Abstract
The study aims to assess the prevalence of food insecurity and malnutrition and to investigate the association between food insecurity, sociodemographic characteristics, and malnutrition among Indian older adults. Data for 28,004 older adults (60 + years) was extracted from Wave-1 of the Longitudinal Aging Study in India, 2017-18. Bivariate analysis was used for prevalence estimates. Multinomial logistic regression provided relative risk ratios (RRR) to determine the association. About 45% of older adults were food insecure and nearly half were malnourished (underweight − 26.7%, overweight − 22.2%). Overweight was widespread in southern, western, and northern India, while underweight and food insecurity were widespread in central, eastern, and north-eastern India. Food insecure older adults were significantly more likely to be underweight (mild: RRR = 1.105, 95% CI = 1.038–1.176; severe: RRR = 1.327, 95% CI = 1.186–1.485). Rather than severe food insecurity, those with moderate food insecurity have the least likelihood of being overweight. Being the oldest, male, widowed, divorced/separated/deserted, having fewer years of schooling, living in a ST or SC household, and in rural areawere associated with higher risk of being underweight; while their other counterparts were of being overweight. No association was found between working status and underweight, meanwhile the non-working older adults were less likely to be overweight (RRR = 0.804, 95% CI = 0.744–0.868). Underweight is strongly linked to food insecurity. In terms of food insecurity and malnutrition, the most vulnerable categories identified include oldest old, widowed, divorced/separated/deserted, SC, ST, economically weaker, and persons without or with only a few years of formal education.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aging is a process that begins right at birth, and it is an unavoidable process, but it can be regulated and monitored for better health and well-being outcomes in later life. The term ‘older adults’ refers to people in their late life. The United Nations defines older adults as people aged 60 and above (Bukunmi & Jeremiah, 2018). Worldwide, older adults are estimated to be 1.049 billion in 2020, and it is projected to reach 1.859 billion in 2050 (UN DESA/PD, 2019). This indicates that people are living longer than earlier. Longevity is an outstanding achievement, but it does not ensure that people live a healthy life over those extended years. Because, with ageing, people become more vulnerable to health-related predicaments such as malnutrition, chronic illness, and diseases (Bukunmi & Jeremiah, 2018). Malabsorption of macronutrients and micronutrients is also common in older adults with morbidities (Russell, 2001), which affects their overall health and nutritional outcomes. Malnutrition is a term used to describe undesirable nutritional outcomes that are frequently associated with longer hospital stays, increased readmissions (Lim et al., 2012), premature mortalities, low quality of life, and increased functional limitations (WHO, 2017). Moreover, loneliness, financial worries, and food insecurity are more likely to be a problem at older age than at younger age; these problems can lead to depression, lack of appetite, and physical and functional limitations (Miller et al., 2020).
Unlike in developed nations, underweight is more prevalent than overweight and obesity in developing nations, but they are estimated to surpass the prevalence of overweight in developed countries in the near future (Bhurosy & Jeewon, 2014; Abdullah, 2015). Because the developing nations are observing rapid changes in diets and activity patterns, i.e., a shift from physical to more sedentary activities (Caballero, 2007; Abdullah, 2015), which are the prime reasons for the increasing prevalence of overweight and obesity across the globe. And this has led developing nations to face a ‘double burden of malnutrition’, i.e., underweight and overweight (Letamo, 2020). In older adults, while being underweight leads to fatigue and constant tiredness, higher infection rates and death, being overweight contrarily leads to more chronic non-transmissible diseases such as diabetes, hypertension, coronary artery disease, reduced functionality, disability and mortality (Gupta et al., 2018). In both cases, it becomes difficult for older adults to achieve a good quality of life. In advancing countries like India, national health policy and legislation are primarily concerned with maternal and child well-being and infectious diseases. On the other hand, the health status of older adults is not adequately addressed (Kapoor & Anand, 2002). Malnutrition among older adults is a serious health issue that must be addressed to ensure a healthy ageing experience for older adults (Khole & Soletti, 2018). As per the UN DESA/PD (2019) estimates, in 2020, with 139.6 million 60 + population (10.1% of the total population), India has the second-largest older adult population in the world and is projected to surpass double its current size to reach 289.5 million (17.3% of the total population) in the next three decades. Besides this, it is witnessing a steady increase in overweight and obesity prevalence among its adults (Vennu et al., 2019). Furthermore, it is contributing the highest proportion to underweight adults globally (NCD Risk Factor Collaboration, 2016). As a result, the ‘double burden of malnutrition’, which is widespread in developing countries, is a major public health concern in India (Arnold et al., 2009).
Both the forms of malnutrition, i.e., underweight and overweight are the most serious consequences of food insecurity (Chinnakali et al., 2014). “Food insecurity is a situation of inadequate access to enough, safe and nutritious food that meets one’s dietary needs and preferences for an active and healthy life” (FAO et al., 2021). Globally, in 2020, the COVID-19 pandemic ravaged the world, resulting in moderate or severe food insecurity prevalence rising to 30.4% from 26.6% to 2019, nearly as much as over the past five years (from 22.6% to 2014) (FAO et al., 2021). Among the world regions, Asia has the second-highest prevalence of moderate and severe food insecurity with 25.8%; and among its sub-regions, South Asia has the highest prevalence with 43.8% (FAO et al., 2021). Given that, India has a significantly larger population size than other South Asian nations, it is reasonable to assume that it shares a majority proportion of the food insecure population in South Asia. Among all the age groups, older adults may have been the most severely affected because they are more susceptible to food insecurity. This can be attributed to fewer economic opportunities, low-paying jobs, social isolation, living alone, minority status and functional impairments in old age (Lee & Frongillo Jr, 2001; Simsek et al., 2013); and their reliance on other family members to meet their daily and healthcare needs (Keshari & Shankar, 2021).
