Abstract
Background
In the North Central Province of Sri Lanka, chronic kidney disease of uncertain etiology (CKDue) has increased markedly over the past 15–20 years.
Methods
From around 4,700 patients who were followed up, 106 affected patients who visited two local clinics in the endemic area for CKDue on August 10, 2009 and 10 pedigrees of 10 of these cases with familial clustering of CKDue participated in this study. Urine samples, collected from affected patients (n = 106), unaffected relative controls (n = 81), and Japanese controls (n = 50), were analyzed for two tubular markers: α1-microglobulin and N-acetyl-β-d-glucosaminidase. Urine samples from patients with CKDue stages 1–4 (n = 101) and all the samples from unaffected relatives and Japanese controls were analyzed for urinary cadmium concentration.
Results
Urinary excretion of α1-microglobulin was elevated even in the earliest stage of CKDue compared with its levels in unaffected relative controls. Urinary excretion of N-acetyl-β-d-glucosaminidase was elevated only in stage 5. In contrast, urinary cadmium excretion was similar in CKDue patients and in the unaffected relative controls, and levels in both these groups were significantly lower than the level in the Japanese controls. All levels were below the threshold level for renal toxicity, indicating the absence of any evidence of cadmium toxicity.
Conclusions
The present study indicates that renal tubular damage occurs in the very early stage of CKDue and demonstrates the existence of familial clustering, suggesting that CKDue is likely to be the outcome of exposure to an unknown nephrotoxin in susceptible subjects in the endemic region.
Similar content being viewed by others
Introduction
The North Central Province (NCP) in the dry zone of Sri Lanka has a total land area of 10,472 km2 and is occupied by about 1.1 million people [1]. The prevalence of an endemic condition of chronic kidney disease (CKD) has dramatically increased over the past 15 years, affecting the low socioeconomic level farming community in the NCP [2–5]. Recently, the disease has also been identified in two neighboring provinces, North Western Province and Uva Province (Fig. 1). Because young farmers are the vulnerable community, CKD has a huge negative impact on the economic and social development of the region. Furthermore, CKD requires long-term care and its treatment is a substantial burden on the healthcare system [6].
The causes of CKD are many, including diabetes, hypertension, chronic glomerulonephritis, tubulointerstitial fibrosis, and exposure to nephrotoxins such as cadmium or aristolochic acid [7]. However, CKD in the NCP is not associated with any identifiable predisposing factors. It is characterized by proteinuria and a low glomerular filtration rate (GFR) resulting in end-stage renal disease. Although several studies have been carried out and the involvement of environmental and/or genetic factors has been strongly suggested [6], the etiology of CKD in this region remains elusive; hence its name, CKD of uncertain etiology (CKDue).
Recently, Bandara and co-workers [4, 5] reported that intensive exposure to cadmium occurred in patients with CKDue. However, such intensive exposure was not confirmed by other ecological investigations [8] and the pathogenesis of CKDue remains unresolved.
The urinary tubular markers α1-microglobulin (A1M) and N-acetyl-β-d-glucosaminidase (NAG) are sensitive exposure markers in cadmium-polluted and non-polluted areas [9, 10]. These renal tubular markers have never been evaluated in CKDue patients. They may, however, provide insights into the possible etiology and pathogenesis of CKDue. We conducted a preliminary study to evaluate renal tubular function in the CKDue population and in unaffected relatives in the NCP and to investigate whether cadmium might play a role in the pathogenesis of CKDue.
The investigation revealed both that renal tubular damage occurred at the very early stage of CKDue and that there was familial clustering. Further, it was confirmed that CKDue is not a cadmium induced nephropathy.
Subjects, materials, and methods
Ethical statement
Ethical approval for the study was obtained both from Kyoto University Graduate School of Medicine, Kyoto, Japan and the University of Peradeniya, Sri Lanka. All clinical records and biological samples were obtained after informed consent was received from the subjects,, and investigations were carried out in accordance with the Helsinki Declaration.
Study population
The Medawachchiya and Girandurukotte Divisional Secretariats, known as areas with a high prevalence of CKDue, were selected for the study (Fig. 1) [3]. The total population in Medawachchiya was 48,451 and in Girandurukotte it was 37,470 [1]. Because of the increasing number of admissions of patients with CKDue to the local renal units, population screening in these endemic areas, using proteinuria, was started in 2003. House-to-house screening using dipstick proteinuria was carried out by trained public health midwives. Early morning samples of the urine of all household members above 5 years of age (except for menstruating females) were checked on three occasions, with an interval of 1 week between consecutive samples. Subjects with proteinuria on two or more occasions were defined as CKDue patients and were referred to renal clinics for further confirmatory investigations and follow-up. According to the screening program, the prevalence of CKDue was 3.7% in Medawachchiya and 3.9% in Girandurukotte.
