Abstract
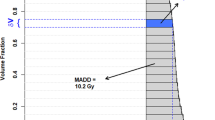
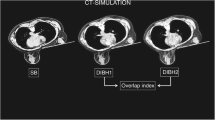
To analyze respiratory motion of surgical clips, chest wall (CW) and the anterior displacement of the heart and its impact on heart dosimetry between prone (Pr) and supine (Su) positions during whole breast radiotherapy after breast conserving surgery. Sixteen patients underwent 4D-CT for radiotherapy planning in Pr and Su positions. Maximum inhale and maximum exhale phases were analyzed. Mean 3D vectorial displacements ± standard deviations (SD) of the surgical clips were measured. Volumetric changes of the CW were recorded and compared. Cardiac displacement was assessed by a volume between the inner surface of CW and the myocardium of the heart (CW/H-V). For left-sided cases, comparative dosimetry was performed in each position simulating no- (Pr-noC, Su-noC) versus daily correction protocols (Pr-C, Su-C). The movements of 81 surgical clips were analyzed. Prone positioning significantly reduced both the mean 3D vectorial displacements (1.1 ± 0.6 (Pr) vs. 2.0 ± 0.9 mm (Su), p < 0.01) and their variability (0.3 ± 0.2 vs. 0.5 ± 0.3 mm, p = 0.01). Respiration-induced volumetric changes of CW were also significantly lower in Pr (2.3 ± 4.9 vs. 9.6 ± 7.1 cm3 , p < 0.01). The CW/H-V was significantly smaller in Pr than in Su (39.9 ± 14.6 vs. 64.3 ± 28.2 cm3 , p < 0.01). Besides identical target coverage heart, left-anterior-descending coronary artery (LADCA) and ipsilateral lung dose parameters were lowered with Pr-C compared to Pr-noC, Su-C and Su-noC. Prone position significantly reduced respiration-related surgical clip movements, their variability as well as CW movements. Significant anterior heart displacement was observed in Pr. Prone position with daily online correction could maximize the heart and LADCA protection.




Similar content being viewed by others
References
Darby S, McGale P, Correa C, Taylor C, Arriagada R, Clarke M et al (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378:1707–1716. doi:10.1016/S0140-6736(11)61629-2
Kovacs A, Lakosi F, Liposits G, Toller G, Hadjiev J, Vandulek C et al (2011) 3-D conformal photon boost in the treatment of early stage breast cancer: 4 years follow up results. Pathol Oncol Res 17:17–23. doi:10.1007/s12253-010-9264-8
Haviland JS, Owen JR, Dewar JA, Agrawal RK, Barrett J, Barrett-Lee PJ et al (2013) The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. Lancet Oncol 14:1086–1094. doi:10.1016/S1470-2045(13)70386-3
Polgár C, Van Limbergen E, Pötter R, Kovács G, Polo A, Lyczek J et al (2010) Patient selection for accelerated partial-breast irradiation (APBI) after breast-conserving surgery: recommendations of the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) breast cancer working group ba. Radiother Oncol 94:264–273. doi:10.1016/j.radonc.2010.01.014
Smith BD, Arthur DW, Buchholz TA, Haffty BG, Hahn CA, Hardenbergh PH et al (2009) Accelerated partial breast irradiation consensus statement from the American Society for Radiation Oncology (ASTRO). Int J Radiat Oncol Biol Phys 74:987–1001. doi:10.1016/j.ijrobp.2009.02.031
Whelan TJ, Pignol J-P, Levine MN, Julian JA, MacKenzie R, Parpia S et al (2010) Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med 362:513–520. doi:10.1056/NEJMoa0906260
Freedman GM, White JR, Arthur DW, Allen Li X, Vicini FA (2013) Accelerated fractionation with a concurrent boost for early stage breast cancer. Radiother Oncol 106:15–20. doi:10.1016/j.radonc.2012.12.001
Freedman GM, White JR, Arthur DW, Allen Li X, Vicini FA (2013) Accelerated fractionation with a concurrent boost for early stage breast cancer. Radiother Oncol 106:15–20. doi:10.1016/j.radonc.2012.12.001
Kim LH, Goyal S, Haffty BG, Taunk NK, Yue NJ (2012) Using respiratory motion to guide planning target volume margins for external beam partial breast irradiation. Int J Radiat Oncol Biol Phys 82:1303–1306. doi:10.1016/j.ijrobp.2011.11.048
Kirby AM, Evans PM, Donovan EM, Convery HM, Haviland JS, Yarnold JR (2010) Prone versus supine positioning for whole and partial-breast radiotherapy: a comparison of non-target tissue dosimetry. Radiother Oncol 96:178–184. doi:10.1016/j.radonc.2010.05.014
Kirby AM, Evans PM, Helyer SJ, Donovan EM, Convery HM, Yarnold JR (2011) A randomised trial of supine versus prone breast radiotherapy (SuPr study): comparing set-up errors and respiratory motion. Radiother Oncol 100:221–226. doi:10.1016/j.radonc.2010.11.005
Krengli M, Masini L, Caltavuturo T, Pisani C, Apicella G, Negri E et al (2013) Prone versus supine position for adjuvant breast radiotherapy: a prospective study in patients with pendulous breasts. Radiat Oncol 8:232. doi:10.1186/1748-717X-8-232
Lymberis SC, de Wyngaert JK, Parhar P, Chhabra AM, Fenton-Kerimian M, Chang J et al (2012) Prospective assessment of optimal individual position (prone versus supine) for breast radiotherapy: volumetric and dosimetric correlations in 100 patients. Int J Radiat Oncol Biol Phys 84:902–909. doi:10.1016/j.ijrobp.2012.01.040