Food insecurity is a risk factor for poor health, quality of life, and nutritional status (Simsek et al., 2013). It could be linked to overweight owing to unhealthy dietary patterns, such as the intake of inexpensive diets rich in energy or simple carbohydrates and fats (Nord et al., 2009); it could also lead to weight loss, especially in its most extreme form, i.e., hunger (Morales & Berkowitz, 2016). Older adults are more prone to food insecurity lead malnutrition and other health-related issues than younger adults (Lee & Frongillo Jr,, 2001). Because attaining nutritional balance in old age is difficult due to the higher prevalence of physical or physiological problems, malabsorption of nutrients, eating dependencies, sarcopenia, appetite decline, poor psychological status, and social isolation (Russell, 2001; Grammatikopoulou et al., 2019).
Determinants of Malnutrition in Aged Persons (DoMap) model demonstrates the direct and indirect malnutrition risk factors associated with the three principal conditions involved in the development of malnutrition: low intake, high requirements, and impaired nutrient bioavailability (Volkert et al., 2019). Indirect factors, such as low educational level and poverty, may lead to malnutrition by activating one of these three principal conditions. Sociodemographic characteristics are well-known predictors of such indirect factors, thus, some sociodemographic characteristics can predict malnutrition in older adults (Krzyminska-Siemaszko et al., 2021). A recent systematic review and meta analysis of 40 studies from various countries (Besora-Moreno et al., 2020) and 45 studies on Indian population (Kushwaha et al., 2020) assessing the risk of malnutrition in various older adult populations confirmed a strong relation between several socioeconomic factors (such as age, sex, educational level, marital status, income level, occupational level, place of residence, and region) and malnutrition or risk of malnutrition in older adults aged above 60. The studies found a mixed association between socioeconomic variables and malnutrition or risk of malnutrition. For example, of the 31 studies that evaluated educational level, 15 established significant relationships with regard to malnutrition or malnutrition risk, of which 11 studies showed a negative association, and the other four had a contrary result (Besora-Moreno et al., 2020). In the Indian context, age, sex, educational level, working status, marital status, place of residence, economic status, and caste significantly impacts indirect factors that can be associated with malnutrition (Arlappa et al., 2006; Sengupta et al., 2015; Konda et al., 2018; Kushwaha et al., 2020).
The issue of malnutrition and food insecurity has attracted the attention of policymakers worldwide. That is reflected in the two indicators for monitoring the Sustainable Development Goal (SDG) Target 2.1: “By 2030, end hunger and ensure access by all people, in particular the poor and people in vulnerable situations, including infants, to safe, nutritious, and sufficient food all year round.” The two SDG Indicators are “2.1.1- the prevalence of undernourishment” and “2.1.2- the prevalence of moderate or severe food insecurity in the population based on the Food Insecurity Experience Scale (FIES)” (FAO et al.,2021). Having said that, while there exist a number of studies on nutritional and food insecurity status among Indian children and women, there is a scarcity of studies that have addressed the issue of malnutrition among Indian older adults. Since malnutrition is a reversible condition and food security is necessary to prevent and overcome various malnutrition associated limitations in later life (Amarya et al., 2015), a nationwide estimate is required to assess the prevalence of food insecurity and malnutrition among older adults in India.
Previous studies in Bangladesh (Alam et al., 2011), Greece (Grammatikopoulou et al., 2019; Gkiouras et al., 2020), Turkey (Simsek et al., 2013), and the United States (Jung et al., 2019) have associated malnutrition and food insecurity, and pointed out that food insecurity is a significant predictor of poor nutritional status among older adults. According to our knowledge, the association between food insecurity and malnutrition has not been investigated in the Indian context. Existing studies in India have examined the risk factors of malnutrition (Arlappa et al., 2006; Rajkamal et al., 2015; Konda et al., 2018; Khole & Soletti 2018) and food insecurity (Chinnakali et al., 2014; Saxena et al., 2020; Keshari & Shankar, 2021) among older adults but have not investigated their association. Moreover, there is significantly higher heterogeneity among these studies in terms of both prevalence and risk of malnutrition and food insecurity. Due to data constraints, the existing studies are limited to state, district, regional, and community levels. Thus, the present study attempts to assess the prevalence of malnutrition and the severity level of food insecurity among people aged above 60 years in India using the Longitudinal Aging Survey of India (LASI), 2017-18, a population-based survey, that covers all Indian states and union territories. Also, it tries to find out if there is a link between malnutrition in older adults and food insecurity and certain sociodemographic factors.
Data and methods
Data
The first and most recent wave of the Longitudinal Aging Survey of India (LASI) conducted in 2017-18 has been used in the present study. LASI, 2017-18, includes detailed information on health care practices, health behaviour and risk factors, health care utilisation, and various demographic and socioeconomic characteristics. Moreover, LASI, 2017-18 is the only dataset available for India that covers older adults from all of its states and union territories and is published in 2020 (IIPS et al., 2020). From a 31,464 nationally representative older adult population aged above 60 years in India, questions on food insecurity were answered by 28,521 older adults (male-13,714; female-14,807), and anthropometric measurements (height and weight) were collected for only 28,050 older adults (male-13,509; female-14,541). Only 28,004 (male-13,480; female-14,524) of the older adults have both anthropometric measurements and responses to the food security questions; hence, only they have been considered as a sample of the present study. A detail procedure of sample selection is depicted in Fig. 1.
Dependent variables
Nutritional Status.
Body mass index (BMI) is an important indicator used to assess an individual’s nutritional status (IIPS et al., 2020). In LASI, 2017-18, the height and weight of adults were measured using standard procedures. The BMI of an individual is the ratio of its weight (in kilograms) to the square of its height (in metres), which was calculated by using the formula: BMI (kg/m2) = [weight (kg)]/ [height (m)] 2. For this study, the WHO classification was adopted to classify the BMI in terms of underweight, normal weight and overweight: underweight if BMI < 18.5 kg/m2; normal weight if BMI in the range of 18.5–24.9 kg/m2; overweight/obese if BMI ≥ 25 kg/m2.
Explanatory variables
Food Insecurity Level.