CKDue patients
Currently, around 2,500 CKDue patients at Medawachchiya renal clinic and around 2,200 CKDue patients at Girandurukotte renal clinic (Fig. 1), who were diagnosed by the screening program from 2003, are being regularly followed up. Of these patients, 63 from Medawachchiya renal clinic and 43 patients from Girandurukotte renal clinic who attended these clinics on August 10, 2009 joined the study. Demographic data and clinical and family history were obtained by face-to-face interviews using a structured questionnaire and from the hospital-based medical records. Patients were categorized into five stages (hereafter referred to as CKDue stages) following the National Kidney Foundation Kidney Disease Outcome Quality Initiative guidelines [11] and based on the latest glomerular filtration rate (GFR). The modified diet in renal disease (MDRD) formula [GFR (ml/min/1.73 m2) = 186 × Scr−1.154 × (Age)−0.203 × (0.742 if female) × (1.212 if African American)] using Serum creatinine (Scr) levels was used to estimate GFR [12]. Glomerular filtration is considered to be the best estimate of kidney function. In most healthy people, the GFR is 90 ml/min/1.73 m2 or higher. However, people with GFRs of ≥90 ml/min/1.73 m2, but with evidence of kidney damage, were included in the patients with stage 1 CKD. Patients with GFRs in the ranges 60–89, 30–59, and 15–29 ml/min/1.73 m2 were assigned to stages 2, 3, and 4, respectively, and when the GFR was <15 ml/min/1.73 m2 the patients were considered to be stage 5 [11].
Unaffected relatives as controls
We invited unaffected first- to third-generation blood relatives of the patients, who reside in the same communities in Medawachchiya and Girandurukotte, to join our control group.
Japanese controls
Urine samples from 50 members of the Japanese general population with no specific morbidity were donated by the Kyoto Human Specimen Bank [13, 14]. The samples were collected in Kyoto city from apparently healthy individuals residing in areas with no particular cadmium exposure.
Urine sample collection, transportation, and storage
Spot urine samples from CKDue patients and their unaffected relatives were stored in ice immediately after collection and brought to the University of Peradeniya, where they were stored at −10°C. The frozen urine samples were put into dry ice and transported to Japan where they were stored in the Kyoto Human Specimen Bank at −30°C until they were analyzed. The Japanese urine samples were stored at −30°C, 4 h after collection.
Analytical methods
All the urine samples from CKDue patients, relative controls, and Japanese controls were analyzed for two tubular biomarkers; A1M and NAG. β2-microglobulin was not analyzed because it shows lower stability than A1M. Urinary cadmium analysis was done for all the urine samples, except for the five samples collected from CKDue stage 5 patients. Urinary A1M, NAG, cadmium, and creatinine concentrations were measured at Special Reference Laboratories Incorporated in Tokyo, Japan. Urinary A1M was determined by latex agglutination immunoassays and urinary NAG concentrations were estimated by calorimetric assay. An enzymatic assay using creatinine amidohydrolase was used to determine urinary creatinine concentrations. Urinary cadmium concentration was measured with a Z-8100 graphite furnace atomic absorption spectrophotometer (Hitachi High-Technologies Corporation, Tokyo, Japan). The spectrophotometer is a single-beam instrument equipped with a deuterium lamp for background correction. Distilled and de-ionized water was used to prepare all the standards and matrix solutions. The matrix solutions, NH4NO3, NH4F, and (NH4)2HPO4, at concentrations of 10 g/l, were treated with ammonium pyrrolidine dithiocarbamate as the complexing agent and extracted with methyl isobutyl ketone. For urinary cadmium analysis, the spectrophotometer slit width was set at 320 μm and the wavelength was 228.8 nm. The peak height was measured and digitally recorded. The flameless sampler was used at atmospheric pressure, and argon was the purge gas, with a gas flow of 20 standard cubic foot per hour (SCFH; 1 SCFH = 0.47 l/h). The minimum detectable limit was 0.4 μg/l.
