Abstract
Objective
To evaluate the role of Unsynchronized Nasal Intermittent Positive Pressure Ventilation (NIPPV) in prevention of extubation failure in mechanically ventilated preterm neonates weighing less than 2,000 g.
Methods
This randomized controlled trial was conducted in the neonatal intensive care unit of a tertiary care teaching hospital. Preterm neonates weighing less than 2,000 g, mechanically ventilated for more than 24 h were included after extubation. Neonates were randomized into two groups. Group 1 was given unsynchronized nasal intermittent positive pressure ventilation with shortened endotracheal tube by ventilator and Group 2 was given head box oxygen, fraction of oxygen in inspired air was 50%. Primary outcome variable was rate of extubation failure within 72 h of extubation.
Results
Birth weight, gestational age, age at intubation, indication for mechanical ventilation and antenatal details were comparable in the two groups. Extubation failure rate was 16% in Group1 vs 63% in Group 2 (RR = 0.25; 95% CI: 0.12, 0.51, p value = 0.00), that is a reduction of 47%. Unsynchronized nasal intermittent positive pressure ventilation did not have any serious side effects, however it did not reduce total hospital stay.
Conclusions
Unsynchronized Nasal Intermittent Positive Pressure Ventilation is a simple technique of noninvasive ventilation which significantly reduces the rate of extubation failure in preterm neonates and is not associated with serious side effects.
Similar content being viewed by others
Introduction
Almost 50% of very low birth weight (LBW) babies require re-intubation and ventilation after being weaned off from the ventilator [1]. Neonatal CPAP has been established as an effective bridge between ventilation and unassisted breathing, but special equipment and prongs are required for this. Studies have shown that 25–40% of LBW neonates fail to be extubated even to CPAP [2]. Efforts to reduce re-intubation led to the use of other techniques like Nasal Intermittent Positive Pressure Ventilation (NIPPV) which involves augmentation of CPAP with superimposed inflations at a set peak pressure. Earlier, unsynchronized NIPPV was used for preventing post extubation failure, but some workers reported occasional gastrointestinal perforation [3]. These studies, however, were uncontrolled. Recent studies have shown about 30% reduction in extubation failure in neonates receiving synchronized NIPPV as compared to CPAP [4]. But for synchronized NIPPV, special expensive equipment like Star sync capsule is required [4]. These were not available in the present setup. The authors, therefore, set out to evaluate the role of unsynchronized NIPPV, for which no additional equipment was required, to prevent extubation failure in preterm neonates weighing less than 2,000 g.
Material and Methods
This randomized controlled trial was conducted over a period of 1 year from August 2007 through July 2008 at the Neonatal intensive care unit of a tertiary care teaching hospital. All preterm neonates weighing less than 2,000 g, given mechanical ventilation for more than 24 h and extubated before 4 week of age were included in the study. The time of enrolment was 6 h prior to extubation. Written informed consent for the study was taken from the parents of the enrolled neonates prior to the randomization. Neonates with major congenital abnormalities and whose parents did not give consent were excluded and not randomized. Neonates were extubated once they were maintaining saturation (SpO2) of 92–96% on a FiO2 of <0.4, on a ventilator rate of ≤12 breaths per min, peak inspiratory pressure (PIP) of ≤14 cm of water and a positive end expiratory pressure (PEEP) of ≤4 cm of water and having a hemoglobin (Hb) of >13 gm% [4]. All neonates were given a loading dose of intravenous aminophylline at 6 mg/kg, before extubation followed by a maintenance dose of 2 mg/kg every 8 h. The random treatment assignment was placed in serially numbered opaque ang sealed envelopes. Neonates were randomly assigned either to Group1 (NIPPV) or Group 2 (O2 by headbox). Demographic details, initial diagnosis at admission, gestational age, birth weight, indication of mechanical ventilation were recorded for all the study subjects at the time of inclusion. Neonates randomized to NIPPV received it using appropriate size endotracheal tube (ET) cut short to a length equal to the horizontal distance between the tip of nose and a vertical line passing through centre of the eyeball. The shortened ET was inserted in one nostril and positive pressure given via the ventilator (Drager Babylog 8000plus/ Newport/ SLE/ Digivent) in the IMV mode at the same rate as before extubation.
PIP was increased by 2 cm of water above the pre extubation PIP, a PEEP of 5 cm of water and a FiO2 of 0.5 was given [5]. Neonates in Group2 were given O2 by headbox on a FiO2 of 0.5 the flow rate being 8–10 L/min in NIPPV group and 2–3 L/min in O2 by headbox group.