Charlton & Rose (2001) reported that inadequate household food security and poor socioeconomic conditions are among the various causes of the poor nutritional status of older adults. In this study, the primary explanatory variable is the severity level of food insecurity as measured using the Food Insecurity Experience scale (FIES) that was developed by the Food and Agriculture Organization (FAO) Voices of the Hungry (VOH) project. FIES is capable of producing a reliable food insecurity prevalence even in countries where food insecurity is either very low or very high, because of its strength and accuracy, in addition to the long-tested robustness of its 8 questions (FAO, 2017). The severity level of food insecurity was classified as mild, moderate, and severe based on eight FIES items associated with the experience captured by the eight different questions with dichotomous answers (Yes/No) asked of the individual (Ballard et al., 2013). However, in LASI, individuals were asked only four of those eight questions, which were assumed to indicate the severity level of food insecurity that the individual experienced in 12 months preceding the survey. Citing this limitation, we followed Ballard et al., (2013)’s classification of the eight FIES items for the four items in LASI: one question each indicating mild and moderate, and the other two indicating severe:
-
Mild: “if the respondent did not eat enough food of his/her choice (excluding fasting/food-related restrictions due to religious or health-related reason)”.
-
Moderate: “if the respondent reduced the size of your meals or skipped meals because there was not enough food at its household”.
-
Severe: “if the respondent ‘was hungry but did not eat’ or ‘did not eat for a whole day’ because there was not enough food at its household (excluding fasting/food-related restrictions due to religious or health-related reason)”.
Sociodemographic Characteristics.
Health and nutrition outcomes can also be observed through any individual’s socioeconomic status (SES) (Khole & Soletti, 2018). In this study, sociodemographic characteristics of older adults (60 + years) were classified into individual and household characteristics. The individual characteristics include age groups (60–74 years, 75 + years), sex (male, female), years of schooling (no education, 1–4 years, 5–9 years, 10 + years), working status (working, not working), and marital status (married/in a live-in relationship, never married, widowed, and divorced/separated/deserted). Household characteristics include place of residence (rural, urban), social group (scheduled caste [SC], scheduled tribe [ST], other backward castes [OBC], and Non-SC/ST/OBC), monthly per capita expenditure (MPCE) quintile (poorest, poorer, middle, richer, and richest) and the six geographical regions of India: Northern, Western, Central, Eastern, North-eastern and Southern.
Statistical methods
Bivariate analysis was carried out to assess the prevalence of food insecurity and malnutrition (underweight and overweight) among Indian older adults by their sociodemographic characteristics. Pearson’s chi-square test for independence was used to test whether or not there is a significant association between the independent and dependent variables. Since the dependent variable, i.e., nutritional status, has more than two unordered categories, the multinomial logistic regression model was employed to see the association between malnutrition and food insecurity by adjusting for individual and household factors. Model-I was fitted to see the association between the severity level of food insecurity and malnutrition. Further, additional adjustments were made, in which model II adjusted for individual characteristics viz., age, sex, years of schooling, working status, and marital status; and model III adjusted for household characteristics viz., place of residence, social group, MPCE quintile, and region. A P-value of less than 0.05 was considered statistical significance by a two-tailed test. The result of the multinomial logistic regression model was presented in terms of the Relative Risk Ratio (RRR) and the 95% confidence interval (CI). All the statistical analyses were carried out using the statistical software package Stata/SE, version 14.
The general multinomial logistic regression model for this study is specified according to Schmidt & Strauss (1975):
\(Pr\left({Y}_{i}=j\right)=\frac{{e}^{{\beta }_{j}{X}_{i}}}{1+\sum _{k=1}^{J}{e}^{{\beta }_{j}{X}_{i}}}\), j=1, 2, 3 (1).
Where \(Pr\left({Y}_{i}=j\right)\) denotes the probability of an individual ‘i’ being in the outcome category ‘j’. ‘J’ is the number of categories in the outcome variables; in this case it is 3, hence ‘j’ takes a value of 1, 2, or 3. \({\beta }_{j}\) is the regression coefficient.
Owing to the three categories of the outcome variable in the study, the model has two equations. The simplified equations are as follows:
The Eq. 2 represents the log odds (logit) of being underweight relative to normal weight. Similarly, Eq. 3 is for the log odds of being overweight relative to normal weight. In both the equations, \(x\)is the self-reported severity level of food insecurity, and \(Y, \text{a}\text{n}\text{d} Z\) are the sets of individual and household characteristics, respectively; and \({\alpha }_{k},{\beta }_{k}, and {\gamma }_{k}\) are the slope coefficients, and \({\epsilon }_{k}\) is the error term for the respective equations. In this study, the estimated parameters represent the RRR.
An RRR > 1 indicates the risk of being in the comparison group (underweight or overweight) relative to the risk of being in the referent group (normal weight) for the comparison group (mildly/moderately/severely food insecure) of the independent variable is higher than that of the referent group (food secure) of the independent variable. In other words, the comparison group (mildly/moderately/severely food insecure) of the independent variable is more likely to be in the comparison outcome (underweight/overweight). Explained in another way, an RRR < 1 indicates that the risk of the older adults being underweight/overweight relative to the older adults being normal is lower for the mildly/moderately/severely food insecure older adults as compared to the food secure older adults.
Results
Sample characteristics
Table 1 displays the sample characteristics, the prevalence of malnutrition and the severity level of food insecurity among older adults (60 + years) by sociodemographic characteristics. Of the 28,004 older adults selected for the study, 79.7% were aged 60–74 years, and 20.3% were aged 75 + years; about 52% were female; more than half (53.4%) had no education; about two-thirds (66.6%) were from rural areas; and 64.5% were married. Further details are depicted in Table 1.
Prevalence of Malnutrition by Severity Level of Food Insecurity and Sociodemographic characteristics
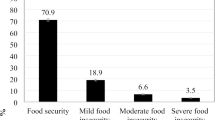
As shown in Fig. 2, two in every five (44.6%) Indian older adults (60 + years) have experienced food insecurity at different levels: mild-37.5%, moderate-2.1%, and severe-5%. Meanwhile, one in every two (48.8%) older adults was malnourished, with 26.7% underweight and 22.1% overweight (including 5.5% obese).
