, Woodrow MC, Poolman JT, Paton JC (2001) Protection against Streptococcus pneumoniae elicited by immunization with pneumolysin and CbpA. Infect Immun 69:5997–6003
Olafsdottir TA, Lingnau K, Nagy E, Jonsdottir I (2012) Novel protein-based pneumococcal vaccines administered with the Th1-promoting adjuvant IC31 induce protective immunity against pneumococcal disease in neonatal mice. Infect Immun 80:461–468
Olarte L, Barson WJ, Barson RM, Romero JR, Bradley JS, Tan TQ, Givner LB, Hoffman JA, Lin PL, Hulten KG, Mason EO, Kaplan SL (2017) Pneumococcal Pneumonia Requiring Hospitalization in U.S. Children in the 13-Valent Pneumococcal Conjugate Vaccine Era. Clin Infect Dis 64(12):1699–1704
Pavia AT (2013) What is the role of respiratory viruses in community-acquired pneumonia?: what is the best therapy for influenza and other viral causes of community-acquired pneumonia? Infect Dis Clin North Am 27:157–175
Picazo JJ (2009) Management of antibiotic-resistant Streptococcus pneumoniae infections and the use of pneumococcal conjugate vaccines. Clin Microbiol Infect 15(Suppl 3):4–6
Pilishvili T, Lexau C, Farley MM, Hadler J, Harrison LH, Bennett NM, Reingold A, Thomas A, Schaffner W, Craig AS, Smith PJ, Beall BW, Whitney CG, Moore MR (2010) Sustained reductions in invasive pneumococcal disease in the era of conjugate vaccine. J Infect Dis 201:32–41
Pliaka V, Kyriakopoulou Z, Markoulatos P (2012) Risks associated with the use of live-attenuated vaccine poliovirus strains and the strategies for control and eradication of paralytic poliomyelitis. Expert Rev Vaccines 11:609–628
Restrepo MI, Mortensen EM, Velez JA, Frei C, Anzueto A (2008) A comparative study of community-acquired pneumonia patients admitted to the ward and the ICU. Chest 133:610–617
Robinson CL, Romero JR, Kempe A, Pellegrini C (2017) Advisory committee on immunization practices recommended immunization schedule for children and adolescents aged 18 years or younger—United States, 2017. MMWR Morb Mortal Wkly Rep 66:134–135
Roche AM, King SJ, Weiser JN (2007) Live attenuated Streptococcus pneumoniae strains induce serotype-independent mucosal and systemic protection in mice. Infect Immun 75:2469–2475
Sheng ZM, Chertow DS, Ambroggio X, Mccall S, Przygodzki RM, Cunningham RE, Maximova OA, Kash JC, Morens DM, Taubenberger JK (2011) Autopsy series of 68 cases dying before and during the 1918 influenza pandemic peak. Proc Natl Acad Sci USA 108:16416–16421
Simon AK, Hollander GA, Mcmichael A (2015) Evolution of the immune system in humans from infancy to old age. Proc Biol Sci 282:20143085
Song JY, Nahm MH, Moseley MA (2013) Clinical implications of pneumococcal serotypes: invasive disease potential, clinical presentations, and antibiotic resistance. J Korean Med Sci 28:4–15
Steel HC, Cockeran R, Anderson R, Feldman C (2013) Overview of community-acquired pneumonia and the role of inflammatory mechanisms in the immunopathogenesis of severe pneumococcal disease. Mediat Inflamm 2013:490346
Van Der Poll T, Opal SM (2009) Pathogenesis, treatment, and prevention of pneumococcal pneumonia. Lancet 374:1543–1556
Verhoeven D, Xu Q, Pichichero ME (2014) Vaccination with a Streptococcus pneumoniae trivalent recombinant PcpA, PhtD and PlyD1 protein vaccine candidate protects against lethal pneumonia in an infant murine model. Vaccine 32:3205–3210
Vila-Corcoles A, Ochoa-Gondar O (2013) Preventing pneumococcal disease in the elderly: recent advances in vaccines and implications for clinical practice. Drugs Aging 30:263–276
WHO the top 10 causes of death, 2015 (2017a) World Health Organization. http://www.who.int/mediacentre/factsheets/fs310/en/index1.html. Accessed 12 Mar 2017
WHO causes of child mortality, 2015 (2017b) Global Health Observatory data World Health Organization. http://www.who.int/gho/child_health/mortality/causes/en/. Accessed 12 Mar 2017
WHO pneumococcal disease (2017c) World Health Organization. http://www.who.int/ith/vaccines/pneumococcal/en/. Accessed 12 Mar 2017
Wu K, Yao R, Wang H, Pang D, Liu Y, Xu H, Zhang S, Zhang X, Yin Y (2014) Mucosal and systemic immunization with a novel attenuated pneumococcal vaccine candidate confer serotype independent protection against Streptococcus pneumoniae in mice. Vaccine 32:4179–4188
Wunderink RG, Waterer GW (2014) Community-acquired pneumonia. N Engl J Med 370:1863
Acknowledgement
This work was supported by the National Research Foundation (NRF-2015R1 A2 A1 A10052511).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, GL., Seon, SH. & Rhee, DK. Pneumonia and Streptococcus pneumoniae vaccine. Arch. Pharm. Res. 40, 885–893 (2017). https://doi.org/10.1007/s12272-017-0933-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-017-0933-y