Abstract
Objective
To look for profile of severe malaria and contribution of vivax infection to malarial morbidity in North Indian children.
Methods
Detailed clinical, biochemical and hematological characteristics of children hospitalized with severe malaria over last 3 y were recorded. Presence of malarial parasite on peripheral smear and/or positive antigen test was considered as diagnostic for malaria.
Results
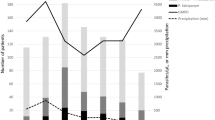
A total of 131(55.3%) patients with Plasmodium vivax (Pv), 79 (33.3%) with Plasmodium falciparum (Pf) and 27 (11.4%) with mixed infections were admitted. Cerebral malaria, severe anemia and shock were significantly more frequently observed in Pf group, while hepatic, renal, respiratory, and bleeding complications were more commonly seen in Pv patients. Malaria mortality was highest in mixed infection (11.1%), followed by Pf (7.6%) and Pv (3%) group.
Conclusions
Severe and fatal vivax malaria is an emerging recognized entity and challenges the perception of Pv as a benign disease. Further clinical studies and molecular research is required to understand emergence of severe malaria in vivax mono-infection.

Similar content being viewed by others
References
World Health Organization. Development of South-Asia Surveillance Network for Malaria Drug Resistance. Report of an informal consultative meeting, New Delhi, January 2002. WHO Project No. ICP CPC 400.
Dhingra N, Jha P, Sharma VP, et al. Adult and child malaria mortality in India: a nationally representative mortality survey. Lancet. 2010;376:1768–74.
Yadav D, Chandra J, Dutta AK. Benign Tertian malaria: how benign is it today? Ind J Pediatr 2011 Jun 25. [Epub ahead of print] PubMed PMID: 21706239.
Genton B, D’Acremont V, Rare L, et al. Pv and mixed infections are associated with severe malaria in children: a prospective cohort study from Papua New Guinea. PLos Med. 2008;5:881–9.
WHO guidelines for treatment of malaria, 2006. Downloaded from http://apps.who.int/tdr/svc/news-events/news/malaria-guidelines. Accessed on Jan 25, 2011.
Ashwani K, Neena V, Tanu J, et al. Burden of malaria in India: retrospective and prospective view. Am J Trop Med Hyg. 2007;77:69–78.
Nanda NC, Rath P, Acharya J, Mishra P, Mishra SK. Falciparum malaria in children-a brief report of 305 patients from rourkela, eastern India. Ind J Pediatr. 2011;78:475–7.
Price RN, Douglas NM, Anstey NM. New developments in Pv malaria: severe disease and chloroquin resistance. Curr Opin Infect Dis. 2009;22:430–5.
Kochar DK, Tanwar GS, Khatri PC, et al. Clinical features of children hospitalized with malaria- a study from Bikaner, northwest India. Am J Trop Med Hyg. 2010;83:981–9.
Luxemburger C, Ricci F, Nosten F, et al. The epidemiology of severe malaria in an area of low transmission in Thailand. Trans R Soc Trop Med Hyg. 1997;91:256–62.
Maitland K, Williams TN, Newbold CI. Pv and Pf: biological interactions and the possibility of cross-species immunity. Parasitol Today. 1997;13:227–31.
Tjitra E, Anstey NM, Sugiarto P, et al. Multidrug-resistant Pv malaria associated with high morbidity and mortality. PLoS Med. 2007;5:e128. doi:10.1371/journal.pmed.0050128.
Kochar DK, Das A, Kochar SK, et al. Severe Pv malaria: a report on serial cases from Bikaner in northwestern India. Am J Trop Med Hyg. 2009;80:194–8.
Anstey NM, Handojo T, Pain MC, et al. Lung injury in vivax malaria: pathophysiological evidence for pulmonary vascular sequestration and post treatment alveolar-capillary inflammation. J Infect Dis. 2007;195:589–96.
Parakh A, Agarwal N, Aggarwal A, et al. Pv malaria: uncommon manifestations. Ann Trop Pediatr. 2009;29:253–6.
Rodrıguez-Morales AJ, Sanchez E, Vargas M, et al. Anemia and thrombocytopenia in children with plasmodium vivax malaria. J Trop Pediatr. 2005;52:49–51.
Fajardo LF, Tallent C. Malarial parasites within human platelets. JAMA. 1974;229:1205–7.
Looaresuwan S, Davis JG, Allen DL, et al. Thrombocytopenia in malaria. Southeast Asian J Trop Med Public Health. 1992;23:44–50.
Yamaguchi S, Kubota T, Yamagishi T, et al. Severe thrombocytopenia suggesting immunological mechanism in two cases of vivax malaria. Am J Hematol. 1997;56:183–6.
Erel O, Vural H, Aksoy N, et al. Oxidative stress of platelets and thrombocytopenia in patients with vivax malaria. Clin Biochem. 2001;34:341–4.
Conflict of Interest
None.
Role of Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yadav, D., Chandra, J., Aneja, S. et al. Changing Profile of Severe Malaria in North Indian Children. Indian J Pediatr 79, 483–487 (2012). https://doi.org/10.1007/s12098-011-0603-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-011-0603-x