It can also be seen from Table 1 that the prevalence of underweight was higher among the severe food insecure older adults (38.1%), and overweight is more prevalent among the food secure (23.6%) and mildly food insecure (21.7%) older adults. In individual characteristics, the prevalence estimates differed between men and women (p < 0.001), with women being overweight. It is also worth noting that underweight and overweight prevalence is relatively identical among women and young olds (60–74 years). Meanwhile, men and the oldest olds (75+) have recorded a higher prevalence of underweight than overweight. With increasing years of schooling, a sharp decline in severe food insecurity and underweight prevalence was noticed. On the other hand, 41.2% of older adults with 10 or more years of schooling were overweight. This was a much higher rate than among younger adults.
It is also apparent from Table 1 that the prevalence of underweight and overweight differed significantly between older adults living in rural and urban areas; while underweight was more common in rural areas, overweight is more common in urban areas. While there was no significant difference in the prevalence of malnutrition across the social groups, underweight was found to be more prevalent among in SC and ST communities, and overweight in the Non-SC/ST/OBC community; whereas among the OBCs, the prevalence of malnutrition is roughly distributed equally between underweight and overweight. Although the prevalence of malnutrition was roughly comparable across the MPCE quintiles, it is worth mentioning that as the MPCE quintile rises, the prevalence of underweight declines and overweight rises. However, the proportion of older adults who were food insecure was remarkably higher among the poorest MPCE quintile compared to the older adults from the other four MPCE quintiles. Though the prevalence of malnutrition did not differ much among India’s regions, the prevalence of being underweight or overweight did. While underweight is more prevalent in central (36.3%), eastern (33.6%), and north-eastern regions (30.6%), overweight is more prevalent in north (26.9%), west (28%) and south (32.5%).
Association between Food Insecurity level, Sociodemographic characteristics and Malnutrition:
Table 2 provides the results obtained from multinomial logistic regression in terms of the RRR, and 95% CI, which indicate the estimated relationships between food insecurity level and nutritional status, following adjustment for individual and household characteristics. Where normal weight is the baseline or the reference category, and underweight and overweight are the comparison categories. The RRR is estimated in terms of underweight relative to normal and overweight relative to normal. The unadjusted model (Model 1) shows that as the severity level of food insecurity grows, so does the risk of being underweight, with a higher risk among the severely food insecure older adults, i.e., 1.71 times more likely (RRR = 1.707, 95% CI = 1.705–1.709) than the food secure older adults. However, an increase in the severity level of food insecurity was associated with a lower risk of being overweight (mild: RRR = 0.948, 95% CI = 0.948–0.949; moderate: RRR = 0.622, 95% CI = 0.623–0.624; severe: RRR = 0.669, 95% CI = 0.668–0.67).
Adjusting for household and individual characteristics in Model 3 attenuated the relationships between food insecurity level and malnutrition, whilst most of the results remained statistically significant. However, no statistically significant result was obtained for overweight relative to normal weight. The estimates from model 3 indicate that the oldest-old were significantly more likely to be underweight and less likely to be overweight compared to the young old. The most striking results have come out for female relative to male and for older adults with 10 + years of schooling relative to older adults with no education. In that instance, compared to males, females were at a 26% lower risk (RRR = 0.741, 95% CI = 0.71–0.772) of being underweight, whereas they were at a 95% higher risk (RRR = 1.954, 95% CI = 1.856–2.052) of being overweight. Similarly, compared to older adults with no education, those with 10 + years of schooling had a 57% lower risk (RRR = 0.43, 95% CI = 0.399–0.461) of being underweight, but a 128% higher risk (RRR = 2.279, 95% CI = 2.137–2.421) of being overweight. In other words, the higher the educational level of older adults, the more likely they are to be overweight. Unmarried, widowed, and divorced/separated/deserted older adults were more likely to be underweight and less likely to be overweight compared to older adults in a marital union or a live-in relationship. The older adults from urban areas, belonging to ST and SC communities had a significantly higher risk of being underweight compared to their urban and non-SC/ST counterparts. Older adults living in lower MPCE (poorer and poorest) households were significantly more likely to be underweight, and older adults living in the higher (richer and richest) MPCE households were more likely to be overweight.
Discussion
The present study was set out to determine the prevalence of food insecurity and malnutrition among Indian older adults and investigate the association of malnutrition with food insecurity and sociodemographic characteristics. The study found that about one in every two older adults (49%) in India are malnourished, with underweight and overweight accounting for approximately 55% and 45%, respectively. In terms of overall malnutrition, this finding is slightly similar to that of Khole & Soletti (2018). However, it differs in terms of its distribution across underweight (25%) and overweight (75%). The prevalence of malnutrition differed by the level of food insecurity. Overweight was found to be greater among food secure and mildly food insecure older adults, and underweight among the moderately and severely food insecure older adults. This finding shows a similar pattern to that observed by Souza & Marin-Leon (2013) and Hosseinpour et al., (2019). It is also interesting to note that the proportion of underweight and overweight among food-secured older adults is fairly similar. The result also indicates a remarkable proportion of food insecure older adults are not only underweight but also overweight, and this finding is consistent with Dinour et al., (2007)’s argument. This may be due to monotonous diets and low cost or inexpensive diets high in energy or simple carbohydrates and fats (Nord et al., 2009), which is a strategy used to combat food insecurity, leading to overconsumption of energy and fat-rich foods, which often results in weight gain (Pan et al., 2012). Multinomial logistic regression results revealed that, as the severity of food insecurity increases, so does the risk of being underweight. However, on the other hand, there is no significant association between being overweight and food insecurity.
