Abstract
Purpose
Lung cancer (LC) has a significant impact on patients’ health-related quality of life (HRQoL). We investigate the correlations between pre-radiation therapy HRQoL and survival.
Materials and methods
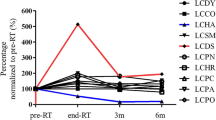
A prospective, intention-to-treat, multicentre study of 437 patients with LC recruited at the radiation oncology departments of three different institutions was conducted between 2012 and 2016. QoL was assessed using the EORTC-QLQ-C30 (v3.0) and EORTC-QLQ-LC13 questionnaires. Global health status (GHS), physical (PF), role functioning (RF), emotional (EF), cognitive (CF), and social functioning (SF) as well as symptoms scores were evaluated in univariate and multivariate analyses.
Results
The cohort consisted of 376 men (86%) and 61 women, with a median age of 66 years (range 31–88). Histology was: 72% (n = 315) non-small cell lung cancer and 28% small cell lung cancer. The most common stage was III (80%) and the median follow-up for alive patients was 30 months (range 7–76). Multivariate analysis showed that RF was associated with a lower risk of mortality (HR: 0.693; p = 0.008) and recurrence (HR: 0.737; p = 0.040). Additionally, lower scores on EF and PF were associated with higher mortality (HR: 0.696; p = 0.003 and HR: 0.765; p = 0.044, respectively). Appetite loss, constipation, and dysphagia were associated with a higher risk of mortality (HR: 1.985; p < 0.001, HR: 1.373; p = 0.036, and HR: 1.659; p = 0.002, respectively), while appetite loss was the only symptom associated with a higher risk of recurrence (HR: 1.525; p = 0.014).
Conclusions
Pre-radiation therapy scores on RF, EF, and PF and symptoms like appetite loss, dysphagia, and constipation were associated with the risk of mortality. This information could be added to other prognostic factors to guide our treatment decisions.


Similar content being viewed by others
References
Yin S, Njai R, Barker L, et al. Summarizing health-related quality of life (HRQOL): development and testing of a one-factor model. Popul Health Metr. 2016;14:22.
Yang GM, Teo I, Neo SH, et al. Pilot randomized phase II trial of the Enhancing Quality of Life in Patients (EQUIP) intervention for patients with advanced lung cancer. Am J Hosp Palliat Care. 2018. https://doi.org/10.1177/1049909118756095.
Reilly CM, Bruner DW, Mitchell SA, et al. A literature synthesis of symptom prevalence and severity in persons receiving active cancer treatment. Support Care Cancer. 2013;21:1525–50.
Chen JE, Lou VW, Jian H, et al. Objective and subjective financial burden and its associations with health-related quality of life among lung cancer patients. Support Care Cancer. 2018;26:1265–72.
Petrosyan F, Daw H, Haddad A, Spiro T. Targeted therapy for lung cancer. Anticancer Drugs. 2012;23:1016–21.
Larsson M, Ljung L, Johansson BBK. Health-related quality of life in advanced non-small cell lung cancer: correlates and comparisons to normative data. Eur J Cancer Care. 2012;21:642–9.
Lin SL, Chen YH, Yang L, Zhou JR. Pain, fatigue, disturbed sleep and distress comprised a symptom cluster that related to quality of life and functional status of lung cancer surgery patients. J Clin Nurs. 2013;22:1281–90.
Morrison EJ, Novotny PJ, Sloan JA, et al. Emotional problems, quality of life, and symptom burden in patients with lung cancer. Clin Lung Cancer. 2017;18:497–503.
Dougall AL, Swanson J, Kyutoku Y, et al. Posttraumatic symptoms, quality of life, and survival among lung cancer patients. J Appl Biobehav Res. 2017;22:e12065.
Wang B, Hao N, Zhang X. Factors influencing the psychology and quality of life in lung cancer patients. Saudi Med J. 2017;38:948–51.
van der Linden N, Bongers ML, Coupe VMH, et al. Costs of non-small cell lung cancer in the Netherlands. Lung Cancer. 2016;91:79–88.
Lefresne S, Olson R, Cashman R, et al. Prospective analysis of patient reported symptoms and quality of life in patients with incurable lung cancer treated in a rapid access clinic. Lung Cancer. 2017;112:35–40.
Ha D, Ries AL, Mazzone PJ, et al. Exercise capacity and cancer-specific quality of life following curative intent treatment of stage I-IIIA lung cancer. Support Care Cancer. 2018;26:2459–69.
Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization-for Research and Treatment of Cancer QLQ-C30: a quality of life instrument for use in international clinical-trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Ran JT, Wang JB, Bi N, et al. Health-related quality of life in long-term survivors of unresectable locally advanced non-small cell lung cancer. Radiat Oncol. 2017;12:195.
Hung HY, Wu LM, Chen KP. Determinants of quality of life in lung cancer patients. J Nurs Scholarsh. 2018;50:257–64.
Hechtner M, Krause M, Konig J, et al. Long-term quality of life in inoperable non-small cell lung cancer patients treated with conventionally fractionated compared to hyperfractionated accelerated radiotherapy—results of the randomized CHARTWEL trial. Radiother Oncol. 2018;126:283–90.
Choi S, Ryu E. Effects of symptom clusters and depression on the quality of life in patients with advanced lung cancer. Eur J Cancer Care. 2018;27:e12508.
Sarac S, Milic R, Vasiljevic M, Sarac M. Quality of life in patients with non-small cell lung cancer. Vojnosanit Pregl. 2017;74:625–32.
Turcott JG, Del Rocío Guillen Núñez M, Flores-Estrada D, Oñate-Ocaña LF, Zatarain-Barrón ZL, Barrón F, Arrieta O. The effect of nabilone on appetite, nutritional status, and quality of life in lung cancer patients: a randomized, double-blind clinical trial. Support Care Cancer. 2018;26:3029–38. https://doi.org/10.1007/s00520-018-4154-9
Xara S, Amaral TF, Parente B. Undernutrition and quality of life in non small cell lung cancer patients. Rev Port Pneumol. 2011;17:153–8.
Chasen M, Bhargava R, Hirschman S. Immunomodulatory agents for the treatment of cachexia. Curr Opin Support Palliat Care. 2014;8:328–33.
Grotmol KS, Lie HC, Hjermstad MJ, et al. W Depression-a major contributor to poor quality of life in patients with advanced cancer. J Pain Symptom Manag. 2017;54:889–97.
Anatchkova MD, Bjorner JB. Health and role functioning: the use of focus groups in the development of an item bank. Qual Life Res. 2010;19:111–23.
Li J, Bentzen SM, Li JL, et al. Relationship between neurocognitive function and quality of life after whole-brain radiotherapy in patients with brain metastasis. Int J Radiat Oncol Biol Phys. 2008;71:64–70.
Acknowledgements
This work was supported by grants from ISCIII (Fis: PI13/01155, PI16/02104) and Consejeria de Salud of the Junta de Andalucia (PI-0096–2012).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All persons listed as authors have given their approval for the submission of the paper. Authors declare that we do not have any financial support or relationships that may suppose conflict of interest.
Ethical approval
No animals were involved in this study.
Informed consent
The information collected in this research has been obtained exclusively from human participants with the previous acceptance of these through informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nieto-Guerrero Gómez, J.M., Silva Vega, G.P., Cacicedo, J. et al. Impact of pre-radiation therapy quality of life in lung cancer survival: a prospective, intention-to-treat, multicenter study. Clin Transl Oncol 22, 1635–1644 (2020). https://doi.org/10.1007/s12094-020-02310-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-020-02310-0