Monitoring during the study period of 72 hours
The respiratory status of neonates was assessed clinically and by blood gas analysis done 1–3 h after extubation, as is routine in the present NICU. Thereafter, blood gases were obtained as clinically indicated, but at least every 12 h in the first 24 h post extubation, then every 24 h for 48 h. In Group1, NIPPV was discontinued once the neonates were stable at minimum settings [PIP 14 cm of H2O, PEEP 5 cm of H2O, rate-12, FiO2–0.3] for 12 h. Neonates in Group 2 received decreasing FiO2 levels if they were maintaining SpO2 and oxygen by head box was removed when they were stable at a FiO2 of 0.3. In both the groups, the FiO2 was gradually increased to 0.6 in an effort to maintain a SpO2 of 92–96%, if required.
Criteria for reintubation during study period (within 72 h of extubation)
pH <7.25, PaCO2 >60 mm Hg, single episode of apnea needing bag and mask resuscitation, frequent (>3 per h) apnea/bradycardia spells (cessation of respiration for >20 s associated with a heart rate of <100/min), frequent desaturation (SpO2 <85%) of >3 episodes /hour not responding to increased ventilator settings or an increase in FiO2 to 0.6, and a PaO2 <50 mm Hg despite a FiO2 of 0.6. The end point of the study was that after 72 h of study period; neonate was weaned off from NIPPV or oxygen by headbox or was reintubated i.e. developed extubation failure. The neonates were fed by bolus feedings every 2 h by nasogastric tube. Gastric aspirates were measured every 2 h. If the volume of gastric aspirate was >20% of the previous feed volume, then the next feed was withheld, particularly if accompanied by abdominal distension.
In all the study subjects hemoglobin, complete blood count, chest radiograph, ET tip culture, blood culture was done on the day of extubation as is routine in the present unit.
Primary outcome was the rate of extubation failure in the two groups. Secondary outcomes were side effects of unsynchronized NIPPV and comparison of duration of hospital stay in neonates in the two groups.
Statistical Methods
The data were described as proportion and mean±SD. χ2 statistics was applied to test the association between two categorical variables. The means between the groups were compared by two sample t-test, if data was normally distributed, otherwise their non-parametric equivalent test, Mann Whitney test, was applied. Data was analyzed using Stata 9.2 statistical software (College Station, Texas, USA) package and the difference was considered to be significant if ‘p’ value was found to be <0.05.
The study was approved by the Institutional Review Board of Department of Pediatrics,CSMMU, Lucknow.
Sample Size
To test a hypothesis of 30%( according to Barrington (4)14.8% neonates failed extubation in nSIMV group as compared to 44.4% on nCPAP) reduction in extubation failure rate in NIPPV group than that of in Oxygen by head box group with a power of 80%, confidence level of 95% and assuming that there is 45% extubation failure rate in Oxygen by head box group, 42 subjects in each group were required. Considering 5% drop out rate, 45 patients in each group were required to be enrolled.
Results
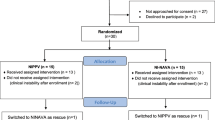
During the study period 94 preterm neonates weighing less than 2,000 g, who were ventilated for more than 24 h and extubated before 4 weeks of age, were considered for enrollment. Two neonates had major congenital malformations (tracheo esophageal fistula and meningomyelocele), while the parents of two did not give consent. As seen in Fig. 1, 90 neonates were enrolled in the study. None of the neonates in the RCT died or left against medical advice during the study period of 72 h. After the observation period of 72 h, 6 (16.2%) neonates expired as compared to 12 (31.6%) in ‘O2 by headbox’ group. Fifteen patients (9 from NIPPV group and 6 from O2 by headbox’ group) left against medical advice after the study period of 72 h.
The salient baseline demographic and clinical details of the patients of the two groups are shown in Table 1. The two groups were well matched in terms of demographic and clinical variables except for the duration of mechanical ventilation. Duration of mechanical ventilation was longer in Group1 (NIPPV group) (106.5 ± 89.8 h) as compared to 80.2 ± 73 h (p = 0.01).
Outcome
Extubation Failure
As shown in Table 2, out of 45 neonates in NIPPV Group, 38(84.4%) were extubated successfully, while 7 (15.6%) failed extubation i.e. had to be reintubated within 72 h. In the ‘O2 by headbox’ group, only 17(37.8%) neonates could be extubated successfully and 28 (63.2%) failed extubation. The difference was found to be statistically significant (RR = 0.25; 95% CI: 0.12, 0.51, p value = 0.00).
On reviewing the Arterial blood gas of the study patients, out of seven neonates who failed extubation in NIPPV group, hypercapnia with respiratory acidosis was found in 6(85.7%)neonates, and hypoxemia in 4(57.1%)neonates. In ‘O2 by headbox’ group, 28 neonates failed extubation and the incidence of respiratory acidosis and hypoxemia was found to be 10 (39.2%) and 12(42.8%), respectively. None of the neonates in the NIPPV group developed hyperoxia and hypocarbia.