No association was established between food insecurity and the age group of older adults. It is difficult to explain this result, but one possible reason is that most older adults rely on their supporters to get the food they need or the food they want. Hence, the traits of the supporter are far more essential than the older adults’ age in determining their food security. Working older adults were shown to have a greater prevalence of moderate and severe food insecurity, which could be because working in later life is more common among economically destitute older adults who usually work to meet their daily requirements or to support their families. Older adults who were never married and divorced/separated/deserted have recorded a dramatically higher prevalence of food insecurity than married and widowed older adults. This finding is supported by a recent study in urban Varanasi, India (Keshari & Shankar, 2021). In household characteristics, older adults living in rural, SC/ST, and lower MPCE households have a higher prevalence of moderate and severe food insecurity. This could be because rural and SC/ST households are mostly clustered in isolated areas with no market access, which has a negative impact on their economic access as well as their health and food consumption (Bhuyan et al., 2020); and the lower MPCE households spend a higher proportion of their income on ‘temptation goods’ such as tobacco and alcohol (Jumrani & Birthal, 2017). Among the regions, the central and eastern regions have recorded a remarkably higher prevalence of food insecurity, where one in every ten older adults is moderately or severely food insecure.
The oldest old are at a higher risk of being underweight, and young old are more likely to be overweight. This finding is in consonance with the findings of Boscatto et al., (2013). This result can be attributed to age-related muscle loss. The findings also show that there is a gender gap in the nutritional status of Indian older adults, with males being more likely to be underweight and females being more likely to be overweight. This finding agrees with the earlier research in Dehradun, India (Saxena et al., 2012), and in other countries such as Eastern Sudan (Omar et al., 2020), and Southern Brazil (Boscatto et al., 2013), but is not compatible with the findings of studies in Bangladesh (Alam et al., 2011), and Iran (Bakhshi et al., 2011). The high prevalence of overweight among females is believed to be due to less physical activity after retirement age and menopause-related weight gain. In contrast, older males are often involved in physical activities or engage in physical work. Similar to the findings of Gupta et al., (2018), we found the educational level of older adults is a most potent predictor of their nutritional status, i.e., educational level is negatively associated with underweight and positively with overweight. Higher risk of becoming overweight possibly due to better socioeconomic conditions and better access to food among the older adults with higher educational level (Ratnaprabha et al., 2015), accompanied by the sedentary lifestyle of the older adults with higher educational level. No significant association was established between working status and underweight. However, on the other hand, working older adults were more likely to be overweight. This link is difficult to explain, but we believe it exists because working older adults from economically well-off families mostly engage in jobs that require less physical activity; and older adults from low-income families are more likely to engage in physical activities that require a lot of energy. To get that energy, they often consume low-quality foods that are high in energy but also high in cholesterol and saturated fat. Consistent with the results of a previous study in Iran (Kaplan et al., 2003), our findings suggest that the prevalence of overweight is higher among older adults who were married or in a live-in relationship. Unlike a previous study in Iran (Bakhshi et al., 2011), our study found a significant association between marital status and nutritional status. While married and widowed older adults were more likely to be overweight, and the divorced/separated/deserted older adults were significantly more likely to be underweight; this finding is supported by a recent study in East Delhi, India (Vaish et al., 2020). Possible explanation for this observed difference lays in the fact that the dissolution of a marital union puts an individual at an increased risk of physical and psychological disorders (Kiecolt-Glaser & Newton, 2001), and not being in a marital union is linked to poorer levels of social support (Soulsby & Bennett, 2015); which are often associated with a higher risk of being undernourished among older adults (Kvamme et al., 2011).
In household characteristics, the place of residence plays a vital role in determining the nutritional status of older adults. The present study indicates that the prevalence of malnutrition among urban older adults is higher than their rural counterparts. The high prevalence of malnutrition (underweight + overweight) in urban areas may be attributed to the steady decline in underweight among rural older adults accompanied by a significant increment in the overweight population in urban areas. This is because India is shifting towards an overnourished from undernourished population due to the advancement in health and healthcare facilities and economic prosperity (Abraham et al., 2018), and this advancement is significantly higher in urban areas compared to the rural parts. Older adults from rural areas were more likely to be underweight, whereas urban older adults were at a higher risk being overweight, and a similar result was observed by Bakhshi et al., (2011). This discrepancy may be explained by the consumption of dietary fat and low physical activity(Pandey et al., 2013) in urban areas contributing to a rise in the proportion of overweight people, and in rural areas, the inadequate accessibility of food items because of their dependency on the food available in the local market, and hindrance in availing commodities due to inadequate transportation facilities (White et al., 2009). Despite India’s remarkable socioeconomic progress in recent decades, a large proportion of its older adult population was underweight, particularly those from poorer and poorest MPCE households. Older adults living in households of the richest MPCE were less likely to be underweight but significantly more likely to be overweight, indicating the prevailing economic disparity in the nutritional status of older adults. This finding is consistent with the finding of Alam et al., (2011), i.e., older adults from a higher SES had significantly higher BMI than their less well-off SES counterparts.
The region-wise prevalence of malnutrition indicates at least two in every five older adults were malnourished in all the regions. The regional disparity in malnutrition prevalence indicates a higher prevalence of underweight among older adults in the central and eastern regions, whereas overweight was more prevalent among older adults in the southern, northern, and western regions. Though older adults from north-eastern states have recorded a low prevalence of malnutrition, the prevalence of underweight is noticeably high. Similar to the findings of Sengupta et al., (2015), who found adult women from states located in the southern, northern, and western regions are more likely to be overweight, this study found older adults from these regions were at higher risk of being overweight, and older adults from central and eastern regions are at a higher risk of being underweight. This could be due to the fact that the southern, northern, and western regions are highly urbanized, and the eating habits, like increased intake of junk and fat-rich foods in urban settlements is a driving factor for being overweight, as well as the fruits and vegetable intake in the states are low (Kalaiselvi et al., 2016).