Statistical analysis
The results are expressed as means (with arithmetic standard deviation), medians, ranges, and percentages. Figures are graphically displayed as box and whisker plots. Differences of P < 0.05 were considered to be statistically significant. A comparison of the excretion of A1M and NAG between CKDue cases and the controls (Sri Lankan and Japanese) and between different CKDue stages (stage 1 to stage 5) was made by the analysis of variance (ANOVA) test. If the ANOVA results were significant, then the Student–Newman–Keuls (SNK) multiple range test was carried out. Various combinations of A1M and NAG levels and the ages of the patients at different CKDue stages were further analyzed using Spearman’s rank correlation coefficients. The levels of the two tubular markers in the two control groups (Sri Lankan and Japanese) were compared using Welch’s t-test for unequal variance. Differences were further checked by the SNK multiple range test.
All statistical procedures were performed using SAS version 9.1 (supplied by the SAS Institute, Cary, NC, USA).
Results and discussion
Demographic characteristics of the patients and pedigrees
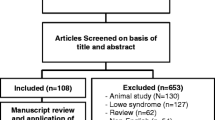
The gender and clinical stage distributions of the patients are shown in Table 1. Of the 106 patients, 5 patients from the Medawachchiya clinic and 5 from the Girandurukotte clinic exhibited familial clustering of CKDue. Eighty-seven blood relatives (28 in Medawachchiya and 59 in Girandurukotte), who had previously undergone screening and had tested negative for CKDue, were retested for proteinuria in August 2009. Of these 87 individuals, 81 (26 in Medawachchiya and 55 in Girandurukotte) were confirmed as negative and were recruited as unaffected relative controls. The age and gender of the relative controls in individual pedigrees are summarized in Table 2, and the pedigrees are illustrated in Fig. 2.
Pedigrees of the families with chronic kidney disease of uncertain etiology (CKDue) that participated in the study. Families G1–5 and M1–5 were from Girandurukotte and Medawachchiya, respectively. Asterisks indicate members who joined this study as CKDue patients and unaffected relative controls, plus symbols indicate individuals who were later found to have proteinuria and were therefore excluded from this study. Solid symbols indicate patients. Circles represent females and squares represent males. Slashed lines through symbols indicate deceased individuals. The ages of all the participants on the day of the sample collection are shown in years (y) below the symbols. Arrows indicate the probands
Although rigorous genetic analysis was impossible, the pattern of CKDue does not support the notion of a single gene disease. For the typical autosomal dominant mode, the expected penetrance is 50%, much higher than was observed. In several families there were more than two generations with unaffected parents; thus, the pattern does not support the autosomal recessive mode either. In addition, male-to-male transmission was found in several pedigrees, and so an X-linked mode of inheritance could be rejected. In several pedigrees, CKDue was transmitted from both the maternal and the paternal sides, suggesting that there might be susceptible polymorphisms with relatively large allele frequencies. The penetrance of CKDue is age-dependent and patients are limited to mostly the first and second generations within three-generation families. Inheritance patterns matched those of multifactorial diseases with a high phenocopy prevalence [15].
Urinary A1M and NAG concentrations
We analyzed A1M and NAG concentrations in urine samples from CKDue patients in all five CKDue stages (n = 106), from the relative controls (n = 81), and from the set of people from Japan who served as non-endemic controls (n = 50). To account for variations in urine concentrations among individuals, all concentrations were expressed in units per gram urinary creatinine excretion. Tentative cut-off values (5 mg/g creatinine for A1M, and 3.5 U/g creatinine for NAG) for screening were set based on previous publications so that even early stages of renal tubular damage could be identified [9, 16–21].
Table 1 shows the urinary concentrations of the two tubular markers in the CKDue patients at different clinical stages, in the relative controls, and in the Japanese controls.
Compared with the relative controls, A1M excretion was significantly higher in CKDue stage 1 (P < 0.05) and steadily increased through the early stages 1–3 (Table 1 and Fig. 3). However, the difference in NAG excretion was found to be significant only in stage 5 (Table 1), indicating that excretion of NAG was elevated only in the late stages of the disease. In contrast, A1M excretion was significantly higher in CKDue patients from the onset of the disease. There was no significant difference in the excretion patterns of the two tubular markers between the relative controls and the Japanese controls. Because the relative controls were significantly younger than the Japanese controls, for comparison we excluded all members of the control groups who were below the age of 20 years. Even after the correction for age, the excretion of A1M and NAG in the relative controls was very similar to their excretion in the Japanese controls (P > 0.05) (Table 3).