The incidence of late intubation (>72 h) in NIPPV group was 15.7% as compared to 17.6% in ‘02 by headbox’ group. The difference was not statistically significant (p = 0.29).
Side Effects of Unsynchronized NIPPV
Agitation was found in four neonates in Group 1 and none in Group 2. The difference was statistically significant (p = 0.04). Minor nasal trauma was found in four neonates in Group 1 and in none of the neonates in Group 2 and was significantly increased (p = 0.04). Feeding intolerance was noted in 13 neonates in Group 1 and nine neonates in Group 2 (p = 0.32). No case of gastrointestinal perforation was noted. One patient in NIPPV group developed pneumothorax.
Duration of Hospital Stay
The Median of duration of hospital stay in NIPPV group was 16 days against 20 days in ‘O2 by headbox’ group. NIPPV is associated with a shorter duration of hospital stay than O2 by headbox’ group but difference was not statistically significant (p value = 0.467).
Discussion
The present study clearly demonstrates that unsynchronized NIPPV is a good modality to prevent extubation failure in preterm babies. The authors found extubation failure rate of 16% in low birth weight neonates extubated to NIPPV vs 63% in those given head box oxygen after extubation, that is, a reduction of 47%. This is attributed to lower incidence of apnea and hypercarbia in the NIPPV group. The study patients were well matched in terms of birth weight, gestational age, age at intubation, indication for ventilation and antenatal details. Only one factor which remained unmatched was the duration of mechanical ventilation which was significantly longer in NIPPV group (p = 0.01). As prolonged duration of mechanical ventilation is associated with a higher risk of extubation failure, the rate of successful extubation could have been even higher if this wouldn’t have been the case.
On searching the available literature, the authors could not find any studies comparing unsynchronized NIPPV with head box oxygen. In a study comparing nasal continuous positive airway pressure (NCPAP) vs oxyhood following extubation of neonates weighing less than 1 kg, results demonstrated that 22 (76%) of 29 neonates were successfully extubated to NCPAP while only 6 (21%) of 29 were successfully extubated to oxyhood (P < .0001) [6]. In a Cochrane meta analysis which included three randomized control trials, comparing synchronized NIPPV with NCPAP there was a reduction of 30–34% in extubation failure rate in the NIPPV group [2] and numbers needed to prevent 1 extubation failure were 3. In the present study, the numbers needed to prevent 1 extubation failure were 2.
Most workers have found post extubation NIPPV to be a better choice as compared to CPAP and CPAP has been found to be better than ‘Oxygen by headbox” [2, 4, 7, 8]. Barrington et al (2001); conducted a study comparing efficacy of nasal SIMV vs nCPAP in preventing extubation failure in infants weighing <1,250 g. 14.8% neonates failed extubation in nSIMV group as compared to 44.4% on nCPAP and the difference was significant (p value <0.05). This was attributed to lower incidence of apnea and hypercarbia in the nSIMV group [4].
In the present study, the incidence of apnea within 72 h of extubation in NIPPV group was 9% (four out of 45 neonates had apnoea) whereas in Oxygen by headbox group it was 22.2% (ten out of 45). The difference was found to be statistically insignificant (p value = 0.37). Similar observations were made by two other workers [9, 10].There are two studies which demonstrated statistically significant reduction in the incidence of apnea with synchronized NIPPV [4, 11].
One of the secondary objectives of the present study was to detect the side effects of unsynchronized NIPPV. Minor side effects in the form of nasal trauma and agitation were found to be commoner in patients in the NIPPV group. No case of gastrointestinal perforation was noted. This was comparable to earlier studies [4, 10, 12]. The increased incidence of agitation in the present study may be because of unsynchronized delivery of breaths, whereas in the other studies NIPPV was synchronized. The increased incidence of nasal trauma could be because of the nature of the improvised nasal prongs that were used. This nasal trauma was mild and did not require any specific therapy other than changing the side of the nostril with ET insertion.
In the present study, the mean duration of hospital stay in NIPPV group (20.6 days) was shorter than Oxygen by headbox group (22.5 days) but the difference was not significant (p value = 0.46). The present findings were like those of Barrington et al [4] who reported a mean duration of hospital stay of 92 days in nCPAP group and 86 days in nSIMV group, and Khalaf et al [10] who reported the length of stay in the nasal synchronized intermittent positive pressure ventilation (NSIPPV) group to be 72 days and in nCPAP group 76 days (p value = 0.72). The longer duration of hospital stay in these studies is probably because of lower gestational age of the neonates enrolled as compared to that in the present study. Hesham Abdel-Hady et al also showed that extubating preterm newborns to NIPPV did not shorten the length of hospital stay [(13.2 days in NIPPV vs15.20 days in NCPAP) (p value = 0.34)] [12].