Conclusion
Most nutritional and food security intercession programmes are for infants, youngsters, teenagers, and pregnant and lactating mothers. Meanwhile, the food security, nourishment, and well-being of older adults are often overlooked. However, the increasing burden of malnutrition among older adults can lead to degenerative conditions and degradation of their quality of life, further affecting their caregivers’ overall well-being. Therefore, there is a need for time-to-time nutritional intervention for older adults; in addition to that, there is a need to set guidelines for underweight and overweight in the population of older adults, which can possibly help in treating or preventing the onset of underweight and obesity and checking its potential health risk in the later stage of life. It is also essential to create awareness among the oldest age groups and their carers about the quality, amount, and frequency of an older individual’s food intake. Furthermore, older adults from SC and ST communities, poor households, with no formal education, and older adults who are divorced/separated/deserted or never married need special policies and programmes focusing on increasing their access to affordable, healthy, and nutritious foods; because they are the most vulnerable groups in terms of both food insecurity and malnutrition. In addition to that, extensive studies are needed to point out state and region-specific factors associated with malnutrition among older adults, which can help in initiating important programmes and formulating various policies at state levels. Due to the cross-sectional nature of this study, even though a substantial association was discovered between food security and underweight among Indian older adults, no causation was demonstrated. Consequently, this study could be used as a baseline for a more thorough analytical investigation.
Data Availability
The data is provided by the IIPS, Mumbai upon submission of the detailed Data Assessment Request Form: https://www.iipsindia.ac.in/sites/default/files/LASI_DataRequestForm_0.pdf.
Code Availability
Not applicable.
References
Abdullah, A. (2015). The double burden of undernutrition and overnutrition in developing countries: an update. Current obesity reports, 4(3), 337–349. https://doi.org/10.1007/s13679-015-0170-y
Abraham, J., Johns, N. N., Aiyappan, F., Shibu, R. M. M., P., & Mathew, E. (2018). Nutritional status of older adults in a community in Pathanamthitta district of Kerala. International Journal of Research in Medical Sciences, 6(1), 210–215
Alam, M., Rahman, M., Flora, M., Karim, M., Sharif, M., & Ahmad, A. (2011). Household Food Security and Nutritional Status of Rural Elderly. Bangladesh Medical Journal, 40(3), 8–11
Amarya, S., Singh, K., & Sabharwal, M. (2015). Changes during aging and their association with malnutrition.Journal of Clinical Gerontology & Geriatrics,78–84
Arlappa, N., Balakrishna, N., Brahmam, G. N., & Vijayaraghavan, K. (2006). Nutritional Status of the Tribal Elderly in India. Journal of Nutrition for the Elderly, 25(2), 23–39. https://doi.org/10.1300/J052v25n02_03
Arnold, F., Parasuraman, S., Arokiasamy, P., & Kothari, M. (2009). Nutrition in India. National Family Health Survey (NFHS-3), India, 2005-06. Mumbai: International Institute for Population Sciences; Calverton, Maryland, USA: ICF Macro
Bakhshi, E., Seifi, B., Biglarian, A., & Mohammad, K. (2011). Factors associated with obesity in Iranian elderly people: Results from the National Health Survey. BMC research notes, 4(1), 1–6. https://doi.org/10.1186/1756-0500-4-538
Ballard, T. J., Kepple, A. W., & Cafiero, C. (2013). The food insecurity experience scale: development of a global standard for monitoring hunger worldwide. Rome: FAO. Retrieved from http://www.fao.org/economic/ess/ess-fs/voices/en/
Besora-Moreno, M., Llaurado, E., Tarro, L., & Sola, R. (2020). Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies. nutrients, 12(737), 1–16. https://doi.org/10.3390/nu12030737
Bhurosy, T., & Jeewon, R. (2014). Overweight and Obesity Epidemic in Developing Countries: A Problem with Diet, Physical Activity, or Socioeconomic Status? The Scientific World Journal, 1–7. https://doi.org/10.1155/2014/964236
Bhuyan, B., Sahoo, B. K., & Suar, D. (2020). Food insecurity dynamics in India: A synthetic panel approach. Social Sciences & Humanities Open, 2(1), 1–14. https://doi.org/10.1016/j.ssaho.2020.100029
Boscatto, E. C., Duarte, M., Coqueiro, R., & Barbosa, A. R. (2013). Nutritional status in the oldest elderly and associated factors. Revista da Associação Médica Brasileira, 59(1), 40–47
Bukunmi, A. A., & Jeremiah, C. O. (2018). Nutritional status, household food security and dietary diversity of the elderly residing in Ilaro, Ogun state, Nigeria. International Journal of Food Science and Nutrition, 3(6), 125–135
Caballero, B. (2007). The Global Epidemic of Obesity: An Overview. Epidemiologic Reviews, 29(1), 1–5. https://doi.org/10.1093/epirev/mxm012
Charlton, K. E., & Rose, D. (2001). Nutrition among Older Adults in Africa: the Situation at the Beginning of the Millenium. The Journal of Nutrition, 13(9), 2424S–2428S
Chinnakali, P., Upadhyay, R. P., Shokeen, D., Singh, K., Kaur, M., Singh, A. K., & Pandav, C. S. (2014). Prevalence of Household-level Food Insecurity and Its Determinants in an Urban Resettlement Colony in North India. Journal of Health Population and Nutrition, 32(2), 227–236
Dinour, L. M., Bergen, D., & Yeh, M. C. (2007). The Food Insecurity–Obesity Paradox: A Review of the Literature and the Role Food Stamps May Play. 107(11),1952–1961
FAO. (2017). The Food Insecurity Experience Scale: Measuring food insecurity through people ’ s experiences. Food and Agriculture Organization
