Abstract
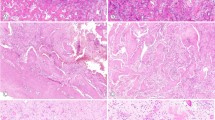
Benign fibro-osseous lesions of the craniofacial skeleton (BFOL) are a variant group of intraosseous disease processes that share similar microscopic features characterized by hypercellular fibroblastic stroma containing various combinations of bone or cementum-like tissue and other calcified structures [1–6]. Whereas some are diagnosable histologically, most require a combined assessment of clinical, microscopic and radiologic features. Some BFOL of the craniofacial complex are unique to that location whereas others are encountered in bones from other regions. Reactive, neoplastic, developmental and dysplastic pathologic processes are included under the rubric of BFOL and treatment varies from disease to disease. This review will discuss the clinical, microscopic and radiologic aspects of the more important types of BFOL of the craniofacial complex with updated information on underlying genetic and molecular pathogenic mechanisms of disease. Four main groups of BFOLs will be addressed.









Similar content being viewed by others
References
Waldron CA, Giansanti JS. Benign fibro-osseous lesions of the jaws: a clinical radiologic-histologic review of sixty-five cases I. Oral Surg Oral Med Oral Pathol. 1973;35:190–201.
Waldron CA, Giansanti JS. Benign fibro-osseous lesions of the jaws: a clinical radiologic-histologic review of sixty-five cases II. Oral Surg Oral Med Oral Pathol. 1973;35:340–50.
Hamner JE III, Scofield HH, Cornyn J (1968) Benign fibro-osseous lesions of periodontal membrane origin. An analysis of 249 cases. Cancer. 1968;22:861–78.
Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg. 1993;51(8):828–35.
El-Mofty S. Bone lesions. In: Gnepp D, editor. Diagnostic surgical pathology of the head and neck, 2nd ed. Philadelphia: Saunders, Elsevier; 2009. p. 729–84.
Eversole R, Su L, El-Mofty S. Benign fibro-osseous lesions of the craniofacial complex: a review. Head Neck Pathol. 2008;2:177–202.
Kransdorf MJ, Moser RP Jr, Gilkey FW. Fibrous dysplasia. Radiographics. 1990;10(3):519–37.
Ishida T, Dorfman HD. Massive chondroid differentiation in fibro-osseous dysplasia of bone (fibrocartilagenous dysplasia). Am J Surg Pathol. 1993;17:924–30.
Lumbroso S, Paris F, Sultan C. McCune-Albright syndrome: molecular genetics. J Pediatr Endocrinol Metab. 2002;15(Suppl 3):875–82.
Marie PJ, de Pollak C, Chanson P, et al. Increased proliferation of osteoblastic cells expressing the activating Gs alpha mutation in monostotic and polyostotic fibrous dysplasia. Am J Pathol. 1997;150:1059–69.
Marie PJ. Cellular and molecular basis of fibrous dysplasia. Histol Histopathol. 2001;16:981–8.
Lietman SA, Ding C, Levine MA. A highly sensitive polymerase chain reaction method detects activating mutations of the GNAS gene in peripheral blood cells in McCune-Albright syndrome or isolated fibrous dysplasia. J Bone Joint Surg Am. 2005;87:2489–94.
Stompro BE, Wolf P, Haghighi P. Fibrous dysplasia of bone. Am Fam Phys. 1989;39(3):179–84.
Ricalde P, Horswell BB. Craniofacial fibrous dysplasia of the fronto-orbital region: a case series and literature review. J Oral Maxillofac Surg. 2001 Feb;59(2):157–67; discussion 67–8.
Moore AT, Buncic JR, Munro IR. Fibrous dysplasia of the orbit in childhood. Clinical features and management. Ophthalmology. 1985;92(1):12–20.
Barat M, Rybak LP, Mann JL. Fibrous dysplasia masquerading as chronic maxillary sinusitis. Ear Nose Throat J. 1989 Jan;68(1):42, 4–6.
Yabut SM Jr. Kenan S, Sissons HA, Lewis MM. Malignant transformation of fibrous dysplasia. A case report and review of the literature. Clin Orthop Relat Res. 1988;228:281–9.
