Abstract
Objective
To study the clinical profile, socio-demographic features, psychosocial stressors and outcome of somatoform disorders in children
Methods
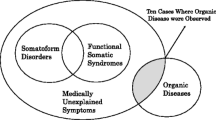
Children up to the age of 18 year presenting with unexplained physical symptoms over a period of 6 months were evaluated. A detailed history and physical examination was carried out. Appropriate investigations were undertaken to exclude organic causes. Diagnosis was made according to DSM-IV-TR criteria.
Results
Forty-five children were diagnosed with somatoform disorders during the study period. The prevalence was 0.5% and 0.9% among outdoor and indoor patients, respectively. Conversion disorder (48.9%) was the commonest followed by other somatoform disorders (26.7%). Pseudoseizures and fainting attacks in conversion disorder and pain abdomen and general body pain in somatoform disorder were the commonest symptoms. Male to female ratio was 2.2:1. Urban children (25) were represented more than rural children (20). Stress factors were identified in 71.1% patients, which included fear of school or examinations. Thirty-three patients (73.3%) remained asymptomatic after counseling whereas, 8 patients (17.6%) had relapse requiring further counseling. Four patients (8.8%) showed no improvement and needed psychiatric evaluation.
Conclusions
Early referral to mental health professional is required to avoid unnecessary investigations and delay in diagnosis of somatoform disorders in children.
Similar content being viewed by others
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington DC: APA; 2000. p. 485–511.
Ghosh JK, Majumder P, Pant P, Dutta R, Bhatia BD. Clinical profile and outcome of conversion disorder in a tertiary hospital of India. J Trop Pediatr. 2007;53:213–4.
Steffanson JG, Messina JA, Meyerowitz S. Hysterical neurosis, conversion type: clinical and epidemiological consideration. Acta Psychiatr Scand. 1976;53:110–38.
Mishra D, Singh HP. Kuppuswami’s socioeconomic status scale: a revision. Indian J Pediatr. 2003;70:273–4.
Bisht J, Sankhyan N, Kaushal RK, Sharma RC, Grover N. Clinical profile of pediatric somatoform disorders. Indian Pediatr. 2008;45:11–5.
Pehlivanturk B, Unal F. Conversion disorder in children and adolescents: a 4-year follow up study. J Psychosom Res. 2002;52:187–91.
Chaudhury S, Prasad PL, Zacharias R, Madhusudan T, Saini R. Psychiatric morbidity pattern in a Child Guidance clinic. Med J Armed Forces India. 2007;63:144–6.
Malhi P, Singhi P. Clinical characteristics and outcome of children and adolescents with conversion disorder. Indian Pediatr. 2002;39:747–52.
Rock NL. Conversion reactions in childhood: a clinical study on child neurosis. Ann Acad Child Adolesc Psychiatr. 1971;10:65–94.
Sharma I, Giri D, Dutta A, Mazumdar P. Psychological factors in children and adolescents with conversion disorder. J Indian Assoc Child Adolesc Ment Health. 2005;1:3–8.
Malhotra S, Singh G, Mohan A. Somatoform and dissociative disorders in children and adolescents: a comparative study. Indian J Psychiatr. 2005;47:39–43.
Leary PM. Conversion disorders in childhood—diagnosed too late, investigated too much? J R Soc Med. 2003;96:436–8.
Hurwitz TA. Somatization and conversion disorder. Can J Psychiatry. 2004;49:172–8.
Tocchio SL. Treatment of conversion disorder: A clinical and holistic approach. J Psychosoc Nurs Ment Health Serv. 2009;47:42–9.
Sitholey P, Agarwal V. Clinical practice guidelines for the management of pediatric somatoform disorders. Indian J Psychiatry. 2008;50:151–6.
Contributions
VG planned and designed the study. AS collected the data. SU helped in manuscript writing. BDB will act as guarantor for the paper.
Conflict of Interest
None.
Role of Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gupta, V., Singh, A., Upadhyay, S. et al. Clinical Profile of Somatoform Disorders in Children. Indian J Pediatr 78, 283–286 (2011). https://doi.org/10.1007/s12098-010-0282-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-010-0282-z