Abstract
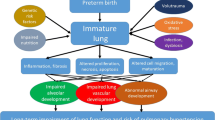
Bronchopulmonary dysplasia (BPD) is a chronic lung disease associated with premature birth and characterized by early lung injury. Over the past 4 decades, there have been significant changes in its definition, pathology and radiological findings as well as management of BPD. Management of the acute phase and later stages of this lung disease continue to evolve. Use of non-invasive ventilatory techniques, recombinant human SOD and CC10 and inhaled NO are some novel approaches that are being studied. Adequate nutrition is vital to optimize lung growth and repair. The widely accepted practice of prophylaxis against viral infections has markedly decreased the rates of rehospitalization. Infants with BPD, however, continue to have significant pulmonary and neurodevelopmental sequelae. Unraveling the genetic contribution to BPD will potentially pave the way to improved preventive and therapeutic approaches.
Similar content being viewed by others
References
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001; 163: 17231729.
Northway WH, Jr., Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med 1967; 276: 357368.
Ehrenkranz RA, Walsh MC, Vohr BR et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 2005; 116: 13531360.
Rosan RC. Hyaline membrane disease and a related spectrum of neonatal pneumopathies. Perspect Pediatr Pathol 1975; 2: 1560.
Stocker JT. Pathologic features of long-standing healed bronchopulmonary dysplasia: a study of 28 3-to 40-month-old infants. Hum Pathol 1986; 17: 943961.
Husain AN, Siddiqui NH, Stocker JT. Pathology of arrested acinar development in postsurfactant bronchopulmonary dysplasia. Hum Pathol 1998; 29: 710717.
De Paepe ME, Mao Q, Powell J et al. Growth of pulmonary microvasculature in ventilated preterm infants. Am J Respir Crit Care Med 2006; 173: 204211.
Coalson JJ. Pathology of new bronchopulmonary dysplasia. Semin Neonatol 2003; 8: 7381.
Thibeault DW, Mabry SM, Norberg M, Truog WE, Ekekezie, II. Lung microvascular adaptation in infants with chronic lung disease. Biol Neonate 2004; 85: 273282.
Bhandari A, Bhandari V. Pathogenesis, pathology and pathophysiology of pulmonary sequelae of bronchopulmonary dysplasia in premature infants. Front Biosci 2003; 8: e370380.
Bhandari V, Bizzarro MJ, Shetty AH et al. Familial and genetic susceptibility to major neonatal morbidities in preterm twins. Pediatrics 2006; 117: 19011906.
Furman L, Baley J, Borawski-Clark E, Aucott S, Hack M. Hospitalization as a measure of morbidity among very low birth weight infants with chronic lung disease. J Pediatr 1996; 128: 447452.
Northway WH, Jr., Moss RB, Carlisle KB et al. Late pulmonary sequelae of bronchopulmonary dysplasia. N Engl J Med 1990; 323: 17931799.
Aquino SL, Schechter MS, Chiles C, Ablin DS, Chipps B, Webb WR. High-resolution inspiratory and expiratory CT in older children and adults with bronchopulmonary dysplasia. AJR Am J Roentgenol 1999; 173: 963967.
Baraldi E, Filippone M, Trevisanuto D, Zanardo V, Zacchello F. Pulmonary function until two years of life in infants with bronchopulmonary dysplasia. Am J Respir Crit Care Med 1997; 155: 149155.
Mitchell SH, Teague WG. Reduced gas transfer at rest and during exercise in school-age survivors of bronchopulmonary dysplasia. Am J Respir Crit Care Med 1998; 157: 14061412.
Santuz P, Baraldi E, Zaramella P, Filippone M, Zacchello F. Factors limiting exercise performance in long-term survivors of bronchopulmonary dysplasia. Am J Respir Crit Care Med 1995; 152: 12841289.
Short EJ, Klein NK, Lewis BA et al. Cognitive and academic consequences of bronchopulmonary dysplasia and very low birth weight: 8-year-old outcomes. Pediatrics 2003; 112: e359.
Lewis BA, Singer LT, Fulton S et al. Speech and language outcomes of children with bronchopulmonary dysplasia. J Commun Disord 2002; 35: 393406.
Verder H, Albertsen P, Ebbesen F et al. Nasal continuous positive airway pressure and early surfactant therapy for respiratory distress syndrome in newborns of less than 30 weeks gestation. Pediatrics 1999; 103: E24.
Khalaf MN, Brodsky N, Hurley J, Bhandari V. A prospective randomized, controlled trial comparing synchronized nasal intermittent positive pressure ventilation versus nasal continuous positive airway pressure as modes of extubation. Pediatrics 2001; 108: 137.