Urinary excretion of α1-microglobulin (A1M) in the endemic relative controls and patients in the early stages of CKDue. Filled circles indicate the A1M values of individual patients/controls, open circles indicate the geometric means for CKDue stages 1-3. The upper and lower error bars show the first and third quartiles for CKDue stages 1-3. CKDue chronic kidney disease of uncertain etiology, Cr creatinine
We further analyzed various combinations of age, A1M, NAG, and CKDue stages using Spearman’s rank correlation coefficient (ρ) (Table 4). A1M had a stronger correlation with CKDue stage than did NAG. The analysis showed that the age of the CKDue patients was positively correlated with CKDue clinical stage (ρ = 0.74; P < 0.0001).
Urinary excretion of cadmium
Urine samples from CKDue patients in CKDue stages 1–4 (n = 101), and from relative (n = 81) and Japanese controls (n = 50) were analyzed for cadmium concentration, which was expressed as units per gram urinary creatinine excretion (Table 5). CKDue stage 5 patients were not considered in this analysis, because when the renal tubular system is damaged urinary cadmium cannot be used as a reliable predictor of cadmium body burden or renal accumulation [9].
All CKDue stages and relative controls had remarkably lower cadmium excretion levels in urine compared with the Japanese controls, replicating the results we had obtained in our previous preliminary investigations [8]. When the CKDue patients and the relative controls were compared, there was no significant difference in urinary cadmium excretion between the two groups that reside in the same residential area (P = 0.94) However, Japanese (non-endemic) controls had significantly higher cadmium excretion in urine than the relative (endemic) controls (P < 0.0001). We did not observe a significant correlation between urinary cadmium excretion and tubular biomarkers in our study population (Table 4).
This investigation found that elevations of urinary excretion of A1M were discernible in CKDue patients in the earliest stage when compared with findings in the relative controls residing in the same geographical region or with the findings in the Japanese controls. As indicated by the excretion pattern of the tubular marker in the CKDue patients, tubular damage clearly occurs early in the disease process and progresses as the disease advances. Our investigations also showed that cadmium exposure in the endemic region was almost negligible, confirming earlier findings that cadmium is unlikely to be associated with CKDue pathogenesis [8].
We also confirmed familial clustering in 10 pedigrees. The inheritance patterns do not suggest a single gene disease but look more like the patterns associated with multifactorial diseases. Populations with both susceptibility genes and environmental factors may be predisposed to CKDue. Further study is warranted to investigate CKDue from the viewpoint of both susceptibility genes and environmental factors.
A1M is a 27-kDa glycoprotein produced by the liver [22] and is a sensitive marker for proximal tubular damage [23]. Nephrotoxic substances that damage the tubules are known to elevate the urinary excretion of A1M. These toxic substances include heavy metals such as cadmium [9], mercury [24], and lead [25], as well as drugs such as aminoglycosides, cyclosporine, and analgesics [26]. It is of particular interest that A1M is also elevated in Balkan endemic nephropathy (BEN) [27].
BEN is an endemic nephropathy similar to CKDue that occurs only in certain endemic rural foci along tributaries of the River Danube in the Balkan countries of Bosnia, Bulgaria, Croatia, Romania, and Serbia. The etiology of BEN is still uncertain [28], but the evidence supports the conclusion that the chronic interstitial nephritis in BEN is the combined result of environmental and genetic factors [28, 29]. Similarly, CKDue is more likely to be a multifactorial disease rather than having a single cause. The familial clustering of CKDue patients (Fig. 2) and the high prevalence of the disease in low socioeconomic level farming communities also suggest a complex interplay between genetic and environmental factors that ultimately affect the clinical outcome [30].
In the present study, we found no evidence to support the reports of Bandara et al. [4, 5], because we did not detect any significant change in any of the tubular markers in the unaffected blood relative controls. Indeed, the urinary cadmium concentrations in the CKDue patients and their relatives were significantly lower than the cadmium concentrations in the apparently healthy Japanese controls from a cadmium non-polluted area. These observations suggest that the exposure levels, if any, of cadmium in the population in the CKDue endemic areas are not intense.
The present study has several limitations. The patients, unaffected relatives, and the Japanese controls were not age- or sex-matched and the screening was limited to only two renal markers. Furthermore, because of the small number of participants and the resultant low statistical power, the possibility of false-negative results cannot be excluded. Future investigations will focus on the elucidation of the pathological process in the renal tubular cells and the underlying etiological factor/s.