FAO, IFAD, UNICEF, WFP, & WHO. (2021). The State of Food Security and Nutrition in the World 2021. Transforming food systems for food security, improved nutrition and affordable healthy diets for all. Rome: Food and Agriculture Organization. https://doi.org/10.4060/cb4474en
Gkiouras, K., Cheristanidis, S., Papailia, T. D., Grammatikopoulou, M. G., Karamitsios, N., Goulis, D. G., & Papamitsou, T. (2020). Malnutrition and Food Insecurity Might Pose a Double Burden for Older Adults. Nutrients, 12, 1–11. https://doi.org/10.3390/nu12082407
Grammatikopoulou, M. G., Gkiouras, K., Theodoridis, X., Tsisimiri, M., Markaki, A. G., Chourdakis, M., & Goulis, D. G. (2019). Food insecurity increases the risk of malnutrition among community dwelling older adults. Maturitas, 119, 8–13. https://doi.org/10.1016/j.maturitas.2018.10.009
Gupta, A., Kapil, U., Khandelwal, R., Khenduja, P., Sareen, N., Pandy, R. M., & Upadhyay, A. D. (2018). Prevalence and risk factors of underweight, overweight and obesity among a geriatric population living in a high-altitude region of rural Uttarakhand, India. Public Health Nutrition, 21(10), 1904–1911
Hosseinpour, S., Dorosty, A. R., & Djazayery, A. (2019). Association of Food Insecurity with Nutrition Status, Food Diversity and Anthropometric Status in Iranian Elderlies: A Cross-Sectional Study. Journal of Nutritional Sciences and Dietetics, 5(1), 26–31
IIPS, N. P. H. C. E., MoHFW, H. S. P. H., & USC. (2020). Longitudinal Ageing Study in India (LASI) Wave 1, 2017-18, India Report. Mumbai: International Institute for Population Sciences
Jumrani, J., & Birthal, P. S. (2017). Does consumption of tobacco and alcohol affect household food security? Evidence from rural India. Food Security, 9(1), 255–279. https://doi.org/10.1007/s12571-017-0660-8
Jung, S. E., Kim, S., Bishop, A., & Hermann, J. (2019). Poor Nutritional Status among Low-Income Older Adults: Examining the Interconnection between Self-Care Capacity, Food Insecurity, and Depression. Journal of the Academy of Nutrition and Dietetics, 119(10), 1687–1694. https://doi.org/10.1016/j.jand.2018.04.009
Kalaiselvi, S., Arjumand, Y., Jayalakshmy, R., Gomathi, R., Pruthu, T., & Palanivel, C. (2016). Prevalence of under-nutrition, associated factors and perceivednutritional status among elderly in a rural area of Puducherry, South India. Archives of Geronology and Geriatrics, 65, 156–160
Kaplan, M. S., Huguet, N., Newsom, J. T., McFarland, B. H., & Lindsay, J. (2003). Prevalence and Correlates of Overweight and Obesity Among Older Adults: Findings From the Canadian National Population Health Survey. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 58(11), M1018–M1030
Kapoor, S. K., & Anand, K. (2002). Nutritional transition: a public health challenge in developing countries. Journal of Epidemiology and Community Health, 56(11), 804–805
Keshari, P., & Shankar, H. (2021). Predictors and Inter-Linkage of Household and Individual Food Insecurity in Urban Geriatric Subjects: A Community based Study from India. Current Research in Nutrition and Food Science, 9(2), 639–652
Khole, C. V., & Soletti, A. (2018). Nutritional Status of Elderly in the Old Age Homes: A Study in Pune city. Current Research in Nutrition and Food Science, 6(1), 234–240
Kiecolt-Glaser, J. K., & Newton, T. L. (2001). Marriage and Health: His and Hers. Psychological Bulletin, 127(4), 472–503. https://doi.org/10.1037/0033-2909.127.4.472
Konda, S., P., R. K., & Giri, P. A. (2018). Prevalence of malnutrition and its determinants in an elderly people in South India. International Journal of Community Medicine and Public Health, 8, 3570–3576. https://doi.org/10.18203/2394-6040.ijcmph20183100
Krzyminska-Siemaszko, R., Deskur-Smielecka, E., ´zniak-Szymanowska, A. K., Kaczmarek, B., Kujawska-Danecka, H., Mossakowska, M., & Wieczorowska-Tobis, K. (2021). Socioeconomic Risk Factors of Poor Nutritional Status in Polish Elderly Population: The Results of PolSenior2 Study. Nutrients, 13(4388), 1–11. https://doi.org/10.3390/nu13124388
Kushwaha, S., Khanna, P., Srivastava, R., Jain, R., Singh, T., & Kiran, T. (2020). Estimates of malnutrition and risk of malnutrition among the elderly (≥ 60 years) in India: A systematic review and meta-analysis. Ageing Research Reviews, 63, 1–12. https://doi.org/10.1016/j.arr.2020.101137
Kvamme, J. M., Grønli, O., Florholmen, J., & Jacobsen, B. K. (2011). Risk of malnutrition is associated with mental health symptoms in community living elderly men and women: The Tromsø Study. Bmc Psychiatry, 11(112), 1–8. https://doi.org/10.1186/1471-244X-11-112
Lee, J., & Frongillo, E. A. Jr. (2001). Nutritional and Health Consequences Are Associated with Food Insecurity among U.S. Elderly Persons. The Journal of Nutrition, 131(5), 1503–1509
Letamo, G. (2020). Dual burden of underweight and overweight/obesity among adults in Botswana: prevalence, trends and sociodemographic correlates: A cross sectional survey. British Medical Journal Open, 10, 1–10
Lim, S. L., Ong, K. C., Chan, Y. H., Loke, W. C., Ferguson, M., & Daniels, L. (2012). Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clinical nutrition. Clinical Nutrition, 31(3), 345–350. https://doi.org/10.1016/j.clnu.2011.11.001
Miller, L. M., Tancredi, D. J., Kaiser, L. L., & Tseng, J. T. (2020). Midlife vulnerability and food insecurity: Findings from low-income adults in the US National Health Interview Survey. Plos One, 15(7), 1–14
Morales, M. E., & Berkowitz, S. A. (2016). The Relationship Between Food Insecurity, Dietary Patterns, and Obesity. Current Nutrition Reports, 5(1), 54–60. https://doi.org/10.1007/s13668-016-0153-y
NCD Risk Factor Collaboration. (2016). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. The Lancet, 387(10026), 1377–1396
