Abstract
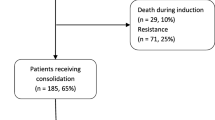
Invasive fungal disease (IFD) is a major cause of morbidity and mortality in acute leukemia (AL) patients. The impact of primary antifungal prophylaxis (PAP) on AL patients with different risk factors is unclear. We analyzed 2015 Chinese AL patients who received a total of 2274 chemotherapy courses, including 1410 courses in acute myeloid leukemia (AML) patients and 864 courses in acute lymphocytic leukemia (ALL) patients. The IFD incidence was significantly higher among AML than ALL patients (11.8 vs. 7.1%, P < 0.001) and in patients receiving induction chemotherapy than in those receiving consolidation chemotherapy (21.6 vs. 3.7%, P < 0.001). Induction chemotherapy, decreased serum albumin, indwelling central venous catheters, parenteral nutrition, and male gender were independent risk factors for IFD in AL patients, whereas PAP independently protected against IFD development. For patients on induction chemotherapy, PAP significantly reduced IFD incidence (P < 0.001). For patients on consolidation chemotherapy, however, PAP did not significantly alter IFD incidence, although PAP did lower IFD incidence in patients with certain risk factors. PAP is highly recommended for patients on induction therapy; for those on consolidation chemotherapy, PAP should be considered for patients who present with severe neutropenia, decreased albumin, and/or an indwelling central venous catheter.
Similar content being viewed by others
References
Kriengkauykiat J, Ito JI, Dadwal SS. Epidemiology and treatment approaches in management of invasive fungal infections. Clin Epidemiol. 2011;3:175–91.
Neofytos D, Lu K, Hatfield-Seung A, Blackford A, Marr KA, Treadway S, et al. Epidemiology, outcomes, and risk factors of invasive fungal infections in adult patients with acute myelogenous leukemia after induction chemotherapy. Diagn Microbiol Infect Dis. 2013;75:144–9.
Pagano L, Caira M, Candoni A, Offidani M, Martino B, Specchia G, et al. Invasive aspergillosis in patients with acute myeloid leukemia: a seifem-2008 registry study. Haematologica. 2010;95:644–50.
Menzin J, Meyers JL, Friedman M, Perfect JR, Langston AA, Danna RP, et al. Mortality, length of hospitalization, and costs associated with invasive fungal infections in high-risk patients. Am J Health Syst Pharm. 2009;66:1711–7.
Slobbe L, Polinder S, Doorduijn JK, Lugtenburg PJ, el Barzouhi A, Steyerberg EW, et al. Outcome and medical costs of patients with invasive aspergillosis and acute myelogenous leukemia-myelodysplastic syndrome treated with intensive chemotherapy: an observational study. Clin Infect Dis. 2008;47:1507–12.
Even C, Bastuji-Garin S, Hicheri Y, Pautas C, Botterel F, Maury S, et al. Impact of invasive fungal disease on the chemotherapy schedule and event-free survival in acute leukemia patients who survived fungal disease: a case–control study. Haematologica. 2011;96:337–41.
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the european organization for research and treatment of cancer/invasive fungal infections cooperative group and the national institute of allergy and infectious diseases mycoses study group (eortc/msg) consensus group. Clin Infect Dis. 2008;46:1813–21.
Lewis G, Hall P, Eisa N, Deremer D, Dobbins R, El-Geneidy M, et al. Acute myelogenous leukemia patients are at low risk for invasive fungal infections after high-dose cytarabine consolidations and thus do not require prophylaxis. Acta Haematol. 2010;124:206–13.
Heng SC, Slavin MA, Al-Badriyeh D, Kirsa S, Seymour JF, Grigg A, et al. Pharmacoeconomic evaluation of fluconazole, posaconazole and voriconazole for antifungal prophylaxis in patients with acute myeloid leukaemia undergoing first consolidation chemotherapy. J Antimicrob Chemother. 2013;68:1669–78.
Sun Y, Huang H, Chen J, Li J, Ma J, Li J, et al. Invasive fungal infection in patients receiving chemotherapy for hematological malignancy: a multicenter, prospective, observational study in china. Tumour Biol. 2015;36:757–67.
Bhatt VR, Viola GM, Ferrajoli A. Invasive fungal infections in acute leukemia. Ther Adv Hematol. 2011;2:231–47.
Cornely OA, Cuenca-Estrella M, Meis JF, Ullmann AJ. European society of clinical microbiology and infectious diseases (escmid) fungal infection study group (efisg) and european confederation of medical mycology (ecmm) 2013 joint guidelines on diagnosis and management of rare and emerging fungal diseases. Clin Microbiol Infect. 2014;20(Suppl 3):1–4.
Arendrup MC, Boekhout T, Akova M, Meis JF, Cornely OA, Lortholary O, et al. Escmid and ecmm joint clinical guidelines for the diagnosis and management of rare invasive yeast infections. Clin Microbiol Infect. 2014;20(Suppl 3):76–98.
Mousset S, Buchheidt D, Heinz W, Ruhnke M, Cornely OA, Egerer G, et al. Treatment of invasive fungal infections in cancer patients-updated recommendations of the infectious diseases working party (agiho) of the german society of hematology and oncology (dgho). Ann Hematol. 2014;93:13–32.