Conclusions
We conclude that, in CKDue, renal tubular damage is initiated at an early stage of the pathological process and progresses as the disease advances. This study has revealed the real possibility of the existence of a renal tubular toxin other than cadmium in this endemic region of the North Central Province of Sri Lanka. In addition, familial clustering strongly suggests the presence of susceptibility genes. These results indicate clear areas for further study to elucidate the etiology and pathogenesis of renal tubular damage in CKDue.
References
Statistical abstract. Department of Census and Statistics, Sri Lanka. 2009. http://www.statistics.gov.lk/abstract2009/Pages/index.htm.
Athuraliya TN, Abeysekera DT, Amerasinghe PH, Kumarasiri PV, Dissanayake. Prevalence of chronic kidney disease in two tertiary care hospitals: high proportion of cases with uncertain aetiology. Ceylon Med. 2009;54:23–5.
World Health Organization (WHO) country office Sri Lanka. News letters. http://www.whosrilanka.org/EN/Section1_76.htm. Accessed 20 Dec 2010.
Bandara JMRS, Senevirathna DMA, Dasanayake DMRSV, Herath V, Bandara JMRP, Abeysekara T, Rajapaksha KH. Chronic renal failure in cascade irrigation systems in Sri Lanka associated with elevated dietary cadmium levels, rice and fresh water fish (Thilapia). Environ Geochem Health. 2008;30:465–78.
Bandara JM, Wijewardena HV, Liyanege J, Upul MA, Bandara. Chronic renal failure in Sri Lanka caused by elevated dietary cadmium: Trojan horse of the green revolution. Toxicol Lett. 2010;198:33–9.
Wanigasuriya KP, Peiris-John RJ, Wickremasinghe R, Hittarage A. Chronic renal failure in North Central Province of Sri Lanka: an environmentally induced disease. Trans R Soc Trop Med Hyg. 2007;101:1013–7.
Soderland P, Lovekar S, Weiner DE, Brooks DR, Kaufman JS. Chronic kidney disease associated with environmental toxins and exposure. Adv Chronic Kidney Dis. 2010;17:254–64.
Chandrajith R, Nanayakkara S, Itai K, Aturaliya TN, Dissanayake CB, Abeysekara T, Harada K, Watanabe T, Koizumi A. Chronic kidney disease of uncertain aetiology (CKDuee) in Sri Lanka: geographic distribution and environmental implications. Environ Geochem Health. 2011;33:267–78.
Järup L, Akesson A. Current status of cadmium as an environmental health problem. Toxicol Appl Pharmacol. 2009;238:201–8.
Moriguchi J, Inoue Y, Kamiyama S, Horiguchi M, Murata K, Sakuragi S, Fukui Y, Ohashi F, Ikeda M. N-acetyl-beta-d-glucosaminidase (NAG) as the most sensitive marker for tubular dysfunction for monitoring residents in non-polluted areas. Toxicol Lett. 2009;190:1–8.
National Kidney Foundation (NKF). KDOQI Clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. http://www.kidney.org/professionals/KDOQI/guidelines_ckd/toc.htm. Accessed 20 Dec 2010.
Kooman JP. Estimation of renal function in patients with chronic kidney disease. J Magn Reson Imaging. 2009;30:1341–6.
Koizumi A, Harada KH, Inoue K, Hitomi T, Yang HR, Moon CS, Wang P, Hung NN, Watanabe T, Shimbo S, Ikeda M. Past, present and future of environmental specimen banks. Environ Health Prev Med. 2009;14:307–18.
Koizumi A Yoshinaga T, Harada K, Inoue K, Morikawa, Muroi J, Inoue S, Eslami B, Fujii S, Fujimine Y, Hachiya N, Koda S, Kusaka Y, Murata K, Nakatsuka H, Omae K, Saito N, Shimbo S, Takenaka K, Takeshita T, Todoriki H, Wada Y, Watanabe T, Ikeda M. Assessment of human exposure to polychlorinated and polybrominated diphenyl ethers in Japan using early 1980s and mid 1990s archive samples. Environ Res. 2005; 99:31–9.
Bodmer W, Bonilla C. Common and rare variants in multifactorial susceptibility to common diseases. Nat Genet. 2008;40:695–701.
Ikeda M, Ohashi F, Fukui Y, Takada S, Moriguchi J, Ezaki T. Changes in tubular dysfunction marker levels in parallel with the levels of copper, rather than cadmium, in urine of middle-aged women in non-polluted areas. Int Arch Occup Environ Health. 2007;80:171–83.