Nord, M., Coleman-Jensen, A., Andrews, M., & Carlson, S. (2009). Household food security in the United States. US Department of Agriculture, Economic Research. Retrieved from http://www.ers.usda.gov/Publications/ERR108/ERR108.pdf
Omar, S. M., Taha, Z., Hassan, A. A., Al-Wutayd, O., & Adam, I. (2020). Prevalence and factors associated with overweight and central obesity among adults in the Eastern Sudan. Plos One, 15(4), 1–10
Pan, L., Sherry, B., Njai, R., & Blanck, H. M. (2012). Food Insecurity Is Associated with Obesity among US Adults in 12 States. Journal of the Academy of Nutrition and Dietetics, 112(9), 1403–1409
Pandey, R. M., Gupta, R., Misra, A., Misra, P., Singh, V., Agrawal, A., & Sharma, V. (2013). Determinants of urban–rural differences in cardiovascular risk factors in middle-aged women in India: A cross-sectional study. International Journal of Cardiology, 163(2), 157–162. https://doi.org/10.1016/j.ijcard.2011.06.008
Rajkamal, R., Singh, Z., Stalin, P., & Muthurajesh, E. (2015). Prevalence and determinants of overweight and obesity among elderly population in an urban area of Puducherry. International Journal of Medical Science and Public Health, 4(3), 1–4
Ratnaprabha, G., Farah, N., Twinkle, A., Naveen, J., & BX, A. (2015). Prevalence of Obesity and its Associated Factors among Elderly in a Rural Area of South Karnataka. Annals of Community Health, 2(3), 15–21
Russell, R. M. (2001). Factors in Aging that Effect the Bioavailability of Nutrients. The Journal of Nutrition, 131(4), 1359S–1361S
Saxena, A., Amin, A., Mohan, S. B., & Mohan, P. (2020). Food Insecurity in Tribal High Migration Communities in Rajasthan, India. Food and Nutrition Bulletin, 41(4), 513–518.
Saxena, V., Kandpal, S., Goel, D., & Bansal, S. (2012). Health status of elderly a community based study. Indian journal of community health, 24(4), 269–274
Schmidt, P., & Strauss, R. P. (1975). The Prediction of Occupation Using Multiple Logit Models. International Economic Review, 16(2), 471–486
Sengupta, A., Angeli, F., Syamala, T. S., Dagnelie, P. C., & Schayck, C. (2015). Overweight and obesity prevalence among Indian women by place of residence and socio-economic status: Contrasting patterns from ‘underweight states’ and ‘overweight states’ of India. Social Science & Medicine, 138(1), 161–169. https://doi.org/10.1016/j.socscimed.2015.06.004
Simsek, H., Meseri, R., Sahin, S., & Ucku, R. (2013). Prevalence of food insecurity and malnutrition, factors related to malnutrition in the elderly: A community-based, cross-sectional study from Turkey. European Geriatric Medicine, 4, 226–230. https://doi.org/10.1016/j.eurger.2013.06.001
Soulsby, L. K., & Bennett, K. M. (2015). Marriage and Psychological Wellbeing: The Role of Social Support. Psychology, 6(11), 1349. https://doi.org/10.4236/psych.2015.611132
Souza, B., & Marin-Leon, L. (2013). Food insecurity among the elderly: Cross-sectional study with soup kitchen users. Brazilian Journal of Nutrition, 26(6), 679–691
UN DESA/PD. (2019). World Population Prospects 2019. United Nations, Department of Economic and Social Affairs, Population Division
Vaish, K., Patra, S., & Chhabra, P. (2020). Nutritional Status among Elderly: A CommunityBased CrossSectional Study. Indian Journal of Public Health, 64(3), 266. https://doi.org/10.4103/ijph.IJPH_150_19
Vennu, V., Abdulrahman, T. A., & Bindawas, S. M. (2019). The Prevalence of Overweight, Obesity, Hypertension, and Diabetes in India: Analysis of the 2015–2016 National Family Health Survey. International Journal of Environmental Research and Public Health, 16(20), 1–22. https://doi.org/10.3390/ijerph16203987
Volkert, D., Kiesswetter, E., Cederholm, T., Donini, L. M., Eglseer, D., Norman, K., & Wirth, R. (2019). Development of a Model on Determinants of Malnutrition in Aged Persons: A MaNuEL Project. Gerontology and Geriatric Medicine, 5, 1–8. https://doi.org/10.1177/2333721419858438
White, A. M., Philogene, G. S., Fine, L., & Sinha, S. (2009). Social Support and Self-Reported Health Status of Older Adults in the United States. American Journal of Public Health, 99(10), 1872–1878
WHO. (2017). Evidence profile: malnutrition. World Health Organization
Acknowledgements
The authors are grateful to the Department of Humanities and Social Sciences, National Institute of Technology (NIT), Rourkela, for their support and encouragement, which helped improve this research paper.
Funding
No funds, grants, or other support was received from any funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors have substantially contributed to conducting the underlying research and drafting this manuscript. The contributions of the authors are as follows:
Binayak Kandapan
Conceptualization, Methodology, Formal analysis, Investigation, and Writing - original draft.
Itishree Pradhan
Writing - original draft, and Writing - Review & Editing,
Dr. Jalandhar Pradhan
Conceptualization, Writing - Review & Editing, and Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no potential competing interest with respect to the research, authorship and/or publication of this article.
Ethics approval
To reuse the Longitudinal Ageing Study in India (LASI), 2017-18 data, approval has been taken from the International Institute for Population Sciences (IIPS), Mumbai by submitting a data assessment request form.
Informed consent
As per ethics protocols, in the LASI, 2017-18 consent forms were administered to each household and age-eligible individual.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kandapan, B., Pradhan, I. & Pradhan, J. Food Insecurity and Malnutrition among Indian Older Adults: Findings from Longitudinal Ageing Study in India, 2017-18. Population Ageing 16, 639–659 (2023). https://doi.org/10.1007/s12062-022-09378-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12062-022-09378-2