Abstract
Objective
To find out the efficacy of continuous fetal heart monitoring by analyzing the cases of cesarean section for nonreassuring fetal heart in labor, detected by cardiotocography (CTG) and correlating these cases with perinatal outcome. To evaluate whether a 30 minute decision to delivery (D-D) interval for emergency cesarean section influences perinatal outcome.
Methods
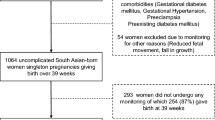
This was a prospective observational study of 217 patients who underwent cesarean section at ≥ 36 weeks for non-reassuring fetal heart in labor detected by CTG. The maternal demographic profile, specific types of abnormal fetal heart rate tracing and the decision to delivery time interval were noted. The adverse immediate neonatal outcomes in terms of Apgar score <7 at 5 minutes, umbilical cord þH <7.10, neonates requiring immediate ventilation and NICU admissions were recorded. The correlation between non-reassuring fetal heart, decision to delivery interval and neonatal outcome were analyzed.
Results
Out of 3148 patients delivered at ≥ 36 weeks, 217 (6.8%) patients underwent cesarean section during labor primarily for non-reassuring fetal heart. The most common fetal heart abnormality was persistent bradycardia in 106 (48.8%) cases followed by late deceleration in 38 (17.5%) cases and decreased beat to beat variability in 17 (7.8%) cases. In 33 (15.2%) babies the 5 minutes Apgar score was <7 out of which 13 (5.9%) babies had cord þH <7.10. Thirty three (15.2%) babies required NICU admission for suspected birth asphyxia. Rest 184 (84.7%) neonates were born healthy and cared for by mother. Regarding decision to delivery interval of ≤30 minutes versus >30 minutes, there was no significant difference in the incidence of Apgar score <7 at 5 minutes, cord pH <7.10 and new born babies requiring immediate ventilation. But the need for admission to NICU in the group of D-D interval ≤ 30 minutes was significantly higher compared to the other group where D-D interval was >30 minutes.
Conclusion
Non-reassuring fetal heart rate detected by CTG did not correlate well with adverse neonatal outcome. There was no significant difference in immediate adverse neonatal outcome whether the D-D time interval was ≤ 30 minutes or >30 minutes; contrary to this, NICU admission for suspected birth asphyxia in ≤ 30 minutes group was significantly higher.
Similar content being viewed by others
References
Hornbuckle J, Vail A, Abrans KR, Thornton JG. Bayesian interpretation of trials: the example of intrapartum electronic fetal heart rate monitoring. Br J Obstet Gynaecol 2000; 107: 3–10.
Olofsson P. Current status of intrapartum fetal monitoring: cardiotocography versus cardiotocography + ST analysis of the fetal ECG. Eur J Obstet Gynaecol Rep Biol 2003; 110: S113–S118.
Nielson JP, Grant AM. The randomized trails of intrapartum electronic fetal monitoring. In Spencer JA, Ward RH, eds. Intrapartum fetal surveillance. London; RCOG Press, 1993.
American college of Obstetricians and Gynecologists: Guidelines for Vaginal Delivery after a Previous Cesarean Birth, ACOG Committee Opinion No. 64. Washington; DC, ACOG, 1988.
Onah EE, Ibeziako N, Umezulike AC, Effetie ER, Ogboukiri CM. Decision - delivery interval and perinatal outcome in emergency caesarean sections. J Obstet Gynaecol 2005; 25: 342–346.
Dwyer JP. Decision to delivery time in emergency caesarean section. Proceedings of Fourth International Scientific Meeting of the RCOG. London; Royal College of Obstetricians and Gynaecologists 1999.
Tufnell DJ, Wilkinson K, Beresford N. Interval between decision and delivery by caesarean section -are current standards achievable? Observational case series. BMJ 2001; 322: 1330–1333.