Huvos A. Bone tumors: diagnosis, treatment, and prognosis. 2nd ed. Philadelphia: W B Saunders; 1991.
Ruggieri P, Sim FH, Bond JR, Unni KK. Malignancies in fibrous dysplasia. Cancer. 1994;73(5):1411–24.
Slootweg P, El-Mofty S. Ossifying Fibroma. In: Barnes L, Eveson J, Reichart P, Sidronsky D, editors. Pathology and genetics head and neck tumors. Lyon: IARC Press; 2005. p. 319–20.
Eversole LR, Leider AS, Nelson K. Ossifying fibroma: a clinicopathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol. 1985;60(5):505–11.
Eversole LR, Merrell PW, Strub D. Radiographic characteristics of central ossifying fibroma. Oral Surg Oral Med Oral Pathol. 1985;59(5):522–7.
El-Mofty SK. Cemento-ossifying fibroma and benign cementoblastoma. Semin Diagn Pathol. 1999;16(4):302–7.
Pimenta FJ, Silveria LFG, Tavares GC, Silva AC, Perdigao PF, et al. HRPT2 gene alterations in ossifying fibroma of the jaws. Oral Oncol. 2006;42:735–9.
Woodard GE. Lin L, Zhang J-H, Agarwal SK, Marx SJ, Simond FS. Parafibromin, product of the hyperparathyroidism-jaw tumor syndrome gene HRPT2, regulates cyclin D1/PRAD expression. Oncogene. 2005;24:1272–6.
Toyosawa S, Yuki M, Kishino M, Ogawa Y, Ueda T, et al. Ossifying fibroma vs fibrous dysplasia of the jaws: molecular and immunological characterization. Mod Pathol. 2007;20:389–96.
Patel MM, Wilkey JF, Abdelsayed R, D’Silva N, Malchoff C, et al. Analysis of GNAS mutations in cemento-ossyfying fibroma and cemento-osseous dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:739–43.
Slootweg P, El-Mofty S. Ossifying Fibroma. In: Barnes L, Eveson J, Reichart P, Sidronsky D, editors. Pathology and genetics head and neck tumors. Lyon: IARC Press; 2005. p. 319–20.
El-Mofty S. Psammomatoid and trabecular juvenile ossifying fibroma of the craniofacial skeleton: two distinct clinicopathologic entities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(3):296–304.
Slootweg PJ, Muller H. Juvenile ossifying fibroma. Report of four cases. J Craniomaxillofac Surg. 1990;18(3):125–9.
Slootweg PJ, Panders AK, Koopmans R, Nikkels PG. Juvenile ossifying fibroma. An analysis of 33 cases with emphasis on histopathological aspects. J Oral Pathol Med. 1994;23(9):385–8.
Margo CE, Weiss A, Habal MB. Psammomatoid ossifying fibroma. Arch Ophthalmol. 1986;104(9):1347–51.
Margo CE, Ragsdale BD, Perman KI, Zimmerman LE, Sweet DE. Psammomatoid (juvenile) ossifying fibroma of the orbit. Ophthalmology. 1985;92(1):150–9.
Khoury NJ, Naffaa LN, Shabb NS, Haddad MC. Juvenile ossifying fibroma: CT and MR findings. Eur Radiol. 2002;12(Suppl 3):S109–13.
Marvel JB, Marsh MA, Catlin FI. Ossifying fibroma of the mid-face and paranasal sinuses: diagnostic and therapeutic considerations. Otolaryngol Head Neck Surg. 1991;104(6):803–8.
Summerlin DJ, Tomich CE. Focal cemento-osseous dysplasia: a clinicopathologic study of 221 cases. Oral Surg Oral Med Oral Pathol. 1994;78:611–20.
Melrose RJ, Abrams AM, Mills BG. Florid osseous dysplasia. A clinical-pathologic study of thirty-four cases. Oral Surg Oral Med Oral Pathol. 1976;41(1):62–82.