Yamagami T, Suna T, Fukui Y, Ohashi F, Takada S, Sakurai H, Aoshima K, Ikeda M. Biological variations in cadmium, alpha 1-microglobulin, beta 2-microglobulin and N-acetyl-beta-d-glucosaminidase in adult women in a non-polluted area. Int Arch Occup Environ Health. 2008;81:263–71.
Ikeda M, Ezaki T, Tsukahara T, Moriguchi J, Furuki K, Fukui Y, Ukai SH, Okamoto, Sakurai H. Critical evaluation of alpha1- and beta2-microglobulins in urine as markers of cadmium-induced tubular dysfunction. Biometals. 2004;17:539–41.
Kobayashi E, Suwazono Y, Uetani M, Inaba T, Oishi M, Kido T, Nishijo M, Nakagawa H, Nogawa K. Estimation of benchmark dose as the threshold levels of urinary cadmium, based on excretion of total protein, beta2-microglobulin, and N-acetyl-beta-d-glucosaminidase in cadmium nonpolluted regions in Japan. Environ Res. 2006;101:401–6.
Uno T, Kobayashi E, Suwazono Y, Okubo Y, Miura K, Sakata K, Okayama A, Ueshima H, Nakagawa H, Nogawa K. Health effects of cadmium exposure in the general environment in Japan with special reference to the lower limit of the benchmark dose as the threshold level of urinary cadmium. Scand J Work Environ Health. 2005;31:307–15.
Bernard A. Cadmium and its adverse effects on human health. Indian J Med Res. 2008;128:557–64.
Vincent C, Marceau M, Blangarin P, Bouic P, Madjar JJ, Revillard JP. Purification of alpha 1-microglobulin produced by human hepatoma cell lines. Biochemical characterization and comparison with alpha 1-microglobulin synthesized by human hepatocytes. Eur J Biochem. 1987;165:699–704.
Yu H, Yanagisawa Y, Forbes MA, Cooper EH, Crockson RA, MacLennan ICM. Alpha-1-microglobulin: an inhibitor protein for renal tubular function. J Clin Pathol. 1983;36:253–9.
Franko A, Budihna MV, Dodic-Fikfak M. Long-term effects of elemental mercury on renal function in miners of the Idrija Mercury Mine. Ann Occup Hyg. 2005;49:521–7.
Pergande M, Jung K, Percht S, Fels LM, Herbort C, Stolte H. Changed excretion of urinary proteins and enzymes by chronic exposure to lead. Nephrol Dial Transplant. 1994;9:613–8.
Penders J, Delanghe JR. Alpha 1-microglobulin: clinical laboratory aspects and applications. Clin Chim Acta. 2004;346:107–18.
Cvorisec D. Early diagnosis of endemic nephropathy. Clin Chim Acta. 2000;297:85–91.
Stefanović V, Polenaković M. Fifty years of research in Balkan endemic nephropathy: where are we now? Nephron Clin Pract. 2009;112:c51–6.
Toncheva D, Dimitrov T. Genetic predisposition to Balkan endemic nephropathy. Nephron. 1996;72:564–9.
Luttropp K, Stenvinkel P, Carrero JJ, Pecoits-Filho R, Lindholm B, Nordfors L. Understanding the role of genetic polymorphisms in chronic kidney disease. Pediatr Nephrol. 2008;23:1941–9.
Acknowledgments
We are grateful to Professor C.M. Madduma Bandara (Emeritus professor), Professor Yasuhiko Wada (University of Kochi, Faculty of Health Science, Kochi, Japan), and Professor Katsunobu Takenaka (Department of Neurosurgery, Takayama Red Cross Hospital, Takayama, Japan), for their support during this study. This study was supported by the Special Coordination Funds for Promoting Science and Technology from the Ministry of Education, Culture, Sports, Science and Technology in Japan. The funding agency had no role in the study design, data collection, and analysis, or in the decision to publish or in the preparation of the manuscript.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the Chronic Kidney Disease of Uncertain etiology Consortium. A full list of Consortium members is provided in the Electronic supplementary material.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional files Additional file 1 – Members of the CKDue consortium.
Rights and permissions
About this article
Cite this article
Nanayakkara, S., Senevirathna, S.T.M.L.D., Karunaratne, U. et al. Evidence of tubular damage in the very early stage of chronic kidney disease of uncertain etiology in the North Central Province of Sri Lanka: a cross-sectional study. Environ Health Prev Med 17, 109–117 (2012). https://doi.org/10.1007/s12199-011-0224-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12199-011-0224-z