Abstract
Objective
Chronic hepatitis B (CHB) and metabolic dysfunction-associated fatty liver disease (MAFLD) are the leading causes of hepatocellular carcinoma (HCC). We aim to explore the impact of concurrent MAFLD on the risk of HCC in CHB.
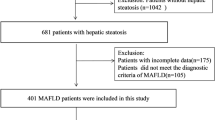
Methods
Patients with CHB were consecutively recruited from 2006 to 2021. MAFLD was defined by steatosis and either obesity, diabetes mellitus, or other metabolic abnormalities. The cumulative incidence of HCC and associated factors were compared between the MAFLD and non-MAFLD groups.
Results
10,546 treatment-naïve CHB patients were included with a median follow-up of 5.1 years. CHB patients with MAFLD (n = 2212) had fewer hepatitis B e antigen (HBeAg)-positivity, lower HBV DNA levels, and Fibrosis-4 index compared with the non-MAFLD group (n = 8334). MAFLD was independently associated with a 58% reduced risk of HCC (adjusted hazard ratio [aHR] 0.42, 95% confidence interval [CI] 0.25–0.68, p < 0.001). Furthermore, steatosis and metabolic dysfunction had distinct effects on HCC. Steatosis was protective against HCC (aHR 0.45, 95% CI 0.30–0.67, p < 0.001), while a greater burden of metabolic dysfunction increased the risk (aHR 1.40 per dysfunction increase, 95% CI 1.19–1.66, p < 0.001). The protective effect of MAFLD was further confirmed in analysis with inverse probability of treatment weighting (IPTW), patients who had undergone antiviral therapy, those with probable MAFLD, and after multiple imputation for missing data.
Conclusions
Concurrent hepatic steatosis is independently associated with a lower risk of HCC, whereas the increasing burden of metabolic dysfunction aggravates the risk of HCC in untreated CHB patients.


Similar content being viewed by others
Data availability
The data supporting this study’s findings are not publicly available due to patients’ privacy but are available from a reasonable request and approved by the Institutional Review Boards.
Abbreviations
- AASLD:
-
The American Association for the Study of Liver Diseases
- AFP:
-
Alpha-fetoprotein
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- aHR:
-
Adjusted hazard ratio
- BMI:
-
Body Mass Index
- CHB:
-
Chronic hepatitis B
- CI:
-
Confidence interval
- CAP:
-
Controlled Attenuation Parameter
- DM:
-
Diabetes mellitus
- FIB-4:
-
Fibrosis-4
- HBcAg:
-
Hepatitis B core antigen
- HBsAg:
-
Hepatitis B surface antigen
- HBeAg:
-
Hepatitis B e antigen
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- HCC:
-
Hepatocellular carcinoma
- HIV:
-
Human immunodeficiency virus
- HR:
-
Hazard ratio
- IFN:
-
Interferon
- IPTW:
-
Inverse probability of treatment weighting
- IQR:
-
Interquartile range
- MAFLD:
-
Metabolic dysfunction-associated fatty liver disease
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- NA:
-
Nucleos(t)ide analogue
References
Li J, Zou B, Yeo YH, Feng Y, Xie X, Lee DH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2019;4:389–398
Fan JG, Kim SU, Wong VW. New trends on obesity and NAFLD in Asia. J Hepatol. 2017;67:862–873
Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20
Orci LA, Sanduzzi-Zamparelli M, Caballol B, Sapena V, Colucci N, Torres F, et al. Incidence of hepatocellular carcinoma in patients with nonalcoholic fatty liver disease: a systematic review, meta-analysis, and meta-regression. Clin Gastroenterol Hepatol. 2022;20:283-292.e210
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209
Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020;40:2082–2089
Huang SC, Su HJ, Kao JH, Tseng TC, Yang HC, Su TH, et al. Clinical and histologic features of patients with biopsy-proven metabolic dysfunction-associated fatty liver disease. Gut Liver. 2021;15:451–458