The authors demonstrated in this study that NIPPV did not affect the incidence of late intubation (after 72 h post extubation) in neonates who were extubated successfully earlier. Late intubation was required in 6(15.7%) of neonates in NIPPV group and 3 (17.6%) neonates in O2 by headbox group. These findings were similar to the study conducted by Hesham Abdel-Hady et al in which 3 (15%) neonates were reintubated after 72 h in nCPAP group and 2(10%) were intubated in NIPPV group (p value = 0.66) [12]. Similar observations were made by the study done by Khalaf et al [10].
Thus, the present study confirms that ventilated preterm neonates should be kept on unsynchronized NIPPV post extubation to prevent extubation failure. The shortened ET is inexpensive and easily available. The side effects due to unsynchronized NIPPV are trivial and of not much consequence.
Strength of the present study is that it is a randomized controlled trial where the two prongs of the trial were well matched. The major limitations of this study is that authors have not compared unsynchronized NIPPV with nasal CPAP.But this was not possible because nasal CPAP prongs are expensive and were not easily available in the present setup.
Conclusions
Unsynchronized NIPPV is a simple technique of noninvasive ventilation for neonates, which significantly reduces the rate of extubation failure in preterm neonates. It is not associated with any serious side effects but does not shorten the duration of hospital stay.
References
Annibale DJ, Hulsey TC, Engstrom PC. Randomized, controlled trial of nasopharyngeal continuous positive airway pressure in the extubation of very birth weight infants. J Pediatric. 1994;124:455–60.
Davis PG, Henderson-Smart DJ. Nasal continuous positive airways pressure immediately after extubation for preventing morbidity in preterm infants. Cochrane Database Syst Rev. 2003;2:CD000143.
Garland JS, Nelson DB, Rice T, et al. Increased risk of gastrointestinal perforations in neonates mechanically ventilated with either face mask or nasal prongs. Pediatrics. 1985;76:406–10.
Barrington KJ, Bull D, Finer NN, et al. Randomized trial of nasal synchronized intermittent mandatory ventilation compared with continuous positive airway pressure after extubation of very low birth weight infants. Pediatrics. 2001;107:638–41.
Jackson JK, Vellucci J, Johnson P, et al. Evidence-based approach to change in clinical practice: introduction of expanded nasal continuous positive airway pressure use in an intensive care nursery. Pediatrics. 2003;111:e542–7.
Higgins RD, Richter SE, Davis JM. Nasal continuous positive airway pressure facilitates extubation of very low birth weight neonates. Pediatrics. 1991;88:999–1003.
Kulkarni A, Ehrenkranz RA, Bhandari V, et al. Effect of introduction of synchronized nasal intermittent positive-pressure ventilation in a neonatal intensive care unit on bronchopulmonary dysplasia and growth in preterm infants. Am J Perinatol. 2006;23:1–8.
Friedlich P, Lecart C, Posen R, et al. A randomized trial of nasopharyngeal synchronized intermittent mandatory ventilation versus nasopharyngeal continuous positive airway pressure in very low birth weight infants after extubation. J Perinatol. 1999;19:413–8.
Ryan CA, Finer NN, Peters KL, et al. Nasal intermittent positive-pressure ventilation offers no advantages over nasal continuous positive airway pressure in apnea of prematurity. Am J Dis Child. 1989;143:1196–8.
Khalaf MN, Brodsky N, Hurley J, et al. A prospective randomized, controlled trial comparing synchronized nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure as modes of extubation. Pediatrics. 2001;108:13–7.
Lin CH, Wang ST, Lin YJ, et al. Efficacy of nasal intermittent positive pressure ventilation in treating apnea of prematurity. Pediatr Pulmonol. 1998;26:349–53.
www.esnpc.org/congress/NIPPV-Gona.ppt Non-Synchronized Nasal Intermittent Positive Pressure Ventilation (NIPPV) versus Nasal Continuous Positive Airway Pressure (NCPAP) As Modes of Extubation in Preterm Neonates by Hesham Abdel Hady accessed on 14/9/2008.
Contributions
MK; Designed the study, helped in patient management, analyzed the data and edited the manuscript, SAv; Helped in designing the study, management of patients and writing the manuscript,SAh; collected the data, analyzed it and wrote the manuscript,GKM, Helped in designing the study and management of patients,SNS; Helped in designing the study and management of patients.
Conflict of Interest
None.
Role of Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s12098-011-0563-1
Rights and permissions
About this article
Cite this article
Kumar, M., Avasthi, S., Ahuja, S. et al. Unsynchronized Nasal Intermittent Positive Pressure Ventilation to Prevent Extubation Failure in Neonates: A Randomized Controlled Trial. Indian J Pediatr 78, 801–806 (2011). https://doi.org/10.1007/s12098-010-0357-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-010-0357-x