Abstract
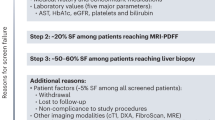
Non-alcoholic steatohepatitis (NASH) is an increasingly common cause of cirrhosis, hepatocellular carcinoma, and liver-related death (LRD). Consequently, there is a critical need for effective drug therapy that improves clinically relevant end-points. Hepatic steatosis assessed by magnetic resonance imaging-proton density fat fraction is increasingly used in the early phase trials examining drugs with anti-steatotic effects. However, the prognostic significance of a reduction in steatosis is unknown, and thus, phase 3 trials require a histological end-point of NASH resolution without fibrosis progression. Nonetheless, it is not clear whether this end-point which requires a liver biopsy reflects a better prognosis. Thus, conditional drug approval currently requires long-term follow-up to demonstrate reduction in ‘harder’ end-points of cirrhosis, liver transplantation, and LRD. Currently, there is an essential need to develop accurate non-invasive markers that are dynamic to drug-induced changes in underlying disease severity and prognosis to utilize as surrogate end-points for clinical trials in NASH.
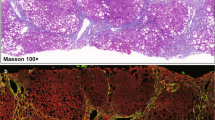
Graphical abstract


Similar content being viewed by others
Change history
09 May 2019
In the original article the title was incorrectly published. This has been corrected and the original article has been updated.
References
Kim D, Kim WR, Kim HJ, Therneau TM. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology (Baltimore, MD) 2013;57:1357–1365
Kabbany MN, Conjeevaram Selvakumar PK, Watt K, Lopez R, Akras Z, Zein N, et al. Prevalence of nonalcoholic steatohepatitis-associated cirrhosis in the United States: an analysis of National Health and Nutrition Examination Survey Data. Am J Gastroenterol 2017;112:581–587
Teli MR, James OF, Burt AD, Bennett MK, Day CP. The natural history of nonalcoholic fatty liver: a follow-up study. Hepatology (Baltimore, MD) 1995;22:1714–1719
Dam-Larsen S, Becker U, Franzmann MB, Larsen K, Christoffersen P, Bendtsen F. Final results of a long-term, clinical follow-up in fatty liver patients. Scand J Gastroenterol 2009;44:1236–1243
Ekstedt M, Franzen LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology (Baltimore, MD) 2006;44:865–873
Angulo P, Kleiner DE, Dam-Larsen S, Adams LA, Bjornsson ES, Charatcharoenwitthaya P, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2015;149(389–97):e10
Vilar-Gomez E, Bertot LC, Wong VW, Castellanos Fernandez MI, Aller R, Eslam M, et al. The long-term clinical course of histologically advanced nonalcoholic fatty liver disease. Impact of fibrosis severity on major clinical outcomes. Hepatology (Baltimore, Md) 2017;66:33A-34A
Adams LA, Lymp JF, Sauver JS, Sanderson SO, Lindor KD, Feldstein A, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 2005;129:113–121
Sanyal AJ, Banas C, Sargeant C, Luketic VA, Sterling RK, Stravitz RT, et al. Similarities and differences in outcomes of cirrhosis due to nonalcoholic steatohepatitis and hepatitis C. Hepatology (Baltimore, MD) 2006;43:682–689
Sanyal AJ, Friedman SL, McCullough AJ, Dimick-Santos L, American Association for the Study of Liver D, United States F et al. Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: findings and recommendations from an American Association for the Study of Liver Diseases—US Food and Drug Administration Joint Workshop. Hepatology (Baltimore, Md) 2015;61:1392–1405
Calzadilla Bertot L, Adams LA. The natural course of non-alcoholic fatty liver disease. Int J Mol Sci 2016;17(5):pii: E774. https://doi.org/10.3390/ijms17050774
Ratziu V. A critical review of endpoints for non-cirrhotic NASH therapeutic trials. J Hepatol 2017;68:353–361
Filozolf C, Chow S-C, Dimick-Santos L, Chen Y-F, Williams RN, Goldstein BJ, et al. Clinical endpoints and adaptive clinical trials in precirrhotic nonalcoholic steatohepatitis: facilitating development approaches for an emerging epidemic. Hepatol Commun 2017;1:577–585
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology (Baltimore, MD) 2005;41:1313–1321
