Abstract
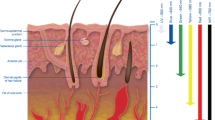
The thermal wave and the Pennes bioheat transfer models are solved analytically by employing the Laplace transform method for small and large values of reflection power (albedo) during laser irradiation. Most of the previous studies have been based on the infinite heat diffusion velocity, but non-Fourier thermal behavior has been observed experimentally in biological tissue. At low initial albedo values, the temperature in the skin depth that directly results from conduction heat transfer process is caused by the lengthy thermal relaxation time in skin tissue. This condition generates a big difference between the thermal wave and Pennes results at the beginning of the heating process. This difference increases under short-time heating condition and high heat flux. However, with high initial albedo, the temperature distribution in the skin depth becomes negligible because of the skin absorption of laser beams. The non-Fourier effect should be considered during laser heating with low albedo, because errors in the predicted temperature values may occur.
Similar content being viewed by others
Reference
S. L. Jacques, Laser-tissue interactions: photochemical, photothermal, and photomechanical, Surg. Clin. N. Am., 72 (1992) 531–558.
S. L. Jaques, How tissue optics affect dosimetry for photochemical photothermal and photomechanical mechanisms of laser-tissue interaction, Proc. SPIE (1991) 316–322.
M. Panjehpour, A. Wilke, D. L. Frazier and B. F. Overholt, Hyperthermia treatment using a computer controlled Nd:YAG laser system in combination with surface cooling, Proc SPIE (1991) 307–315.
P. Svensson, P. Bjerring, L. Arendtnielsen, J. C. Nielsen and S. Kaaber, Comparison of four laser type for experimental pain stimulation on oral-mucosa and hairy skin, Lasers Surg Med, 11(4) (1991) 313–324.
S. W. Derbyshire, A. K. Jones, F. Gyulai, S. Clark, D. Towsend and L. Firestone, Pain processing of three levels of noxious stimulation produces differential patterns of central activity, Pain, 73 (1997) 431–445.
A. C. Chen, Human brain measures of clinical pain: a review I. Topographic mappings, Pain, 54 (1993) 115–132.
U. Bingel, M. Quante, R. Knab, B. Bromm, C. Weiller and C. Buchel, Subcortical structures involved in pain evidence from single-trial Fmri, Pain, 99 (2002) 313–321.
R. Biehl, R. D. Treede and B. Bromm, Pain ratings and short radiant heat pulses. In: Bromm B (ed) Pain measurement in man: neurophysiological correlates of pain, Elsevier, Amsterdam (1984) 397–408.
M. Jaunich, S. Raje, K. Kim, K. Mitra and Z. Guo, Bio-heat transfer analysis during short pulse laser irradiation of tissues, Int. J. Heat Mass Transfer, 51 (2008) 5511–5521.
C. C. Katsidis, A simple model for the analysis of light absorption and temperature rise in human skin: the role of surface roughness, Department of Applied Informatics and Multimedia, A.T.E.I of Crete, Heraklion, Greece, 2002.
J. Molina, M. Rivera and M. Trujillo, Assessment of hyperbolic heat transfer equation in theoretical modeling for radiofrequency heating techniques, The open Biomedical engineering journal, 2 (2008) 22–27.
K. W. Guan, Y. Q. Jiang, C. S. Sun and H. Yu, A two-layer model of laser interaction with skin: A photothermal effect analysis, Optics & Laser Technology, 43 (2011) 425–429.
J. Z. Zhang, Y. G. Shen and X. X. Zhang, A dynamic photo-thermal model of carbon dioxide laser tissue ablation, Lasers Med Sci (2009) 24:329–338.
A. Sakurai, I. Nitta, S. Maruyama, J. Okajima and K. Matsubara, Coupled photon and heat transport simulation inside biological tissue for laser therapy, J. Thermal Science and Technology, 4(2) (2009) 314–323.
J. M. Amado, M. J. Tobar, A. Ramil and A. Yanez, Application of the Laplace transform Dual reciprocity boundary element method in the modeling of laser heat treatments, Engineering Analysis with Boundary Elements, 29 (2005) 126–135.
J. Zhou, J. K. Chen and Y. Zhang, Dual-phase-lag effects on thermal damage to biological tissues cause by laser irradiation, Computer in Biology and Medicine, 39 (2009) 286–293.
J. Zhou, Y. Zhang and J. K. Chen, An axisymmetric dualphase-lag bioheat model for laser heating of living tissues, Int. J. Thermal science, 48 (2009) 1477–1485.
D. Y. Tzou, A unified field approach for heat conduction from macro- to microscales, ASME Journal of Heat Transfer, 117 (1995) 8–16.
K. Kim and Z. Guo, Multi-time-scale heat transfer modeling of turbid tissues exposed to short-pulsed irradiations, Comp. Meth. Prog. Biomed., 86 (2007) 112–123.
J. Jiao and Z. Guo, Thermal interaction of short-pulsed laser focused beams with skin tissues, Phys. Med. Biol., 54 (2009) 4225–4241.
A. Banerjee, A. A. Ogale, C. Das, K. Mitra and C. Subramanian, Temperature distribution in different materials due to short pulse laser irradiation, Heat Transfer Engineering, 26(8) (2005) 41–49.
S. Özen, S. Helhel and S. Bilgin, Temperature and burn injury prediction of human skin exposed to microwaves: a model analysis, Radiation and Environmental Biophysics, 50(3) (2011) 483–489.