El-Mofty SK. Lesions of the head and neck. In: Wick M, Humphrey P, Ritter J, editors. Pathology of pseudoneoplastic lesions. Philadelphia: Lippincott—Raven; 1997. p. 69–96.
Mupparapu M, Singer SR, Milles M, Rinaggio J. Simultaneous presentation of focal cemento-osseous dysplasia and simple bone cyst of the mandible masquerading as a multilocular radiolucency. Dentomaxillofac Radiol. 2005;34(1):39–43.
Wakasa T, Kawai N, Aiga H, Kishi K. Management of florid cemento-osseous dysplasia of the mandible producing solitary bone cyst: report of a case. J Oral Maxillofac Surg. 2002;60(7):832–5.
Sawyer JR, Tryka AF, Bell JM, et al. Nonrandom chromosome breakpoints at Xq26 and 2q33 characterize cemento-ossifying fibromas of the orbit. Cancer. 1995;76:1853–9.
Tabareau-Delalande F, Collin C, Gomez-Brouchet A, Bouvier C, Decouvelaere A-V, et al. Chromosome 12 long arm rearrangement covering MDM2 and RASAL1 is associated with aggressive craniofacial juvenile ossifying fibroma and extracranial psammomatoid fibro-osseous lesions. Mod Pathol. 2014;. doi:10.1038/modpathol.2014.80.
Shattuck T, Valimaki S, Obara T, Gaz RD, Clark OH, et al. Somatic and germ-line mutations of HRPT2 gene in sporadic parathyroid carcinoma. N Eng J Med. 2003;349:1722–9.
Iacobone M, Masi G, Barzon L, Porzionato A, Macchi V, et al. Hyperparathyroidism-jaw tumor syndrome: a report of three large kindred. Langenbecks Arch Surg. 2009;394:817–25.
Kenneth S, Pollick H. jaw lesions in familial hyperparathyroidism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1971;31:502–10.
Rosen IB, Palmer JA. Fibro-osseous tumors of the facial skeleton in association with primary hyperparathyroidism: an endocrine syndrome r coincidence? Am J Surg. 1981;142:494–8.
Aldred MJ, Talacko AA, Savarirayan R, Murdolo V, Mills AE, et al. Dental findings in a family with hyperparathyroidism-jaw tumor syndrome and novel HPRT2 gene mutation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:212–8.
Szabo J, Heath B, Hill VM, Jackson CE, Zarbo RJ, et al. Hereditary hyperparathyroidism-jaw tumor syndrome; the endocrine tumor gene HRPT2 maps to chromosome 1q21-q31. Am J Hum Genet. 1995;56:944–50.
Warnakulasuriya S, Markwell BD, Williams DM. Familial hyperparathyroidism associated with cementifyingfibromas of the jaws in two siblings. Oral Surg Oral Med Oral Pathol. 1985;59:269–74.
Carlson AL, Smith CL. Primary hyperparathyroidism and jaw tumor syndrome; a novel mutation in HRPT2 gene. Endocr Pract. 2008;14:743–7.
Abdulla AG, O’Leary EM, Isorena JP, Diaz MFP, Yeh MW. Recurrent hyperparathyroidism and novel nonsense mutation in a patient with hyperparathyroidism-jaw tumor syndrome. Endocr Pract. 2013;19:e134–7.
Agazzi C, Belloni L. Gli odontomi duri dei mascellari contributo clinico-rontgenologico e anatomo-microscopico con particolare riguardo alle formle ad estensione e alla comparsa familiare. Arch Ital Otol. 1953;64(suppl 16):3–102.
Young SK, Markowitz R, Sullivan S, Seal TW, Hirsci R. Familial gigantiform cementoma; classification and presentation of a large pedigree. Oral Surg Oral Med Oral Pathol. 1989;68:740–747.
Abdelsayed RA, Eversole LR, Singh BS, Scarbrough FE. Gigantiform cementoma; clinicopathologic presentation of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:438–44.