Ullmann AJ, Akova M, Herbrecht R, Viscoli C, Arendrup MC, Arikan-Akdagli S, et al. Escmid guideline for the diagnosis and management of candida diseases 2012: adults with haematological malignancies and after haematopoietic stem cell transplantation (hct). Clin Microbiol Infect. 2012;18(Suppl 7):53–67.
Alothman AF, Al-Musawi T, Al-Abdely HM, Salman JA, Almaslamani M, Yared N, et al. Clinical practice guidelines for the management of invasive candida infections in adults in the middle east region: expert panel recommendations. J Infect Public Health. 2014;7:6–19.
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2011;52:e56–93.
Flowers CR, Seidenfeld J, Bow EJ, Karten C, Gleason C, Hawley DK, et al. Antimicrobial prophylaxis and outpatient management of fever and neutropenia in adults treated for malignancy: american society of clinical oncology clinical practice guideline. J Clin Oncol. 2013;31:794–810.
Pagano L, Caira M. The role of primary antifungal prophylaxis in patients with haematological malignancies. Clin Microbiol Infect. 2014;20(Suppl 6):19–26.
Gomes MZ, Mulanovich VE, Jiang Y, Lewis RE, Kontoyiannis DP. Incidence density of invasive fungal infections during primary antifungal prophylaxis in newly diagnosed acute myeloid leukemia patients in a tertiary cancer center, 2009 to 2011. Antimicrob Agents Chemother. 2014;58:865–73.
Gerber B, Koppel J, Paul M, Nguyen-Kim TD, Frauenfelder T, Nair G, et al. Efficacy of anti-fungal but not anti-bacterial prophylaxis in intensive primary AML therapy: a real-world, retrospective comparative single-centre study. Swiss Med Wkly. 2014;144:w13985.
Pagano L, Caira M, Candoni A, Aversa F, Castagnola C, Caramatti C, et al. Evaluation of the practice of antifungal prophylaxis use in patients with newly diagnosed acute myeloid leukemia: results from the seifem 2010-b registry. Clin Infect Dis. 2012;55:1515–21.
Yeh TC, Liu HC, Hou JY, Chen KH, Huang TH, Chang CY, et al. Severe infections in children with acute leukemia undergoing intensive chemotherapy can successfully be prevented by ciprofloxacin, voriconazole, or micafungin prophylaxis. Cancer. 2014;120:1255–62.
Fisher BT, Kavcic M, Li Y, Seif AE, Bagatell R, Huang YS, et al. Antifungal prophylaxis associated with decreased induction mortality rates and resources utilized in children with new-onset acute myeloid leukemia. Clin Infect Dis. 2014;58:502–8.
Robenshtok E, Gafter-Gvili A, Goldberg E, Weinberger M, Yeshurun M, Leibovici L, et al. Antifungal prophylaxis in cancer patients after chemotherapy or hematopoietic stem-cell transplantation: systematic review and meta-analysis. J Clin Oncol. 2007;25:5471–89.
Kobayashi R, Kaneda M, Sato T, Ichikawa M, Suzuki D, Ariga T. The clinical feature of invasive fungal infection in pediatric patients with hematologic and malignant diseases: a 10-year analysis at a single institution at Japan. J Pediatr Hematol Oncol. 2008;30:886–90.
Prentice HG, Kibbler CC, Prentice AG. Towards a targeted, risk-based, antifungal strategy in neutropenic patients. Br J Haematol. 2000;110:273–84.
Pagano L, Caira M, Valentini CG, Posteraro B, Fianchi L. Current therapeutic approaches to fungal infections in immunocompromised hematological patients. Blood Rev. 2010;24:51–61.
Muhlemann K, Wenger C, Zenhausern R, Tauber MG. Risk factors for invasive aspergillosis in neutropenic patients with hematologic malignancies. Leukemia. 2005;19:545–50.
Marr KA, Carter RA, Boeckh M, Martin P, Corey L. Invasive aspergillosis in allogeneic stem cell transplant recipients: changes in epidemiology and risk factors. Blood. 2002;100:4358–66.
Kaya Z, Gursel T, Kocak U, Aral YZ, Kalkanci A, Albayrak M. Invasive fungal infections in pediatric leukemia patients receiving fluconazole prophylaxis. Pediatr Blood Cancer. 2009;52:470–5.
Gerson SL, Talbot GH, Hurwitz S, Strom BL, Lusk EJ, Cassileth PA. Prolonged granulocytopenia: the major risk factor for invasive pulmonary aspergillosis in patients with acute leukemia. Ann Intern Med. 1984;100:345–51.
Acknowledgements
This work was supported by Merck Sharp & Dohme China.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
The original version of this article was revised: Table 1 was published incorrectly with rows out of order and it was corrected.
An erratum to this article is available at http://dx.doi.org/10.1007/s12185-017-2269-2.
About this article
Cite this article
Zhang, R., Chen, J., Huang, H. et al. Primary fungal prophylaxis in acute leukemia patients with different risk factors: retrospective analysis from the CAESAR study. Int J Hematol 106, 221–228 (2017). https://doi.org/10.1007/s12185-017-2224-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-017-2224-2