Ş. Özen, S. Helhel and O. Çerezci, Heat analysis of biological tissue exposed to microwave by using thermal wave model of bio-heat transfer, Burns, 34(1) (2008) 45–49.
K. C. Liu, P. J. Cheng and Y. N. Wang, Analysis of non-Fourier thermal behaviour for multi-layer skin model, Thermal Science, 15 (2011) S61–S67.
K. R. Foster, H. Zhang and J. M. Osepchuk, Thermal response of tissue to millimeter waves: implications for setting exposure guidelines, Health Physics, 99(6) (2010) 806–810.
R. Waynant, Lasers in medicine, CRC press LLC, (2002).
C. Raulin and S. Karsai, Laser and ILP technology in dermatology and aesthetic medicine, Springer-Verlag Berlin Heidelberg (2011).
T. Vo-Dinh, Biomedical photonics handbook, CRC press LLC (2003).
S. A. Prahl, I. A. Vitkin, U. Bruggemann and B. C. Wilson, Determination of optical properties of turbid media using pulsed photothermal radiometry, Phys. Med. Biol., 37 (1992) 1203–1217.
A. J. Welch and M. J. C. van Gemert, Optical-thermal response of laser-irradiated tissue, Springer Science and Business Media B.V. (2011).
T. J. Farrell, M. S. Patterson and B. C. Wilson, A diffusion theory model of spatially resolved, steady-state diffuse reluctance for the non-invasive determination of tissue optical properties in vivo. Med. Phys., 19 (1992) 879–888.
H. H. Pennes, Analysis of tissue and arterial blood temperature in the resting forearm, J. Appl. Physiol., 1 (1948) 93–122.
C. Cattaneo, A form of heat conduction equation which eliminates the paradox of instantaneous propagation, Comp. Rend., 247 (1958) 431–433.
P. Vernotte, Les paradoxes de la theorie continue de l’equation de la chaleur, Comp. Rend., 246 (1958) 3154–3155.
J. Liu, Z. Ren and C. Wang, Interpretation of living tissue’s temperature oscillations by thermal wave theory, Chinese Sci. Bull., 40 (1995) 1493–1495.
D. Y. Tzou, Macro- to micro-scale heat transfer: The Lagging Behavior, Taylor and Francis, Washington, DC (1997).
M. M. Tung, M. Trujillo, J. A. Lopez Molina, M. J. Rivera and E. J. Berjano, Modeling the heating of biological tissue based on the hyperbolic heat transfer equation, Mathematical and Computers Modelling, 50 (2009) 665–672.
M. Abramowitz and A. Stegun, Handbook of mathematical functions, Dover, New York (1972).
F. Xu, K. A. Seffen and T. J. Lu, Non-Fourier analysis of skin biothermomechanics, Int. J. Heat Mass Transfer, 51 (2008) 2237–2259.
T. C. Shih, P. Yuan, W. L. Lin and H. S. Kou, Analytical analysis of the Pennes bioheat transfer equation with sinusoidal heat flux condition on skin surface, Medical Engineering & Physics, 29 (2007) 946–953.
K. Mitra, S. Kumar, A. Vedavarz and M. K. Moallemi, Experimental evidence of hyperbolic heat conduction in processed meat, J. Heat Transfer, Trans. ASME, 117(3) (1995) 568–573.
L. M Brodie, Welding of Skin using Nd:YAG Laser with Bipolar Contact Applicators, University of Southern Queensland Faculty of Engineering and Surveying (2003).
J. C. Chato, Thermal properties of tissues, Handbook of Bioengineering, New York: Mcgraw-Hill (1987).
M. H. Niemz, Laser-tissue interactions, Springer-Verlag Berlin Heidelberg (2007).
Author information
Authors and Affiliations
Corresponding author
Additional information
Recommended by Associate Editor Dongsik Kim
Hossein Ahmadikia is an assistant professor of Mechanical Engineering at the University of Isfahan, Isfahan, Iran. He received his B.Sc. degree in Ferdosi University, Mashad, Iran in 1990. He received his M.Sc. and Ph.D degrees from Isfahan University of Technology, Isfahan, Iran in 1993 and 2000, respectively. His research focuses on biological heat transfer and turbulence modeling.
Amir Moradi received his B.Sc. degree in Mechanical Engineering from Semnan University, Semnan, Iran in 2008. He received his M.Sc. degree from Bu-Ali sina University, Hamadan, in 2010. His research interests focuses on bioheat transfer and advanced CFD modeling.
Reza Fazlali received his B.Sc. and M.Sc. degrees in Mechanical Engineering from Bu-Ali sina University, Hamadan, Iran in 2007 and 2010, respectively. His research interests focuses on bioheat transfer and analytical solutions for mechanics of fluids.
Amir Basiri Parsa completed his BSc. and MSc. degrees in Mechanical Engineering at the Bu-Ali sina University, Hamedan, Iran in 2008 and 2011, respectively. He is currently a Ph.D student at this University. His research interests include analytical solution for boundary layer problems and optimization of thermodynamics cycles.
Rights and permissions
About this article
Cite this article
Ahmadikia, H., Moradi, A., Fazlali, R. et al. Analytical solution of non-Fourier and Fourier bioheat transfer analysis during laser irradiation of skin tissue. J Mech Sci Technol 26, 1937–1947 (2012). https://doi.org/10.1007/s12206-012-0404-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12206-012-0404-9