Abstract
Objective
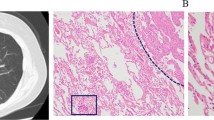
The goal of our study was to demonstrate the clinical usefulness of positron emission tomography/computed tomography (PET/CT) for adenocarcinoma with bronchioloalveolar carcinoma (BAC) features, through evaluating the relationship between the intrathoracic lymph node metastases and maximum standardized uptake value (SUVmax), tumor size of the primary tumor and the ratio of BAC component and analysing the correlation of SUVmax, tumor size and the ratio of BAC component.
Methods
This was a retrospective study. Forty-five patients with focal peripheral lung adenocarcinoma with BAC features were included in this study and underwent the PET/CT scan. Twenty-one patients were women and 24 were men. None of the patients had insulin-dependent diabetes and the serum glucose levels in all patients just before 18F-FDG was injected were less than 120 mg/dl. The diagnosis of the lesion was made by surgical histopathology.
Results
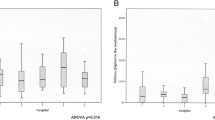
All patients underwent successful surgery, and pathologic examination confirmed that 34 of 118 excised nodal groups in 18 patients were proved to be positive for malignancy. Univariate analysis revealed 3 potential factors related to intrathoracic lymph node metastases: SUVmax (P = 0.002); the ratio of BAC component (P = 0.002); maximum dimension of a tumor on mediastinal window setting images (mDmax, P = 0.025). The maximum dimension of a tumor on pulmonary window setting images (pDmax, P = 0.373) had no significance. A receiver operating characteristic (ROC) curve based on SUVmax, mDmax and the ratio of BAC component was constructed, the area under curve (AUC) was 85.2, 70.3 and 81.5% separately. There was no statistical significance between AUC of SUVmax and AUC of the ratio of BAC component (Z = 0.901, P = 0.368). The AUC of SUVmax and AUC of the ratio of BAC component were significantly higher than AUC of mDmax (Z = 2.112, P = 0.035; Z = 2.016, P = 0.042).The SUVmax and the ratio of BAC component had significant inverse correlation (r = −0.85, P < 0.01). The mDmax and the ratio of BAC component had significant inverse correlation (r = −0.69, P < 0.01). The SUVmax and mDmax had significant correlation (r = 0.60, P < 0.01).
Conclusions
PET/CT would be clinically useful for adenocarcinoma with BAC features, because SUVmax obtained by PET/CT can predict the incidence of intrathoracic lymph node metastases at preoperative stages and even for inoperable patients.



Similar content being viewed by others
References
Travis WD, Garg K, Franklin WA, Wistuba II, Sabloff B, Noguchi M, et al. Evolving concepts in the pathology and computed tomography imaging of lung adenocarcinoma and bronchioloalveolar carcinoma. J Clin Oncol. 2005;23:3279–87.
Read WL, Page NC, Tierney RM, Piccirillo JF, Govindan R. The epidemiology of bronchioloalveolar carcinoma over the past two decades: analysis of the SEER database. Lung Cancer. 2004;45:137–42.
Ebright MI, Zakowski MF, Martin J, Venkatraman ES, Miller VA, Bains MS, et al. Clinical pattern and pathologic stage but not histologic features predict outcome for bronchioloalveolar carcinoma. Ann Thorac Surg. 2002;74:1640–6.
Raz DJ, He B, Rosell R, Jablons DM. Current concepts in bronchioloalveolar carcinoma biology. Clin Cancer Res. 2006;12:3698–704.
Vansteenkiste JF, Stroobants SG, Dupont PJ, De Leyn PR, Verbeken EK, Deneffe GJ, et al. Prognostic importance of the standardized uptake value on (18)F-fluoro-2-deoxy-glucose-positron emission tomography scan in non-small-cell lung cancer: an analysis of 125 cases Leuven Lung Cancer Group. J Clin Oncol. 1999;17:3201–6.
Cerfolio RJ, Bryant AS, Ohja B, Bartolucci AA. The maximum standardized uptake values on positron emission tomography of a non-small cell lung cancer predict stage, recurrence, and survival. J Thorac Cardiovasc Surg. 2005;130:151–9.
Higashiyama M, Kodama K, Yokouchi H, Takami K, Mano M, Kido S, et al. Prognostic value of bronchiolo-alveolar carcinoma component of small lung adenocarcinoma. Ann Thorac Surg. 1999;68:2069–73.
Miller DL, Rowland CM, Deschamps C, Allen MS, Trastek VF, Pairolero PC. Surgical treatment of non-small cell lung cancer 1 cm or less in diameter. Ann Thorac Surg. 2002;73:1545–50.
Watanabe S, Oda M, Go T, Tsunezuka Y, Ohta Y, Watanabe Y, et al. Should mediastinal nodal dissection be routinely undertaken in patients with peripheral small-sized (2 cm or less) lung cancer? Retrospective analysis of 225 patients. Eur J Cardiothorac Surg. 2001;20:1007–11.
Carretta A, Canneto B, Calori G, Ceresoli GL, Campagnoli E, Arrigoni G, et al. Evaluation of radiological and pathological prognostic factors in surgically-treated patients with bronchoalveolar carcinoma. Eur J Cardiothorac Surg. 2001;20:367–71.
Okubo K, Mark EJ, Flieder D, Wain JC, Wright CD, Moncure AC, et al. Bronchoalveolar carcinoma: clinical, radiologic, and pathologic factors and survival. J Thorac Cardiovasc Surg. 1999;118:702–9.
Terasaki H, Niki T, Marsuno Y, Yamada T, Maeshima A, Asamura H, et al. Lung adenocarcinoma with mixed bronchioloalveolar and invasive components: clinicopathological features, subclassification by extent of invasive foci, and immunohistochemical characterization. Am J Surg Pathol. 2003;27:937–51.
Suzuki K, Yokose T, Yoshida J, Nishimura M, Takahashi K, Nagai K, et al. Prognostic significance of the size of central fibrosis in peripheral adenocarcinoma of the lung. Ann Thorac Surg. 2000;69:893–7.
Kuriyama K, Seto M, Kasugai T, Higashiyama M, Kido S, Sawai Y, et al. Ground-glass opacity on thin-section CT: value in differentiating subtypes of adenocarcinoma of the lung. AJR Am J Roentgenol. 1999;173:465–9.
Jang HJ, Lee KS, Kwon OJ, Rhee CH, Shim YM, Han J. Bronchioloalveolar carcinoma: focal area of ground-glass attenuation at thin-section CT as an early sign. Radiology. 1996;199:485–8.
Yap CS, Schiepers C, Fishbein MC, Phelps ME, Czernin J. FDG-PET imaging in lung cancer: how sensitive is it for bronchioloalveolar carcinoma? Eur J Nucl Med Mol Imaging. 2002;29(9):1166–73.
Acknowledgments
We thank the PET/CT technologists, nurses and PET/CT chemistry staff of Shandong Provincial Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, S., Cheng, H., Yao, S. et al. The clinical application value of PET/CT in adenocarcinoma with bronchioloalveolar carcinoma features. Ann Nucl Med 24, 541–547 (2010). https://doi.org/10.1007/s12149-010-0395-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-010-0395-5