Chauhan SP, Magann EF, Scott JR, Scardo JA, Hendrix NW, Martin JN Jr. Emergency cesarean delivery for nonreassuring fetal heart rate tracings: compliance with ACOG Guidelines. J Rep Med 2003; 48: 975–981.
Chauhan SP, Roach H, Naef RW, Magann EF, Morrison JC, Martin JN Jr. Cesarean section for suspected fetal distress. Does the decision-incision time make a difference? J Rep Med 1997; 42: 347–352.
Dunphy BC, Robinson JN, Sheil OM, Nicholls JSD, Gillmer MDG. Cesarean section for fetal distress, the interval from decision to delivery and the relative risk of poor neonatal condition. J Obstet Gynecol 1991; 11: 241–244.
Wareham V, Bain C, Cruickshank D. Caesarean section audit by peer review. Eur J Obstet Gynecol Rep Biol 1993; 48: 9–14.
Dellinger EH, Boehm FH, Crane MM. Electronic fetal heart rate monitoring: Early neonatal outcomes associated with normal rate, fetal stress, and fetal distress. Am J Obstet Gynecol 2000; 182: 214–220.
Shiono PH, McNellis D, Rhoads GG. Reasons for the rising cesarean delivery rates: 1978–1984. Obstet Gynecol 1987; 69: 696–700.
Nelson KR, Dambrosia JM, Ting TY Grether JK. Uncertain value of electronic fetal monitoring in predicting cerebral palsy. The New England J of Med 1996; 334: 613–617.
Wijngaarden WJ V, Sahota DS, James DK, Farrell T, Mires GJ, Wilcox M, Chang A. Improved intrapartum surveillance with PR interval analysis of the fetal electrocardiogram: A randomized trial showing a reduction in fetal blood sampling. Am J Obstet Gynecol 1996; 174: 1295–1462.
Chawla R, Deppe G, Ahart S, Gleicher N. Hemorrhage after fetal blood sampling. Am J Obstet Gynecol 1984; 149–192.
Reed NN, Mohajer MP, Sahota DS, James DK, Symonds EM. The potential impact of PR interval analysis of the fetal electrocardiogram (FECG) on intrapartum fetal monitoring. Eur J Obstet Gynecol Rep Biol 1996; 86: 87–92.
Wijngarden WJ V, Strachan BK, Sahota DS, James DK. Improving intrapartum surveillance: an individualized T/QRS ratio? Eur J Obstet Gynecol Rep Biol 2000; 88: 43–48.
Vayssiere C, Haberstich R, Sebahoun V, David E, Roth E, Langer B. Fetal electrocardiogram ST-segment analysis and prediction of neonatal acidosis. Int J Obstet Gynecol 2007; 97: 110–114.
Schauberger CW, Rooney BL, Beguin EA, Schaper AM, Spindler J. Evaluating the 30 minute interval in emergency caesarean sections. Am J Surg 1994; 179: 151–155.
Bloom SL, Leveno Kenneth, Spong CY et al. Decision to incision times and maternal and infant outcomes. Obstet & Gynecol 2006; 108: 6–11
Helmy WH, Jolaoso AS, Ifaturoti OO, Afify SA, Jones MH. The decision to delivery interval for emergency caesarean section: is 30 minutes a realistic target? BJOG 2002; 109: 505–508.
MacKenzie IZ, Cooke I. What is a reasonable time from decision to delivery by caesarean section? Evidence from 415 deliveries. BJOG 2002; 109: 498–504.
Mackenzie IZ, Cooke I. Prospective 12 months study of 30 minute decision to delivery interval for ‘emergency’ caesarean section. BMJ 2001; 322: 1334–1335
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roy, K., Baruah, J., Kumar, S. et al. Cesarean section for suspected fetal distress, continuous fetal heart monitoring and decision to delivery time. Indian J Pediatr 75, 1249–1252 (2008). https://doi.org/10.1007/s12098-008-0245-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-008-0245-9