Nguyen VH, Le MH, Cheung RC, Nguyen MH. Differential clinical characteristics and mortality outcomes in persons with NAFLD and/or MAFLD. Clin Gastroenterol Hepatol. 2021;19:2172-2181.e2176
Su HJ, Kao JH, Tseng TC, Yang HC, Su TH, Chen PJ, et al. Pathologic findings of patients with nonalcoholic fatty liver disease and the impact of concurrent hepatitis B virus infection in Taiwan. J Formos Med Assoc. 2020;119:1476–1482
Yang M, Wei L. Impact of NAFLD on the outcome of patients with chronic hepatitis B in Asia. Liver Int. 2022;42:1981–1990
Huang SC, Kao JH. Metabolic dysfunction-associated fatty liver disease and chronic hepatitis B. J Formos Med Assoc. 2022;121:2148–2151
Joo EJ, Chang Y, Yeom JS, Ryu S. Hepatitis B virus infection and decreased risk of nonalcoholic fatty liver disease: a cohort study. Hepatology. 2017;65:828–835
Shi JP, Fan JG, Wu R, Gao XQ, Zhang L, Wang H, et al. Prevalence and risk factors of hepatic steatosis and its impact on liver injury in Chinese patients with chronic hepatitis B infection. J Gastroenterol Hepatol. 2008;23:1419–1425
Mak LY, Hui RW, Fung J, Liu F, Wong DK, Li B, et al. Reduced hepatic steatosis is associated with higher risk of hepatocellular carcinoma in chronic hepatitis B infection. Hepatol Int. 2021;15:901–911
Oh JH, Lee HW, Sinn DH, Park JY, Kim BK, Kim SU, et al. Controlled attenuation parameter value and the risk of hepatocellular carcinoma in chronic hepatitis B patients under antiviral therapy. Hepatol Int. 2021;15:892–900
Zheng Q, Zou B, Wu Y, Yeo Y, Wu H, Stave CD, et al. Systematic review with meta-analysis: prevalence of hepatic steatosis, fibrosis and associated factors in chronic hepatitis B. Aliment Pharmacol Ther. 2021;54:1100–1109
Chan AW, Wong GL, Chan HY, Tong JH, Yu YH, Choi PC, et al. Concurrent fatty liver increases risk of hepatocellular carcinoma among patients with chronic hepatitis B. J Gastroenterol Hepatol. 2017;32:667–676
Choi HSJ, Brouwer WP, Zanjir WMR, de Man RA, Feld JJ, Hansen BE, et al. Nonalcoholic steatohepatitis is associated with liver-related outcomes and all-cause mortality in chronic hepatitis B. Hepatology. 2020;71:539–548
van Kleef LA, Choi HSJ, Brouwer WP, Hansen BE, Patel K, de Man RA, et al. Metabolic dysfunction-associated fatty liver disease increases risk of adverse outcomes in patients with chronic hepatitis B. JHEP Rep. 2021;3: 100350
Lee YC, Chao YT, Lin PJ, Yang YY, Yang YC, Chu CC, et al. Quality assurance of integrative big data for medical research within a multihospital system. J Formos Med Assoc. 2022;121:1728–1738
Tchelepi H, Ralls PW, Radin R, Grant E. Sonography of diffuse liver disease. J Ultrasound Med. 2002;21:1023–1032 (quiz 1033-1024)
Sarin SK, Kumar M, Lau GK, Abbas Z, Chan HL, Chen CJ, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10:1–98
EASL. Clinical practice guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;2017(67):370–398
Terrault NA, Lok ASF, McMahon BJ, Chang KM, Hwang JP, Jonas MM, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–1599
Su TH, Liao CH, Liu CH, Huang KW, Tseng TC, Yang HC, et al. Acoustic radiation force impulse US imaging: liver stiffness in patients with chronic hepatitis B with and without antiviral therapy. Radiology. 2018;288:293–299
Bruix J, Sherman M. American association for the study of liver D: management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022
van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67
Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014;33:1242–1258
Hui RWH, Seto WK, Cheung KS, Mak LY, Liu KSH, Fung J, et al. Inverse relationship between hepatic steatosis and hepatitis B viremia: results of a large case-control study. J Viral Hepat. 2018;25:97–104