Loomba R, Kayali Z, Noureddin M, Ruane P, Lawitz EJ, Bennett M, et al. GS-0976 reduces hepatic steatosis and fibrosis markers in patients with nonalcoholic fatty liver disease. Gastroenterology. 2018. https://doi.org/10.1053/j.gastro.2018.07.027
Loomba R, Lawitz E, Mantry PS, Jayakumar S, Caldwell SH, Arnold H, Diehl AM, et al; GS-US-384-1497 Investigators. The ASK1 inhibitor selonsertib in patients with nonalcoholic steatohepatitis: A randomized, phase 2 trial. Hepatology. 2017. https://doi.org/10.1002/hep.29514. [Epub ahead of print]
Caussy C, Reeder SB, Sirlin CB, Loomba R. Noninvasive, quantitative assessment of liver fat by MRI-PDFF as an endpoint in NASH trials. Hepatology (Baltimore, MD) 2018;68:763–772
Ajmera V, Park CC, Caussy C, Singh S, Hernandez C, Bettencourt R, et al. Magnetic resonance imaging proton density fat fraction associates with progression of fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology 2018;155(307–10):e2
Patel J, Bettencourt R, Cui J, Salotti J, Hooker J, Bhatt A, et al. Association of noninvasive quantitative decline in liver fat content on MRI with histologic response in nonalcoholic steatohepatitis. Ther Adv Gastroenterol 2016;9:692–701
Chow JC, Wong GL, Chan AW, Shu SS, Chan CK, Leung JK, et al. Repeating measurements by transient elastography in non-alcoholic fatty liver disease patients with high liver stiffness. J Gastroenterol Hepatol. 2018. https://doi.org/10.1111/jgh.14311
Hsu C, Caussy C, Imajo K, Chen J, Singh S, Kaulback K, et al. Magnetic resonance vs transient elastography analysis of patients with nonalcoholic fatty liver disease: a systematic review and pooled analysis of individual participants. Clin Gastroenterol Hepatol. 2018. https://doi.org/10.1016/j.cgh.2018.05.059
Jayakumar S, Middleton MS, Lawitz EJ, Mantry PS, Caldwell SH, Arnold H, et al. Longitudinal correlations between MRE, MRI-PDFF, and liver histology in patients with non-alcoholic steatohepatitis: analysis of data from a phase II trial of selonsertib. J Hepatol. 2018. https://doi.org/10.1016/j.jhep.2018.09.024
Boursier J, Vergniol J, Guillet A, Hiriart JB, Lannes A, Le Bail B, et al. Diagnostic accuracy and prognostic significance of blood fibrosis tests and liver stiffness measurement by FibroScan in non-alcoholic fatty liver disease. J Hepatol 2016;65:570–578
Vilar-Gomez E, Calzadilla-Bertot L, Friedman SL, Gra-Oramas B, Gonzalez-Fabian L, Lazo-Del Vallin S, et al. Serum biomarkers can predict a change in liver fibrosis 1 year after lifestyle intervention for biopsy-proven NASH. Liver Int 2017;37:1887–1966
Chalasani N, Abdelmalek MF, Loomba R, Kowdley KV, McCullough AJ, Dasarathy S, et al. Relationship between three commonly used non-invasive fibrosis biomarkers and improvement in fibrosis stage in patients with NASH. Liver Int. 2018. https://doi.org/10.1111/liv.13974
Kamada Y, Ono M, Hyogo H, Fujii H, Sumida Y, Yamada M, et al. Use of Mac-2 binding protein as a biomarker for nonalcoholic fatty liver disease diagnosis. Hepatol Commun 2017;1:780–791
Alkhouri N, Johnson C, Adams L, Kitajima S, Tsuruno C, Colpitts TL, et al. Serum Wisteria floribunda agglutinin-positive Mac-2-binding protein levels predict the presence of fibrotic nonalcoholic steatohepatitis (NASH) and NASH cirrhosis. PLoS One 2018;13:e0202226
Lai LL, Chan WK, Sthaneshwar P, Nik Mustapha NR, Goh KL, Mahadeva S. Serum Wisteria floribunda agglutinin-positive Mac-2 binding protein in non-alcoholic fatty liver disease. PLoS One 2017;12:e0174982
European Association for the Study of the Liver, Electronic address eee, European Association for the Study of D, European Association for the Study of O. EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64:1388–1402
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I declare that I have no conflict of interest.
Ethical approval
This article is a review of the literature and does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adams, L.A. End-points for drug treatment in NASH. Hepatol Int 13, 253–258 (2019). https://doi.org/10.1007/s12072-019-09935-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-019-09935-6