Shah S, Huh KH, Yi WJ, Heo MS, Lee SS, Choi SC. Follow up findings of recurrent gigantiform cementoma of a female child. Skeletal Radiol. 2012;41:341–6.
Finical SJ, Kane WJ, Clay RP, Bite U. Familial Gigantiform cementoma. Plastic Recon Surg. 1999;103:949–54.
Tsutsumi S, Kamata N, Maruoka Y, Ando M, Tezuka O, et al. Autosomal dominant Gnathodiaphyseal dysplasia maps to chromosome11p14.3-15.1. J Bone Miner Res. 2003;18:413–8.
Marconi C, Binello PB, Badiali G, Caci E, Cusano R, et al. A novel missense mutation in ANO5/TMEM516E is causative for Gnathodiaphyseal dysplasia in a large Italian pedigree. Eur J Hum Genet. 2013;21:613–9.
Levin LS, Wright JM, Byrd DL, Greenway G, Dorst JP, et al. Osteogenesis imperfeacta with unusual skeletal lesions: report of three families. Amer J Med Genet. 1985;21:257–69.
Shibahara T, Noma H, Yamane G-Y, Hashimoto S. Large cementifying fibroma in a patient with osteogenesis imperfecta. J Oral Maxillofac Surg. 1996;54:1016–9.
Nishimora G, Haga N, Ikeuchi S, Yamaguchi T, Aoki K, Yamato M. Fragil bone syndrome associated with craniognathic fibro-osseous lesions and abnormal modeling of the tubular bones; report of two cases with review of literature. Skeletal Radiol. 1996;25:717–22.
Moshref M, Khojastch A, Kazemi B, Roudsari MV, Varshowaz M, Eslami B. Autosomal dominant gigantiform cementoma associated with bone fractures. Am J Med Genet Part A. 2008;146A:644–8.
Rossbach HC, Leston D, lacson A, Ruas E, Salazar P. Familial gigantiform cementoma with brittle bone disease, pathologic fractures, and osteosarcoma: a possible explanation of an ancient mystery. Pediatr Blood Cancer 2005;44:390–6.
Akaska Y, Nakajima T, Koyama K, Furuya K, Misuka Y. Familial cases of new systemic bone disease, hereditary gnathodiaphysial sclerosis. Nippon Seigeka Gakkai Zasshi. 1996;43:381–94.
Riminucci M, Collins MT, Corsi A, Boyde A, Murphey MD, et al. Gnathodiaphyseal dysplasia; a syndrome of fibro-osseous lesions of the jaw bones, bone fragility, and long bone bowing. J Bone Miner Res. 2001;16:1710–8.
Ahluwalia J, Ly JQ, Norman E, Costello RF Jr, Beall DP. Gnathodiaphyseal dysplasia. Clin Imag. 2007; 31:67–9.
Tsutsumi S, Kamata N, Vokes TJ, Maruoka Y, Nakakuki K, et al. The novel gene encoding transmembrane protein is mutated in gnathodiaphyseal dysplasia (GDD). Am J Hum Genet. 2004;74:1255–61.
Mizuta K, Tsutsumi S, Inoue H, Sakamoto Y, Miyataki K, et al. Molecular characterization of GDD1/TMEM16E, the gene product responsible for autosomal dominant gnathodiaphyeal dysplasia. BBRC. 2007;357:126–32.
Acknowledgments
The national and international community of Oral and Head and Neck pathologists are particularly grateful for Lewis Roy Eversole role in founding this Journal and for acting as its first co-Editor-In-Chief.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is dedicated to Lewis Roy Eversole DDS, MSD, MA: a generous teacher, dedicated scholar and esteemed colleague and friend. His vast and seminal contributions to the field of Oral and Maxillofacial Pathology and particularly to the fascinating subject of fibro-osseous lesions of the maxillofacial skeleton are acknowledged.
Rights and permissions
About this article
Cite this article
El-Mofty, S.K. Fibro-Osseous Lesions of the Craniofacial Skeleton: An Update. Head and Neck Pathol 8, 432–444 (2014). https://doi.org/10.1007/s12105-014-0590-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-014-0590-0