Wang MM, Wang GS, Shen F, Chen GY, Pan Q, Fan JG. Hepatic steatosis is highly prevalent in hepatitis B patients and negatively associated with virological factors. Dig Dis Sci. 2014;59:2571–2579
Yu MW, Lin CL, Liu CJ, Huang YW, Hu JT, Wu WJ, et al. Hepatic steatosis and development of type 2 diabetes: impact of chronic hepatitis B and viral specific factors. J Formos Med Assoc. 2022;121:1478–1487
Hu D, Wang H, Wang H, Wang Y, Wan X, Yan W, et al. Non-alcoholic hepatic steatosis attenuates hepatitis B virus replication in an HBV-immunocompetent mouse model. Hepatol Int. 2018;12:438–446
Liu Q, Mu M, Chen H, Zhang G, Yang Y, Chu J, et al. Hepatocyte steatosis inhibits hepatitis B virus secretion via induction of endoplasmic reticulum stress. Mol Cell Biochem. 2022;477:2481–2491
Wong VW, Wong GL, Yu J, Choi PC, Chan AW, Chan HY, et al. Interaction of adipokines and hepatitis B virus on histological liver injury in the Chinese. Am J Gastroenterol. 2010;105:132–138
Yoon S, Jung J, Kim T, Park S, Chwae YJ, Shin HJ, et al. Adiponectin, a downstream target gene of peroxisome proliferator-activated receptor γ, controls hepatitis B virus replication. Virology. 2011;409:290–298
Seto WK, Hui RWH, Mak LY, Fung J, Cheung KS, Liu KSH, et al. Association between hepatic steatosis, measured by controlled attenuation parameter, and fibrosis burden in chronic hepatitis B. Clin Gastroenterol Hepatol. 2018;16:575-583.e572
Mak LY, Hui RW, Fung J, Liu F, Wong DK, Cheung KS, et al. Diverse effects of hepatic steatosis on fibrosis progression and functional cure in virologically quiescent chronic hepatitis B. J Hepatol. 2020;73:800–806
Huang SC, Liu CJ. Chronic hepatitis B with concurrent metabolic dysfunction-associated fatty liver disease: challenges and perspectives. Clin Mol Hepatol. 2023;29(2):320–331
van der Poorten D, Samer CF, Ramezani-Moghadam M, Coulter S, Kacevska M, Schrijnders D, et al. Hepatic fat loss in advanced nonalcoholic steatohepatitis: are alterations in serum adiponectin the cause? Hepatology. 2013;57:2180–2188
Kanwal F, Kramer JR, Mapakshi S, Natarajan Y, Chayanupatkul M, Richardson PA, et al. Risk of hepatocellular cancer in patients with non-alcoholic fatty liver disease. Gastroenterology. 2018;155:1828-1837.e1822
Yu MW, Shih WL, Lin CL, Liu CJ, Jian JW, Tsai KS, et al. Body-mass index and progression of hepatitis B: a population-based cohort study in men. J Clin Oncol. 2008;26:5576–5582
Davila JA, Morgan RO, Shaib Y, McGlynn KA, El-Serag HB. Diabetes increases the risk of hepatocellular carcinoma in the United States: a population based case control study. Gut. 2005;54:533–539
Chen CL, Yang HI, Yang WS, Liu CJ, Chen PJ, You SL, et al. Metabolic factors and risk of hepatocellular carcinoma by chronic hepatitis B/C infection: a follow-up study in Taiwan. Gastroenterology. 2008;135:111–121
Hsueh RC, Wu WJ, Lin CL, Liu CJ, Huang YW, Hu JT, et al. Impact of PNPLA3 p.I148M and hepatic steatosis on long-term outcomes for hepatocellular carcinoma and HBsAg seroclearance in chronic hepatitis B. J Hepatocell Carcinoma. 2022;9:301–313
Li J, Yang HI, Yeh ML, Le MH, Le AK, Yeo YH, et al. Association between fatty liver and cirrhosis, hepatocellular carcinoma, and hepatitis B surface antigen seroclearance in chronic hepatitis B. J Infect Dis. 2021;224:294–302
Minuk GY, Iliant V, Zhou N, Kaita KD, Wong SG, Peretz D, et al. Concomitant nonalcoholic fatty liver disease does not alter the activity, severity or course of primary biliary cholangitis. Liver Int. 2018;38:1110–1116