Santin R, Brodsky N, Bhandari V. A prospective observational pilot study of synchronized nasal intermittent positive pressure ventilation (SNIPPV) as a primary mode of ventilation in infants > or = 28 weeks with respiratory distress syndrome (RDS). J Perinatol 2004; 24: 487493.
Mestan KK, Marks JD, Hecox K, Huo D, Schreiber MD. Neurodevelopmental outcomes of premature infants treated with inhaled nitric oxide. N Engl J Med 2005; 353: 2332.
Schreiber MD, Gin-Mestan K, Marks JD, Huo D, Lee G, Srisuparp P. Inhaled nitric oxide in premature infants with the respiratory distress syndrome. N Engl J Med 2003; 349: 2099107.
Field D, Elbourne D, Truesdale A et al. Neonatal Ventilation With Inhaled Nitric Oxide Versus Ventilatory Support Without Inhaled Nitric Oxide for Preterm Infants With Severe Respiratory Failure: the INNOVO multicentre randomised controlled trial (ISRCTN 17821339). Pediatr 2005; 115: 926936.
Hascoet JM, Fresson J, Claris O et al. The safety and efficacy of nitric oxide therapy in premature infants. J Pediatr 2005; 146: 31823.
Davis JM, Rosenfeld WN, Richter SE et al. Safety and pharmacokinetics of multiple doses of recombinant human CuZn superoxide dismutase administered intratracheally to premature neonates with respiratory distress syndrome. Pediatrics 1997; 100: 2430.
Davis JM, Parad RB, Michele T, Allred E, Price A, Rosenfeld W. Pulmonary outcome at 1 year corrected age in premature infants treated at birth with recombinant human CuZn superoxide dismutase. Pediatrics 2003; 111: 469476.
Levine CR, Gewolb IH, Allen K et al. The safety, pharmacokinetics, and anti-inflammatory effects of intratracheal recombinant human Clara cell protein in premature infants with respiratory distress syndrome. Pediatr Res 2005; 58: 1521.
Dodd JM, Crowther CA, Cincotta R, Flenady V, Robinson JS. Progesterone supplementation for preventing preterm birth: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 2005; 84: 526533.
Akram Khan M, Kuzma-Oreilly B, Brodsky NL, Bhandari V. Site-specific characteristics of infants developing bronchopulmonary dysplasia. J Perinatol 2006; 26: 428435.
Kulkarni A, Ehrenkranz RA, Bhandari V. Effect of introduction of synchronized nasal intermittent positive-pressure ventilation in a neonatal intensive care unit on bronchopulmonary dysplasia and growth in preterm infants. Am J Perinatol 2006; 23: 233240.
Bhandari V, Brodsky N, Porat R. Improved outcome of extremely low birth weight infants with Tegaderm application to skin. J Perinatol 2005; 25: 276281.
Bhandari V, Fall P, Raisz L, Rowe J. Potential biochemical growth markers in premature infants. Am J Perinatol 1999; 16: 339349.
Kamlin CO, Davis PG. Long versus short inspiratory times in neonates receiving mechanical ventilation. Cochrane Database Syst Rev 2004: CD004503.
Yost CC, Soll RF. Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database Syst Rev 2000; CD001456.
Schmidt B, Roberts RS, Davis P et al. Caffeine therapy for apnea of prematurity. N Engl J Med 2006; 354: 21122121.
Tyson JE, Wright LL, Oh W et al. Vitamin A supplementation for extremely-low-birth-weight infants. National Institute of Child Health and Human Development Neonatal Research Network. N Engl J Med 1999; 340: 19621968.
Halliday HL, Ehrenkranz RA, Doyle LW. Delayed (>3 weeks) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Database Syst Rev 2003: CD001145.
Halliday HL, Ehrenkranz RA, Doyle LW. Moderately early (714 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev 2003: CD001144.
Halliday HL, Ehrenkranz RA, Doyle LW. Early postnatal (<96 hours) corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev 2003: CD001146.
Panitch HB, Keklikian EN, Motley RA, Wolfson MR, Schidlow DV. Effect of altering smooth muscle tone on maximal expiratory flows in patients with tracheomalacia. Pediatr Pulmonol 1990; 9: 170176.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhandari, A., Bhandari, V. Bronchopulmonary dysplasia: An update. Indian J Pediatr 74, 73–77 (2007). https://doi.org/10.1007/s12098-007-0032-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-007-0032-z