Mitchell J, Formenti SC, DeWyngaert JK (2010) Interfraction and intrafraction setup variability for prone breast radiation therapy. Int J Radiat Oncol Biol Phys 76:1571–1577. doi:10.1016/j.ijrobp.2009.07.1683
Morrow NV, Stepaniak C, White J, Wilson JF, Li XA (2007) Intra- and interfractional variations for prone breast irradiation: an indication for image-guided radiotherapy. Int J Radiat Oncol Biol Phys 69:910–917. doi:10.1016/j.ijrobp.2007.06.056
Mulliez T, Veldeman L, van Greveling A, Speleers B, Sadeghi S, Berwouts D et al (2013) Hypofractionated whole breast irradiation for patients with large breasts: a randomized trial comparing prone and supine positions. Radiother Oncol 108:203–208. doi:10.1016/j.radonc.2013.08.040
Nissen HD, Appelt AL (2013) Improved heart, lung and target dose with deep inspiration breath hold in a large clinical series of breast cancer patients. Radiother Oncol 106:28–32. doi:10.1016/j.radonc.2012.10.016
Veldeman L, De Gersem W, Speleers B, Truyens B, Van Greveling A, Van den Broecke R et al (2012) Alternated prone and supine whole-breast irradiation using IMRT: setup precision, respiratory movement and treatment time. Int J Radiat Oncol Biol Phys 82:2055–2064. doi:10.1016/j.ijrobp.2010.10.070
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Brønnum D et al (2013) Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 368:987–998. doi:10.1056/NEJMoa1209825
Würschmidt F, Stoltenberg S, Kretschmer M, Petersen C (2014) Incidental dose to coronary arteries is higher in prone than in supine whole breast irradiation. A dosimetric comparison in adjuvant radiotherapy of early stage breast cancer. Strahlenther Onkol 190:563–568. doi:10.1007/s00066-014-0606-4
Chino JP, Marks LB (2008) Prone positioning causes the heart to be displaced anteriorly within the thorax: implications for breast cancer treatment. Int J Radiat Oncol Biol Phys 70:916–920. doi:10.1016/j.ijrobp.2007.11.001
Z. Varga, A. Cserháti, F. Rárosi, K. Boda, G. Gulyás, Z. Együd, et al (2013) Individualized positioning for maximum heart protection during breast irradiation. Acta Oncol. 1–7. doi:10.3109/0284186X.2013.781674
van Herk M, Remeijer P, Rasch C, Lebesque JV (2000) The probability of correct target dosage: dose-population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys 47:1121–1135
Feng M, Moran JM, Koelling T, Chughtai A, Chan JL, Freedman L et al (2011) Development and validation of a heart atlas to study cardiac exposure to radiation following treatment for breast cancer. Int J Radiat Oncol Biol Phys 79:10–18. doi:10.1016/j.ijrobp.2009.10.058
Gulyban A, Kovács P, Sebestyén Z, Farkas R, Csere T, Karácsonyi G et al (2008) Multisegmented tangential breast fields: a rational way to treat breast cancer. Strahlenther Onkol 184:262–269. doi:10.1007/s00066-008-1770-1
Price GJ, Sharrock PJ, Marchant TE, Parkhurst JM, Burton D, Jain P et al (2009) An analysis of breast motion using high-frequency, dense surface points captured by an optical sensor during radiotherapy treatment delivery. Phys Med Biol 54:6515–6533. doi:10.1088/0031-9155/54/21/005
Kim LH, Goyal S, Haffty BG, Taunk NK, Yue NJ (2012) Using respiratory motion to guide planning target volume margins for external beam partial breast irradiation. Int J Radiat Oncol Biol Phys 82:1303–1306. doi:10.1016/j.ijrobp.2011.11.048
Price GJ, Sharrock PJ, Marchant TE, Parkhurst JM, Burton D, Jain P et al (2009) An analysis of breast motion using high-frequency, dense surface points captured by an optical sensor during radiotherapy treatment delivery. Phys Med Biol 54:6515–6533. doi:10.1088/0031-9155/54/21/005
Lakosi F, Ben Mustapha S, Gulyban A, Cucchiaro S, Ernst C, Martin N et al (2014) Hypofractionated whole prone breast RT using Sagittilt system: patient comfort, setup accuracy and acute toxicity. Radiat Oncol ESTRO 33:EP–1204
Chino JP, Marks LB (2008) Prone positioning causes the heart to be displaced anteriorly within the thorax: implications for breast cancer treatment. Int J Radiat Oncol Biol Phys 70:916–920. doi:10.1016/j.ijrobp.2007.11.001
Hall EJ, Wuu C-S (2003) Radiation-induced second cancers: the impact of 3D-CRT and IMRT. Int J Radiat Oncol 56:83–88. doi:10.1016/S0360-3016(03)00073-7
de Puysseleyr A, Mulliez T, Gulyban A, Bogaert E, Vercauteren T, Van Hoof T et al (2013) Improved cone-beam computed tomography in supine and prone breast radiotherapy. Surface reconstruction, radiation exposure, and clinical workflow., Strahlenther. Onkol 189:945–950. doi:10.1007/s00066-013-0435-x
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lakosi, F., Gulyban, A., Janvary, L. et al. Respiratory Motion, Anterior Heart Displacement and Heart Dosimetry: Comparison Between Prone (Pr) and Supine (Su) Whole Breast Irradiation. Pathol. Oncol. Res. 21, 1051–1058 (2015). https://doi.org/10.1007/s12253-015-9932-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-015-9932-9