De Luca-Johnson J, Wangensteen KJ, Hanson J, Krawitt E, Wilcox R. Natural history of patients presenting with autoimmune hepatitis and coincident nonalcoholic fatty liver disease. Dig Dis Sci. 2016;61:2710–2720
Acknowledgements
We thank Miss Shih-Wan Chou for her administrative assistance and the Department of Medical Research, National Taiwan University Hospital staff for the Integrated Medical Database. In addition, we thank the 7th Core Laboratory of the Department of Medical Research, National Taiwan University Hospital, for technical assistance.
Funding
This work was supported by grants from the Ministry of Science and Technology, Taiwan (grant numbers MOST 109-2326-B-002-012-MY3, MOST 110-2326-B-400-004, MOST 110-2628-B-002-041), National Taiwan University Hospital (Grant numbers VN-110-02, 110-S4952, 110-N01, NTUH110-T20).
Author information
Authors and Affiliations
Contributions
SCH: study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; statistical analysis. THS: study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; obtained funding; study supervision. TCT: analysis and interpretation of data; critical revision of the manuscript for important intellectual content. CLC: analysis and interpretation of data; critical revision of the manuscript for important intellectual content. SJH: analysis and interpretation of data; critical revision of the manuscript for important intellectual content. SHL: analysis and interpretation of data; critical revision of the manuscript for important intellectual content. CMH: analysis and interpretation of data; critical revision of the manuscript for important intellectual content. CHL: analysis and interpretation of data; critical revision of the manuscript for important intellectual content. TYL: critical revision of the manuscript for important intellectual content; technical support. HCY: analysis and interpretation of data; critical revision of the manuscript for important intellectual content; study supervision. CJL: analysis and interpretation of data; critical revision of the manuscript for important intellectual content; study supervision. PJC: analysis and interpretation of data; critical revision of the manuscript for important intellectual content; study supervision. JHK: study concept and design; analysis and interpretation of data; drafting of the manuscript; obtained funding; study supervision. All authors: final approval of the version to be published.
Corresponding authors
Ethics declarations
Conflict of interest
T-HS received a research Grant from Gilead Sciences, and was on speaker’s bureaus for Abbvie, Bayer, Bristol-Myers Squibb, Gilead Sciences, Merck Sharp and Dohme, and Takeda. J-HK has served as a consultant for Abbvie, Abbott, Gilead Sciences, Roche, and Sysmex and on speaker’s bureaus for Abbvie, Bristol-Myers Squibb, Gilead Sciences, Merck Sharp, and Dohme, and Sysmex. S-CH, T-CT, C-LC, S-JH, S-HL, C-MH, C-HL, T-YL, H-CY, C-JL, P-JC declare no conflict of interest.
Ethical approval
This study was approved by the Institutional Review Board of National Taiwan University Hospital (202104086RIND) and conformed to the ethical principles for medical research involving human subjects of the Declaration of Helsinki updated in 2013. The informed consent was waived because this is a retrospective study conducted by a review of medical records only.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, SC., Su, TH., Tseng, TC. et al. Distinct effects of hepatic steatosis and metabolic dysfunction on the risk of hepatocellular carcinoma in chronic hepatitis B. Hepatol Int 17, 1139–1149 (2023). https://doi.org/10.1007/s12072-023-10545-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-023-10545-6